Published online Sep 21, 2015. doi: 10.3748/wjg.v21.i35.10242
Peer-review started: January 15, 2014
First decision: January 22, 2015
Revised: February 5, 2015
Accepted: April 3, 2015
Article in press: April 3, 2015
Published online: September 21, 2015
Unspecific abdominal complaints including bloating and irregular bowel movements may be caused by carbohydrate malabsorption syndromes, e.g., lactose and fructose malabsorption. These symptoms were investigated with hydrogen (H2) breath tests and correlated to carbohydrate malabsorption. During performing these H2-breath tests the patient presented with an acute, localized, non-migratory pain in the left lower abdominal quadrant. Primary epiploic appendagitis is a rare cause of abdominal acute or subacute complaints and diagnosis of primary epiploic appendagitis (PEA) is made when computed tomography reveals a characteristic lesion. We report on a patient with co-occurrence of lactose and fructose malabsorption, which was treated successfully with a diet free of culprit carbohydrates, with PEA recovering without medication or surgical treatment within few days. Since the abdominal unspecific symptoms had been present for months, they appeared not to be correlated to the acute localized abdominal pain, therefore we speculate on a random co-occurrence of combined carbohydrate malabsorption and PEA.
Core tip: The symptoms of unspecific abdominal complaints were investigated with hydrogen breath tests and correlated to lactose and fructose malabsorption. During performing these H2-breath tests the patient presented with an acute abdominal pain. Primary epiploic appendagitis (PEA) is a rare cause of abdominal acute complaints and diagnosis of PEA is made when computed tomography reveals a characteristic lesion. Since the abdominal unspecific symptoms had been present for months, they appeared not to be correlated to the acute localized abdominal pain, therefore we speculate on a random co-occurrence of combined carbohydrate malabsorption and PEA.
- Citation: Schnedl WJ, Kalmar P, Mangge H, Krause R, Wallner-Liebmann SJ. Co-occurrence of carbohydrate malabsorption and primary epiploic appendagitis. World J Gastroenterol 2015; 21(35): 10242-10245
- URL: https://www.wjgnet.com/1007-9327/full/v21/i35/10242.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i35.10242
Carbohydrate intolerance is frequently observed in patients with unspecific abdominal complaints including bloating and loose stools[1]. To evaluate symptoms we investigated digestive disorders including hydrogen (H2) breath tests in this patient and a combined carbohydrate, lactose and fructose, malabsorption was diagnosed. During evaluation acute abdominal pain occurred and a primary epiploic appendagitis (PEA) was demonstrated by computed tomography (CT). PEA is an uncommon, benign inflammatory process of epiploic appendages which are adipose structures protruding from the colon[2]. We report on a patient with co-occurrence of lactose and fructose malabsorption with PEA, who recovered with a diet free of culprit carbohydrates and without medication or surgical treatment within few days.
A 30-year-old male Caucasian patient presented for evaluation of postprandial epigastric discomfort, bloating, flatulence, frequent bowel movements and semisolid stools up to three times per day. Physical examination and an abdominal ultrasound revealed a meteoristic abdomen. The patient refused to undergo gastroscopy. A serum test for Helicobacter pylori demonstrated 23 U/mL (normal < 20). Antibodies against tissue transglutaminase were not found. In addition, hydrogen breath tests for lactose and fructose intolerance were performed. During breath tests with drinks containing 50 g lactose and a 25 g fructose load the exhalation of H2 was measured every 30 min for a period of 150 min. These tests demonstrated an increasing H2-value up to 32 parts per million (ppm) and 108 ppm, respectively. The diagnosis of lactose and fructose malabsorption was completed because H2 increased > 20 ppm in both tests. Dietary intervention showed improvement of symptoms and within few days of accurate lactose and fructose-free diet the patient’s epigastric complaints resolved.
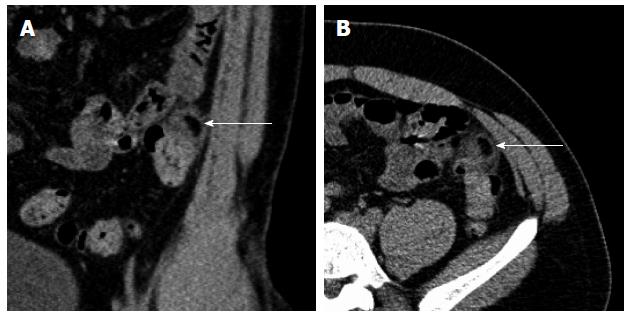
During performing these H2-breath tests the patient presented with an acute, dull, constant, localized, non-migratory, movement-intensifying pain in the left lower abdominal quadrant. An abdominal CT with intravenous contrast medium was performed and demonstrated an oval lesion, measuring 2.8 cm in maximum diameter, with a hyperattenuated rim, and surrounding fat stranding, located adjacent to the sigmoid colon. These findings of the inflamed and thickened visceral peritoneum surrounding the fat-containing appendage as hyperattenuating ring led to the diagnosis of PEA (Figure 1A and B). The count of leukocytes was 10.4 × 109/L (normal 4-10 × 109/L), and all other routine laboratory parameters, including C-reactive protein, erythrocyte sedimentation rate and liver enzymes, were within normal limits.
Within 6 d the patient’s localized pain caused by PEA resolved without therapy. For therapy of Helicobacter pylori positive gastritis a French triple therapy with pantoprazole, clarithromycin and amoxicillin was suggested. Further recovery was uneventful. After three months the patient was still symptom-free, therefore he refused further investigation concerning Helicobacter pylori infection. Written informed consent was obtained for all procedures, which were in accordance with the Declaration of Helsinki and the recommendations of the local Ethics Committee.
Carbohydrate malabsorption, mainly caused by fructose or lactose malabsorption, is used to describe disease conditions in which these carbohydrates, due to missing enzymes, are not broken down during gastrointestinal passage. In the small intestine, enzymes are aimed to hydrolyze carbohydrates into monosaccharides, which are absorbed by various carrier systems. Non-digested and/or -absorbed carbohydrates result in symptoms due to complete or incomplete bacterial metabolism of these carbohydrates in the colon. The clinical symptoms of carbohydrate malabsorption include flatulence, bloating, abdominal cramps and pain, diarrhea, and sometimes even headache, usually after the ingestion of a product containing culprit carbohydrates[1]. Carbohydrate malabsorption is frequent in patients with these unspecific gastrointestinal complaints and can cause gastrointestinal symptoms mimicking irritable bowel syndrome. Combined carbohydrate malabsorption with lactose and fructose malabsorption was recently demonstrated to occur in 25% of patients with carbohydrate malabsorption syndromes[3].
Due to the lack of pathognomonic clinical features and awareness, the diagnosis of PEA is difficult and rare. During the last few years with the introduction of cross-sectional imaging and the increasing use of abdominal CT scans for primary evaluation of abdominal pain, the recognition of PEA is increasing[4]. Appendices epiploicae are pouches of subserosal fat lining the entire length of the colon. PEA is thought to be a localized sterile inflammation in and surrounding one epiploic appendage, and to arise primarily from a torsion causing ischemia and infarction with aseptic fat necrosis, and spontaneous venous thrombosis. CT is the diagnostic modality of choice[5]. Symptoms mainly include acute and subacute non-migratory abdominal pain and local tenderness. This abdominal pain is usually dull, constant, non-migrating, and physical examination reveals a well-localized tenderness. Incidence of PEA is not known although most cases of PEA are described at the sigmoid colon[6]. It was suggested that patients treated for mild diverticulitis may have PEA and it was reported that up to 7% of all patients clinically suspected of having diverticulitis may have PEA[7].
Carbohydrate intolerance, e.g., lactose and fructose malabsorption, is frequently observed in patients with irregular bowel movements including bloating and loose stools. Although bowel habits are usually not disturbed in PAE a prevalence of carbohydrate malabsorption in PEA with up to 30% was suggested. A diet free of triggering carbohydrates in lactose and fructose malabsorption causes improvement of bloating and irregular bowel movements in a high percentage of patients. Since the abdominal unspecific symptoms were present for months, they appeared not to be correlated to the acute localized abdominal pain, which is present in most patients with PEA[2,7]. There is no indication that the H2-tests with high carbohydrate content may have caused PEA. Therefore we speculate on random co-occurrence of combined carbohydrate malabsorption and PEA. So far we know of only one case reported on carbohydrate (fructose) malabsorption and PEA[8].
In conclusion, symptoms as bloating and irregular bowel movements in patients may be due to carbohydrate malabsorption and can be treated effectively with a diet free of culprit carbohydrates. Recognition of acute and subacute non-migratory abdominal pain and appropriate diagnosis by CT allows diagnosis of PEA and usually an outpatient treatment without medication or surgery is successful within few days[9]. In patients with PEA we suggest investigation of carbohydrate malabsorption if unspecific abdominal symptoms including irregular bowel movements are additionally present besides the acute and subacute non-migratory abdominal pain.
Main symptoms were irregular bowel movements including flatulence, and bloating caused by carbohydrate malabsorption syndromes, and acute abdominal pain due to primary epiploic appendagitis (PEA).
Using breath tests with drinks containing 50 g lactose and 25 g fructose, combined lactose and fructose malabsorption, and PEA by computed tomography, were found.
For differential diagnosis of irregular bowel movements, celiac disease and Helicobacter pylori infection were also considered, and diverticulitis was excluded by abdominal computed tomography (CT).
Laboratory parameters were determined with slightly elevated leukocytes, but all other routine laboratory parameters were within normal limits.
Abdominal computed tomography scans are the method of choice for evaluation and recognition of PEA.
The diagnosis of lactose and fructose malabsorption was made because H2 increased > 20 ppm in both breath tests, and abdominal CT with intravenous contrast medium demonstrated an oval lesion located adjacent to the sigmoid colon.
Carbohydrate malabsorption can be treated effectively with a diet free of culprit carbohydrates and PEA treatment is usually successful without medication or surgery.
To the best knowledge of the authors, there exists only one report on carbohydrate (fructose) malabsorption and PEA.
This case report speculates on a random co-occurrence of combined carbohydrate malabsorption and PEA.
The paper reports on random co-occurrence of carbohydrate malabsorption syndrome and primary epiploic appendagitis. There is no indication that the H2-tests with high carbohydrate content may have caused PEA. However, the authors suggest investigation of carbohydrate malabsorption in patients with if unspecific abdominal symptoms including irregular bowel movements are additionally present besides the acute and subacute non-migratory abdominal pain of PEA.
P- Reviewer: Berg LK, Komericki P S- Editor: Yu J L- Editor: Wang TQ E- Editor: Wang CH
| 1. | Born P. Carbohydrate malabsorption in patients with non-specific abdominal complaints. World J Gastroenterol. 2007;13:5687-5691. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 25] [Cited by in F6Publishing: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Schnedl WJ, Krause R, Tafeit E, Tillich M, Lipp RW, Wallner-Liebmann SJ. Insights into epiploic appendagitis. Nat Rev Gastroenterol Hepatol. 2011;8:45-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Goebel-Stengel M, Stengel A, Schmidtmann M, Voort Iv, Kobelt P, Mönnikes H. Unclear abdominal discomfort: pivotal role of carbohydrate malabsorption. J Neurogastroenterol Motil. 2014;20:228-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Singh AK, Gervais DA, Hahn PF, Rhea J, Mueller PR. CT appearance of acute appendagitis. AJR Am J Roentgenol. 2004;183:1303-1307. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 107] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Ozdemir S, Gulpinar K, Leventoglu S, Uslu HY, Turkoz E, Ozcay N, Korkmaz A. Torsion of the primary epiploic appendagitis: a case series and review of the literature. Am J Surg. 2010;199:453-458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Vázquez GM, Manzotti ME, Alessandrini G, Lemos S, Perret MC, Catalano HN. [Primary epiploic appendagitis: clinical features in 73 cases]. Medicina (B Aires). 2014;74:448-450. [PubMed] [Cited in This Article: ] |
| 7. | Hwang JA, Kim SM, Song HJ, Lee YM, Moon KM, Moon CG, Koo HS, Song KH, Kim YS, Lee TH. Differential diagnosis of left-sided abdominal pain: primary epiploic appendagitis vs colonic diverticulitis. World J Gastroenterol. 2013;19:6842-6848. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 22] [Cited by in F6Publishing: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Schnedl WJ, Lipp RW, Wallner-Liebmann SJ, Kalmar P, Szolar DH, Mangge H. Primary epiploic appendagitis and fructose malabsorption. Eur J Clin Nutr. 2014;68:1359-1361. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Schnedl WJ, Krause R, Wallner-Liebmann SJ, Tafeit E, Mangge H, Tillich M. Primary epiploic appendagitis and successful outpatient management. Med Sci Monit. 2012;18:CS48-CS51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |