Published online Dec 7, 2015. doi: 10.3748/wjg.v21.i45.12857
Peer-review started: March 30, 2015
First decision: May 18, 2015
Revised: May 22, 2015
Accepted: September 2, 2015
Article in press: September 2, 2015
Published online: December 7, 2015
AIM: To investigate the safety and feasibility of needlescopic grasper-assisted single-incision laparoscopic common bile duct exploration (nSIL-CBDE) by comparing the surgical outcomes of this technique with those of conventional laparoscopic CBDE (CL-CBDE).
METHODS: We retrospectively analyzed the clinical data of patients who underwent CL-CBDE or nSIL-CBDE for the treatment of common bile duct (CBD) stones between January 2000 and December 2014. For performing nSIL-CBDE, a needlescopic grasper was also inserted through a direct puncture below the right subcostal line after introducing a single-port through the umbilicus. The needlescopic grasper helped obtain the critical view of safety by retracting the gallbladder laterally and by preventing crossing or conflict between laparoscopic instruments. The gallbladder was then partially dissected from the liver bed and used for retraction. CBD stones were usually extracted through a longitudinal supraduodenal choledochotomy, mostly using flushing a copious amount of normal saline through a ureteral catheter. Afterward, for the certification of CBD clearance, CBDE was performed mostly using a flexible choledochoscope. The choledochotomy site was primarily closed without using a T-tube, and simultaneous cholecystectomies were performed.
RESULTS: During the study period, 40 patients underwent laparoscopic CBDE. Of these patients, 20 underwent CL-CBDE and 20 underwent nSIL-CBDE. The operative time for nSIL-CBDE was significantly longer than that for CL-CBDE (238 ± 76 min vs 192 ± 39 min, P = 0.007). The stone clearance rate was 100% (40/40) in both groups. Postoperatively, the nSIL-CBDE group required less intravenous analgesic (pethidine) (46.5 ± 63.5 mg/kg vs 92.5 ± 120.1 mg/kg, P = 0.010) and had a shorter hospital stay than the CL-CBDE group (3.8 ± 2.0 d vs 5.1 ± 1.7 d, P = 0.010). There was no significant difference in the incidence of postoperative complications between the two groups.
CONCLUSION: The results of this study suggest that nSIL-CBDE could be safe and feasible while improving cosmetic outcomes when performed by surgeons trained in conventional laparoscopic techniques.
Core tip: Though single-incision laparoscopic surgery has been applied in various fields worldwide, the reports on the single-incision laparoscopic common bile duct exploration (SIL-CBDE) are very limited, possibly due to technical difficulties. In this study, we were intended to overcome these difficulties by using additional 2-mm needlscopic grasper. This grasper is separately entered into the right abdomen by a puncture, and helps to form a stable trangulation with the transumbilically placed instruments. Our SIL-CBDE resulted in comparable surgical outcomes as conventional laparoscopic CBDE, indicating that the nSIL-CBDE is not only cosmetically acceptable but also provides both operative safety and feasibility.
- Citation: Kim SJ, Kim KH, An CH, Kim JS. Innovative technique of needlescopic grasper-assisted single-incision laparoscopic common bile duct exploration: A comparative study. World J Gastroenterol 2015; 21(45): 12857-12864
- URL: https://www.wjgnet.com/1007-9327/full/v21/i45/12857.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i45.12857
The introduction of single-incision laparoscopic surgery (SILS) has offered significant advantages to patients, including nearly scarless wounds and reduced wound morbidity[1-11] . In the same time, it has also increased the burden on surgeons because the entire operation is performed solely through one small incision. Accordingly, SILS is usually limited to operations in which the procedure is uncomplicated or less technically demanding[12-14]. Common bile duct exploration (CBDE) is a complicated surgery that includes a series of steps such as choledochoscopic lithotripsy and common bile duct (CBD) repair. Hence, reports on single-incision laparoscopic (SIL) CBDE are limited[15-17].
Recent advances in techniques and instruments have led to a progression of laparoscopic CBDE procedure. Moreover, current trends of no T-tube implementation during CBDE have further simplified the procedure[18-23]. Thus, these changes have opened wide the way for SIL-CBDE. Here, we describe needlescopic grasper-assisted single-incision CBDE (nSIL-CBDE). This technique is a modification of SIL-CBDE in order to reproduce the environment of laparoscopic CBDE by the addition of a very fine (2-mm) needlescopic grasper apart from the umbilical port. Simple addition of the needlescopic grasper to SIL-CBDE was expected to simultaneously enhance operative proficiency and minimize wound trauma. In this study, we aimed to demonstrate the safety and operative feasibility of nSIL-CBDE by comparing the surgical outcomes of nSIL-CBDE with those of conventional laparoscopic CBDE (CL-CBDE).
We performed a retrospective analysis of prospectively collected data from patients who underwent laparoscopic CBDE - either CL-CBDE or nSIL-CBDE - for stone(s) in the Department of Surgery, Uijeongbu St. Mary’s Hospital, College of Medicine, the Catholic University of Korea, between January 2000 and December 2014. The Ethics Committee at Uijeongbu St. Mary’s Hospital (IRB code: UC15RISI0027) approved the study. A total 40 laparoscopic CBDE procedures were performed during the study period.
Preoperatively, all the patients underwent ultrasonography, computed tomography, or magnetic resonance cholangiography. The inclusion criteria for CL-CBDE and nSIL-CBDE were identical and included all types of CBD stones that were estimated from preoperative evaluations, regardless of the severity of the inflammation or a history of abdominal laparotomy. In March 2012, we first performed nSIL-CBDE, and since then nSIL-CBDE was considered first for all the patients with CBD stone(s). The exclusion criteria for both CL-CBDE and nSIL-CBDE included CBD stone(s) combined with hepatolithiasis, lesion(s) suspected to be malignant, an American Society of Anesthesiologists (ASA) physical status classification of IV or V, severe medical conditions such as a recent history of myocardial infarction, and combined operation(s) outside the biliary tract. The total follow-up duration was 61.1 (6-171) mo.
The operative time was defined as the interval between the initial skin incision and the completion of wound closure as documented by the anesthesiologist. Open conversion was defined as completion of the operation with an incision for open surgery. In terms of postoperative complications, a minor bile leak was defined as bile drainage from the drain site prior to the seventh postoperative day that did not require radiological or operative interventions.
Under general anesthesia, patients were placed in the supine position, and the monitor was placed on the right-hand side of the patient, opposite the operating surgeon. In performing CL-CBDE, standard 4-port approach was utilized: one 10-mm infra-umbilical port for laparoscope, one 5-mm subxipholdal, one 5-mm right flank, and one 5-mm ports along the midclavicular line below the right subcostal region. After meticulous dissecting the Calot’s triangle, the critical view of safety was obtained. The cystic artery was clipped and divided, and then cystic duct was clipped. After making 5- to 10-mm vertical choledochotomy, CBD stone retrieval was attempted using a Stonebasket forcep (Olympus), Fogarty catheter, or triflange forceps (through a rigid nephroscope). To confirm the clearance of CBD, intraoperative cholangiography or flexible choledochoscopic exploration was performed. After CBD repairing, the gallbladder was completely removed from the liver, and trocar sites were repaired.
In performing nSIL-CBDE, a single, 25-mm vertical incision was made on the umbilicus and a dissection performed down to the peritoneum. Thereafter, a commercial single-port (SILSTM port; Covidien, Mansfield, MA) was then introduced through the umbilicus. The instruments used through the single port were a 5-mm grasper (Echicon Endosurgery, Cincinnati, OH), liver retractor (Snake retractor; Snowden Pencer, Tucker, GA), and laparoscope (Endoeye Flex 10 mm videoscope; Olympus, Tokyo, Japan). The grasper was replaced intermittently with a hook cautery and suction probe (Endopath Electrosurgery Probe Plus II; Echicon Endo-Surgery, Cincinnati, OH) for meticulous dissection. The snake retractor played a substantial role in achieving operative vision by pushing the hepatic hilum upwards in the direction of the cephalad. EndograbTM internal retractor (Virtual Ports, Misgav, Israel) was intermittently used to assist in obtaining optimal retraction of the liver.
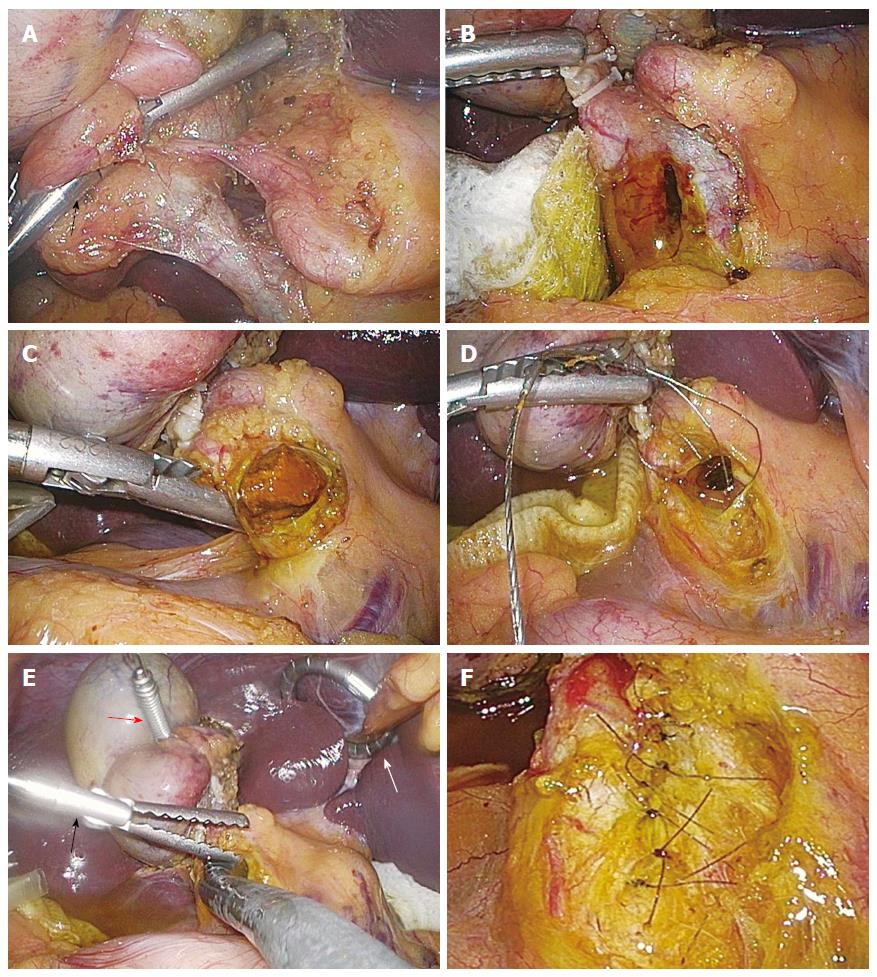
After abdominal insufflation, a needlescopic grasper (Minilap Grasper, Stryker, San Jose, CA or EndoRelief, Hirata Precision Co., Japan) was also inserted through a direct puncture below the right subcostal line along the right anterior axillary line (Figure 1). The needlescopic grasper helped obtain the critical view of safety (CVS)[24] by retracting the gallbladder laterally and by preventing crossing or conflict between laparoscopic instruments.
After dissection and identification of cystic artery and duct, they were ligated with 5-mm Hem-o-lok® clips (Weck Closure Systems, Research Triangle Park, NC), and then transected using laparoscopic scissors. The gallbladder was partially dissected from the liver bed and used for retraction. For CBD stone(s) retrieval, a longitudinal supraduodenal choledochotomy was made using an endoknife (Karl-Storz, Tuttlingen, Germany). Stones and debris from the CBD were extracted either by flushing a copious amount of normal saline through a ureteral catheter (3 - 5 French) or by using a Fogarty balloon catheter.
Afterwards, for the detection of residual CBD stone(s), CBDE was performed using a flexible choledochoscope (11-Fr, 30°; Karl-Storz). During choledochoscope manipulation (Figure 2), the needlescopic grasper effectively assisted the insertion of the choledochoscope into the CBD and changes in direction. It gently pushed the choledochoscope toward upper and lower part of the CBD to properly visualize both directions, enabling thorough visualization of both the upper (up to the right and left hepatic ducts) and lower (down to the papilla) portion of the CBD. Any residual stones were removed using a Stonebasket forcep or Fogarty catheter. In extracting residual stones, we selectively used a rigid nephroscope (17-Fr, 6°; Karl-Storz). It accommodates wide graspers, thereby making it possible to extract large stones under the direct vision. Therefore, it was commonly indicated at the time of failing to extract stones using stonebasket forcep or Fogarty catheter.
After CBD clearance, the choledochotomy site was primarily closed without using a T-tube. Initially, it was interruptedly repaired using a laparoscopic suturing device (Lap-suture®; Sejong Medical, Seoul, Korea). Lap-suture is a pre-knotted suturing material which enables convenient suturing just by suturing, passing the needle through the pre-knotted hole, and then tightening it by pushing using a bar. Thereafter, it was replaced with continuous suturing using an absorbable monofilament suture (PDS®6/0 Ethicon; Johnson and Johnson, Somerville, NJ). During intracorporeal suturing, the needlescopic grasper assisted a 5-mm straight needle holder (ENDOPATH Needle holder; Ethicon Endo-surgery) which had been entered via the transumbilical port.
We next dissected the gallbladder completely away from the liver. The resected gallbladder was placed in a specimen bag and was subsequently extracted from the abdomen through the umbilical wound. A Jackson-Pratt drain was placed in the subhepatic space, if necessary. After abdominal deflation, intraumbilical fascial defects and transumbilical skin incisions were closed with interrupted sutures.
Numeric data were presented as the mean and standard deviation or as the median and range. Continuous variables were analyzed using independent t-tests or Wilcoxon rank-sum tests. Categorical variables or proportions were compared using Pearson χ2 tests or Fisher exact tests when appropriate. Statistical analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago, IL). All P values were two-tailed. Statistical significance was accepted for P values < 0.05.
A total of 40 patients who underwent laparoscopic CBDE during the study period were included in this study. Of these patients, 20 (50%) underwent CL-CBDE and 20 (50%) underwent nSIL-CBDE. The mean patient age was 55.8 ± 18.7 (25-81) years. Male patients accounted for 45% (18/40) of the total patients in the study. The mean body mass index (BMI) was 23.8 ± 3.8 (17.2-34.8) kg/m2. Table 1 shows a summary of comparisons in patient demographics and preoperative clinical parameters. The two operative groups were similar in age, sex, and BMI. Laboratory and radiological variables were also comparable between the two groups. However, a comparison of the ASA classifications in the two groups revealed that patients with more severe conditions were included in the CL-CBDE group (P = 0.010).
| CL-LCBDE(n = 20) | nSIL-CBDE(n = 20) | P value | |
| Age (yr) | 51.0 ± 19.3 | 60.5 ± 17.2 | 0.068 |
| Male:female | 9:11 | 9:11 | |
| Body mass index (kg/m²) | 0.064 | ||
| mean ± SD | 25.00 ± 3.97 | 22.55 ± 2.69 | |
| median (range) | 25.10 (19.60-34.80) | 22.45 (17.16-27.69) | |
| ASA classification | 0.010 | ||
| 1 | 3 (15) | 10 (50) | |
| 2 | 15 (75) | 10 (50) | |
| 3 | 2 (10) | 0 (0) | |
| Comorbidity | 0.231 | ||
| CCI = 0 | 17 (85) | 20 (100) | |
| CCI ≥ 1 | 3 (15) | 0 (0) | |
| Previous abdominal surgery) | 4 (20) | 4 (20) | 1.000 |
| Laboratory parameters | |||
| Total leukocyte count (cells/mm3) | 9117 ± 3756 | 9123 ± 2569 | 0.274 |
| ALT (IL/dL) | 319 ± 267 | 215 ± 240 | 0.068 |
| Total bilirubin (mg/dL) | 3.71 ± 2.24 | 2.18 ± 2.02 | 0.079 |
| Alkaline phosphatase (IL/dL) | 610 ± 321 | 453 ± 342 | 0.069 |
| Radiological parameters | |||
| Gallbladder wall thickening (≥ 4 mm) | 4 (20) | 7 (35) | 0.480 |
| Acute cholangitis | 17 (85) | 14 (70) | 0.294 |
| CBD stone(s) | 1.000 | ||
| Definite | 18 (90) | 19 (95) | |
| Suspicious | 2 (10) | 1 (5) | |
| Indication of CBDE | 0.025 | ||
| Primary intervention | 7 (35) | 15 (75) | |
| Secondary intervention | 13 (65) | 5 (25) | |
| After ERCP failure | 7 (35) | 5 (25) | |
| Remnant CBD stone(s) after ERCP | 6 (30) | 0 (0) | |
| Admission route | 1.000 | ||
| ER | 12 (60) | 13 (65) | |
| OPD | 8 (40) | 7 (35) |
We classified the operative indications for laparoscopic CBDE into two categories: primary intervention and secondary intervention. The secondary intervention category was further subdivided into the inability or failure of therapeutic endoscopic retrograde cholangiopancreatography (ERCP) and remnant CBD stone(s) after ERCP attempt(s). We compared the operative indications between the two groups. CL-CBDE group included 37% (7/21) of patients with primary intervention, and nSIL-CBDE group included 75% (15/21) of patients with primary intervention (P = 0.025).
We next compared the operative results following CL-CBDE and nSIL-CBDE (Table 2). The operative time in the nSIL-CBDE group was significantly longer than that of the CL-CBDE group (238 ± 76 min vs 192 ± 39 min, P = 0.007). There was no significant difference in the estimated blood loss. The mean size and number of CBD stones that were retrieved were comparable. Successful retrievals of CBD stone(s) were reported in both groups, and there was no open conversion or addition of another port(s) during the procedure. Two methods were used to detect remnant stone(s) after CBD stone retrieval: completion cholangiography and completion choledochoscopy. All CL-CBDE patients, but not all nSIL-CBDE patients, underwent completion cholangiography (P = 0.018). Instead, all the nSIL-CBDE patients underwent completion choledochoscopy. In addition, Jackson-Pratt drains were less frequently placed in the nSIL-CBDE patients than in the CL-CBDE patients (15% vs 95.0%, P < 0.001).
| CL-LCBDE(n = 20) | nSIL-CBDE(n = 20) | P value | |
| Operative time (skin to skin, min) | 0.007 | ||
| mean ± SD | 192 ± 39 | 238 ± 76 | |
| median (range) | 197.5 (115-245) | 215.0 (125-365) | |
| Estimated blood loss (mL) | 132 ± 309 | 75 ± 161 | 0.101 |
| Completion cholangiogram | 5 (25) | 0 (0) | 0.018 |
| Completion choledochoscopy | 16 (80) | 20 (100) | 0.037 |
| Stone clearance | 20 (100) | 20 (100) | 1.000 |
| CBD stone | 0.348 | ||
| Single CBD stone | 12 (60) | 9 (45) | |
| Multiple CBD stones | 8 (40) | 11 (55) | |
| Mean number of CBD stone extracted | 1.9 ± 1.7 | 3.0 ± 3.2 | 0.316 |
| The largest diameter of CBD stone (mm) | 0.624 | ||
| mean ± SD | 12.3 ± 3.8 | 14.1 ± 4.6 | |
| median (range) | 14.0 (5.0-15.8) | 13.6 (7.0-20.0) | |
| Open conversion | 0 | 0 | 1.000 |
| Addition of another port | 0 | 0 | 1.000 |
| Gallbladder pathology | 0.234 | ||
| Gangrene/empyema | 1 (5) | 4 (20) | |
| Acute inflammation | 3 (15) | 3 (15) | |
| Chronic inflammation | 16 (80) | 13 (65) | |
| Drain placed | 19 (95) | 3 (15) | < 0.001 |
| Pethidine dose (mg/kg) | 92.5 ± 120.1 | 46.5 ± 63.5 | 0.010 |
| Postoperative hospital stay (d) | 0.010 | ||
| mean ± SD | 5.1 ± 1.7 | 3.8 ± 2.0 | |
| median (range) | 5.0 (2.0-8.0) | 3.0 (2.0-9.0) | |
| Postoperative complication | 0.275 | ||
| Infected subhepatic collection | 1 | 0 | |
| Minor bile leak | 0 | 1 | |
| Subhepatic seroma | 0 | 1 |
Postoperatively, the nSIL-CBDE group had lesser intravenous analgesic (pethidine) administration (46.5 ± 63.5 mg/kg vs 92.5 ± 120.1 mg/kg, P = 0.010) and shorter duration of hospitalization (3.8 ± 2.0 d vs 5.1 ± 1.7 d, P = 0.010). Postoperative complications were comparable between the two groups. Specifically, CL-CBDE group included one patient with infected subhepatic fluid collection, and nSIL-CBDE group included one patient with minor bile leak and the other patient with subhepatic hematoma.
To our best knowledge, this study was the first to compare CL-CBDE with nSIL-CBDE. Although nSIL-CBD increased the total operative time, it significantly reduced both intravenous analgesic administration and the length of hospital stay. The two groups were similar in other variables, including the CBD clearance rate, open conversion rate, and incidence of postoperative complications. Besides, nSIL-CBDE has intuitive advantages of cosmetic superiority and lessened wound morbidity. Therefore, we conclude that nSIL-CBDE is a reasonable alternative to CL-CBDE when performed by a surgeon with sufficient laparoscopic experience.
Patients prefer cosmesis and quality of life, as long as their safety is guaranteed[25]. nSIL-CBDE provides cosmetic superiority because it reproduces laparoscopic CBDE environment using the nearly scarless incisions. nSIL-CBDE exclusively leaves two trivial wounds; one is usually concealed in the umbilicus and the other is often negligible because it is made by a puncture of a 2-mm instrument. Moreover, though we could not detect possibly due to relatively small patient population, nSIL-CBDE is expected to reduce wound morbidity, as the number of port(s) is correlated with the number of the port-related complications, including trocar site hernia, and injury to the vessels, bowel, and other intra-abdominal organs[26-28]. Therefore, we believe that reducing the possibility of wound morbidity would be a major advantage of nSIL-CBDE.
Although SILS has been applied in various fields during the past two decades[11,12,29,30], technical difficulties has prevented widespread use of SIL-CBDE to the patients with CBD stone(s). However, as SILS experiences have been accumulated, the more refined surgical techniques and instruments have been overcoming the significant proportion of the technical difficulties. For instance, it has been considered challenging to appropriately manipulate the choledochoscope during SIL-CBDE. In nSIL-CBDE, however, this difficulty can be circumvented by the addition of a convenient guiding grasper which is aligned with the laparoscope in a triangular shape. Likewise, nSIL-CBDE provides a similar environment as CL-CBDE in terms of the handling of the choledochoscope.
CBD repair is one of the most challenging step during laparoscopic CBDE and has been performed with various techniques. The degree of difficulty is particularly increased when the T-tube is inserted into the CBD. However, data from a recent meta-analysis have provided evidence that primary closure instead of T-tube drainage is superior in terms of operative time, overall postoperative complications, and postoperative hospital stay associated with laparoscopic CBDE[31,32]. In our study, we performed primary closure in all patients who underwent laparoscopic CBDE. After retrieval of CBD stones, open CBD can be primarily closured by either interrupted or continuous sutures. We initially performed interrupted suturing using laparoscopic suture loops, but later changed to continuous sutures using 6.0 PDS. Recently, an increasing number of reports have described the use of continuous suturing, which is also supported by favorable long-term outcomes[18,19,22,33]. We think that although continuous suturing may initially result in increased operative time, with practice, it may actually shorten the total operative time.
We believe that nSIL-CBDE is particularly advantageous in CBD repair. During CL-CBDE, the needle holder, which is usually inserted through an epigastric port, reaches the CBD at an oblique angle. This alignment often hinders the stable performance of CBD repair. However, during nSIL-CBDE, the needle holder is inserted through the umbilicus and reaches the CBD nearly vertically, which allows comfortable suturing. We used two kinds of needlescopic graspers for assistance: the MinilapTM and EndoreliefTM graspers. While the MinilapTM has a 2-mm forceps, EndoreliefTM has a 5-mm forceps, enabling a grasping power equivalent to that of a 5-mm grasper. After a period of testing, we preferred to use the EndoreliefTM, because it provided an operative efficiency that was equivalent to that of the 5-mm grasper.
The nSIL-CBDE group had significantly longer operative times than the CL-CBDE group (237.8 ± 76.4 min vs 192.1 ± 39.0 min, P = 0.007). The most of nSIL-CBDE were performed during a learning period. Therefore, we expected that the operative times of nSIL-CBDE would be shorter once the learning curve was completed. In addition, although the series of nSIL-CBDE are our early experience, nSIL-CBDE significantly reduced the requirement for intravenous analgesic administration (P = 0.010) and the duration of hospitalization (P = 0.010). However, drain placement is one of the factors influencing postoperative pain[34], and nSIL-CBDE group lesser placed the drain (15% vs 95%, P < 0.001). Therefore, further investigation is required to determine whether or not nSIL-CBDE has the potential to reduce postoperative pain.
This study had several limitations. Because it was a retrospective study with a small sample size, future prospective randomized trials are required to definitively determine the efficacy and safety of nSIL-CBDE. In addition, the patient distribution was not completely balanced between the two groups. CL-CBDE group included more patients who had high ASA score (P = 0.010). However, it seems not to be substantial because no differences observed in the other variables reflecting degree of inflammation, such as the serum leukocyte count, total bilirubin level, and radiologic findings, between the two groups. Finally, there was a chronological difference between the two groups. A total series of nSIL-CBDE was followed by a series of CL-CBDE. Because both CL-CBDE and nSIL-CBDE are same laparoscopic surgery by nature, the nSIL-CBDE technique could be refined with accumulated experience. However, because most of the nSIL-CBDE were performed during its learning period, we think the comparable surgical outcomes of nSIL-CBDE demonstrate the operative feasibility of this technique.
In conclusion, although nSIL-CBDE increased the total operative time, it could maintain the critical view of safety throughout the procedure. nSIL-CBDE showed similar surgical outcomes as CL-CBDE, especially in the CBD clearance rate and the incidences of open conversion and postoperative complications. Moreover, nSIL-CBDE significantly reduced requirement of postoperative analgesics and length of the postoperative hospital stay. Therefore, we think nSIL-CBDE could provide both operative safety and feasibility while improving cosmetic outcomes.
Common bile duct exploration (CBDE) is a complicated surgery that includes a strenuous series of steps, including choledochoscopic lithotripsy and common bile duct (CBD) repair. Hence, reports on single-incision laparoscopic (SIL) CBDE are limited. The authors were intended to overcome these limitations by the addition of a very fine (2-mm) needlescopic grasper apart from the umbilical port.
In contrast to conventional laparoscopic CBDE which usually requires four incisions for trocar insertion, needlescopic grasper-assisted single-incision laparoscopic (nSIL) CBDE only requires one umbilical incision and a negligible 2-mm incision.
SIL-CBDE is very strenuous operation due to the difficulties provoked by the processes of choledochoscopic lithotripsy and common bile duct (CBD) repair. The results shows that simple addition of the needlescopic grasper to SIL-CBDE enhances operative proficiency while minimizing wound trauma. It was more facilitated by recent trends of primary CBD closure instead of T-tube drainage after CBDE.
Although CL-CBDE is a difficult operation, SIL-CBDE is even more difficult. nSIL-CBDE does not require the operator’s surgical skill enough to perform SIL-CBDE; only the surgical skill to perform CL-CBDE is sufficient. In addition, nSIL-CBDE seems to be accustomed within a relatively short learning curve. Therefore, nSIL-CBDE could be safe and feasible while improving cosmetic outcomes when performed by surgeons trained in conventional laparoscopic techniques.
This manuscript has novelty. This is the first study comparing needlescopic grasper-assisted single incision with conventional laparoscopic common bile duct exploration.
P- Reviewer: Kassir R, Wada H S- Editor: Yu J L- Editor: A E- Editor: Wang CH
| 1. | Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, Oh ST. The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg. 2011;254:933-940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 121] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 2. | Weiss HG, Brunner W, Biebl MO, Schirnhofer J, Pimpl K, Mittermair C, Obrist C, Brunner E, Hell T. Wound complications in 1145 consecutive transumbilical single-incision laparoscopic procedures. Ann Surg. 2014;259:89-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 3. | Ahmed K, Wang TT, Patel VM, Nagpal K, Clark J, Ali M, Deeba S, Ashrafian H, Darzi A, Athanasiou T. The role of single-incision laparoscopic surgery in abdominal and pelvic surgery: a systematic review. Surg Endosc. 2011;25:378-396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Asakuma M, Hayashi M, Komeda K, Shimizu T, Hirokawa F, Miyamoto Y, Okuda J, Tanigawa N. Impact of single-port cholecystectomy on postoperative pain. Br J Surg. 2011;98:991-995. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 5. | Chow A, Purkayastha S, Nehme J, Darzi LA, Paraskeva P. Single incision laparoscopic surgery for appendicectomy: a retrospective comparative analysis. Surg Endosc. 2010;24:2567-2574. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 6. | Hodgett SE, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS. Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg. 2009;13:188-192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 138] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 7. | Lee PC, Lo C, Lai PS, Chang JJ, Huang SJ, Lin MT, Lee PH. Randomized clinical trial of single-incision laparoscopic cholecystectomy versus minilaparoscopic cholecystectomy. Br J Surg. 2010;97:1007-1012. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 134] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 8. | Marks J, Tacchino R, Roberts K, Onders R, Denoto G, Paraskeva P, Rivas H, Soper N, Rosemurgy A, Shah S. Prospective randomized controlled trial of traditional laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy: report of preliminary data. Am J Surg. 2011;201:369-72; discussion 372-3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 144] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 9. | Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009;55:1198-1204. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 273] [Cited by in F6Publishing: 297] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 10. | Teixeira J, McGill K, Koshy N, McGinty J, Todd G. Laparoscopic single-site surgery for placement of adjustable gastric band--a series of 22 cases. Surg Obes Relat Dis. 2010;6:41-45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Vestweber B, Alfes A, Paul C, Haaf F, Vestweber KH. Single-incision laparoscopic surgery: a promising approach to sigmoidectomy for diverticular disease. Surg Endosc. 2010;24:3225-3228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Carus T. Current advances in single-port laparoscopic surgery. Langenbecks Arch Surg. 2013;398:925-929. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Goel R, Lomanto D. Controversies in single-port laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2012;22:380-382. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Kim SJ, Choi BJ, Lee SC. Overview of single-port laparoscopic surgery for colorectal cancers: past, present, and the future. World J Gastroenterol. 2014;20:997-1004. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 22] [Cited by in F6Publishing: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Chuang SH, Chen PH, Chang CM, Tsai YF, Lin CS. Single-incision laparoscopic common bile duct exploration with conventional instruments: an innovative technique and a comparative study. J Gastrointest Surg. 2014;18:737-743. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Shibao K, Higure A, Yamaguchi K. Laparoendoscopic single-site common bile duct exploration using the manual manipulator. Surg Endosc. 2013;27:3009-3015. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Yeo D, Mackay S, Martin D. Single-incision laparoscopic cholecystectomy with routine intraoperative cholangiography and common bile duct exploration via the umbilical port. Surg Endosc. 2012;26:1122-1127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Abellán Morcillo I, Qurashi K, Abrisqueta Carrión J, Martinez Isla A. Laparoscopic common bile duct exploration. Lessons learned after 200 cases. Cir Esp. 2014;92:341-347. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Decker G, Borie F, Millat B, Berthou JC, Deleuze A, Drouard F, Guillon F, Rodier JG, Fingerhut A. One hundred laparoscopic choledochotomies with primary closure of the common bile duct. Surg Endosc. 2003;17:12-18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Dong ZT, Wu GZ, Luo KL, Li JM. Primary closure after laparoscopic common bile duct exploration versus T-tube. J Surg Res. 2014;189:249-254. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 21. | Lee HM, Min SK, Lee HK. Long-term results of laparoscopic common bile duct exploration by choledochotomy for choledocholithiasis: 15-year experience from a single center. Ann Surg Treat Res. 2014;86:1-6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 53] [Article Influence: 5.3] [Reference Citation Analysis (2)] |
| 22. | Zhang HW, Chen YJ, Wu CH, Li WD. Laparoscopic common bile duct exploration with primary closure for management of choledocholithiasis: a retrospective analysis and comparison with conventional T-tube drainage. Am Surg. 2014;80:178-181. [PubMed] [Cited in This Article: ] |
| 23. | Zhou Y, Wu XD, Fan RG, Zhou GJ, Mu XM, Zha WZ, Jia J. Laparoscopic common bile duct exploration and primary closure of choledochotomy after failed endoscopic sphincterotomy. Int J Surg. 2014;12:645-648. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101-125. [PubMed] [Cited in This Article: ] |
| 25. | Varadarajulu S, Tamhane A, Drelichman ER. Patient perception of natural orifice transluminal endoscopic surgery as a technique for cholecystectomy. Gastrointest Endosc. 2008;67:854-860. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 98] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 26. | Rao PP, Rao PP, Bhagwat S. Single-incision laparoscopic surgery - current status and controversies. J Minim Access Surg. 2011;7:6-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 27. | Lowry PS, Moon TD, D’Alessandro A, Nakada SY. Symptomatic port-site hernia associated with a non-bladed trocar after laparoscopic live-donor nephrectomy. J Endourol. 2003;17:493-494. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 87] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 28. | Marcovici I. Significant abdominal wall hematoma from an umbilical port insertion. JSLS. 2001;5:293-295. [PubMed] [Cited in This Article: ] |
| 29. | Froghi F, Sodergren MH, Darzi A, Paraskeva P. Single-incision Laparoscopic Surgery (SILS) in general surgery: a review of current practice. Surg Laparosc Endosc Percutan Tech. 2010;20:191-204. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 30. | Greaves N, Nicholson J. Single incision laparoscopic surgery in general surgery: a review. Ann R Coll Surg Engl. 2011;93:437-440. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 31. | Wu X, Yang Y, Dong P, Gu J, Lu J, Li M, Mu J, Wu W, Yang J, Zhang L. Primary closure versus T-tube drainage in laparoscopic common bile duct exploration: a meta-analysis of randomized clinical trials. Langenbecks Arch Surg. 2012;397:909-916. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Yin Z, Xu K, Sun J, Zhang J, Xiao Z, Wang J, Niu H, Zhao Q, Lin S, Li Y. Is the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones is coming? A systematic review and meta-analysis. Ann Surg. 2013;257:54-66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 33. | Hua J, Lin S, Qian D, He Z, Zhang T, Song Z. Primary closure and rate of bile leak following laparoscopic common bile duct exploration via choledochotomy. Dig Surg. 2015;32:1-8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 34. | Eidy M, Jesmi F, Raygan F, Pishgahroudsari M, Pazouki A. Evaluating the Effect of Drain Site on Abdominal Pain after Laparoscopic Gastric Bypass Surgery for Morbid Obesity: A Randomized Controlled Trial. Bariatr Surg Pract Patient Care. 2015;10:38-41. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |