Published online Jan 21, 2015. doi: 10.3748/wjg.v21.i3.1024
Peer-review started: May 4, 2014
First decision: June 27, 2014
Revised: July 6, 2014
Accepted: July 30, 2014
Article in press: July 30, 2014
Published online: January 21, 2015
Obscure gastrointestinal bleeding is an uncommonly encountered and difficult-to-treat clinical problem in gastroenterology, but advancements in endoscopic and radiologic imaging modalities allow for greater accuracy in diagnosing obscure gastrointestinal bleeding. Ectopic varices account for less than 5% of all variceal bleeding cases, and jejunal variceal bleeding due to extrahepatic portal hypertension is rare. We present a 47-year-old man suffering from obscure gastrointestinal bleeding. Computed tomography of the abdomen revealed multiple vascular tufts around the proximal jejunum but no evidence of cirrhosis, and a visible hypodense filling defect suggestive of thrombus was visible in the superior mesenteric vein. Enteroscopy revealed several serpiginous varices in the proximal jejunum. Serologic data disclosed protein C deficiency (33.6%). The patient was successfully treated by therapeutic balloon-assisted enteroscopy and long-term anticoagulant therapy, which is normally contraindicated in patients with gastrointestinal bleeding. Diagnostic modalities for obscure gastrointestinal bleeding, such as capsule endoscopy, computed tomography enterography, magnetic resonance enterography, and enteroscopy, were also reviewed in this article.
Core tip: This article presents a rare case of obscure gastrointestinal bleeding-jejunal variceal bleeding and superior mesenteric venous thrombosis. The variceal bleeding and superior mesenteric venous thrombosis were secondary to protein C deficiency. It is worth mentioning that the bleeding was controlled under anticoagulant therapy after therapeutic enteroscopy.
- Citation: Hsu WF, Tsang YM, Teng CJ, Chung CS. Protein C deficiency related obscure gastrointestinal bleeding treated by enteroscopy and anticoagulant therapy. World J Gastroenterol 2015; 21(3): 1024-1027
- URL: https://www.wjgnet.com/1007-9327/full/v21/i3/1024.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i3.1024
Recent advancements in endoscopic and radiologic imaging modalities allow for greater accuracy in diagnosing obscure gastrointestinal bleeding (OGIB), an uncommonly encountered and difficult-to-treat clinical problem in gastroenterology[1]. Ectopic varices, which comprise large portosystemic venous collaterals located anywhere other than the gastroesophageal region[2], account for less than 5% of all variceal bleeding cases[3] and usually are due to previous abdominal surgery, intrahepatic portal hypertension, and rarely extrahepatic causes[4]. We present a case of thrombosis in the superior mesenteric vein (SMV) complicated by jejunal variceal bleeding secondary to protein C deficiency. OGIB was successfully treated by balloon-assisted enteroscopy and anticoagulant therapy.
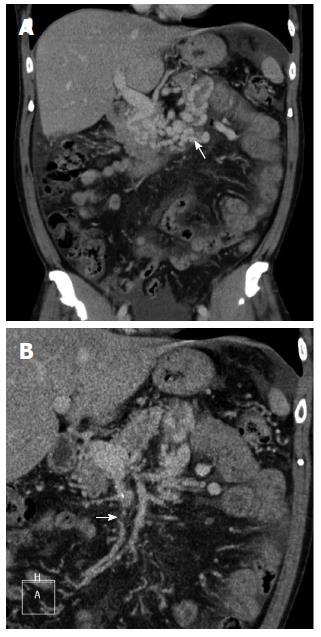
A 47-year-old man presented with a 10-d history of tarry stool passage. The patient had no other underlying disease. Results of physical examinations were unremarkable with the exception of pale conjunctiva. Laboratory studies revealed a hemoglobin level of 6.9 g/dL (normal range: 13-17 g/dL), a platelet count of 200 × 103/μL (normal range, 140-400 × 103/μL), an international normalized ratio (INR) of prothrombin time of 1.01, an activated partial thromboplastin time of 26.8 s (normal range: 23.3-39.3 s), and normal aminotransferase levels. Esophagogastroduodenoscopic and colonoscopic examinations revealed no evidence of stigmata of recent hemorrhage. The preliminary diagnosis was OGIB. Computed tomography (CT) of the abdomen revealed multiple vascular tufts around the proximal jejunum but no evidence of cirrhosis (Figure 1A). A hypodense filling defect suggestive of thrombus was visible in the SMV (Figure 1B). Celiac angiography revealed engorged collateral veins in the left upper quadrant of the abdomen without contrast agent in the main trunk of the SMV (Figure 2). Antegrade single-balloon enteroscopy (SIF-Q260; Olympus Medical systems, Tokyo, Japan) revealed several serpiginous varicose veins (Figure 3) with poor distensibility of the proximal jejunum. A mixture of 0.5 mL N-butyl-2-cyanoacrylate and 0.5 mL lipioidol was endoscopically injected into said veins. Serologic data disclosed protein C deficiency (33.6%). Anti-smooth muscle antibody, antinuclear antibody, anti-cardiolipin antibody, homocysteine, antithrombin III, and tumor markers were all within normal limits. The patient was therefore placed on oral warfarin therapy (INR 2.0), and he lived uneventfully 17 mo after the enteroscopy.
Variceal bleeding due to portal hypertension developing in locations other than the esophagus and stomach accounts for less than 5% of all variceal bleeding cases[3]. Jejunal variceal bleeding due to extrahepatic portal hypertension is rare. Small intestinal varices normally present as melena or hematochezia[5]. Bleeding from chronic mesenteric thrombosis is a rare cause of OGIB and without prompt diagnosis it can result in death[6].
Diagnosis of small bowel disorders is challenging because of the small intestine’s length (about 6 to 7 m), mobility, and tortuosity. With the development of diagnostic modalities, such as capsule endoscopy[7], CT enterography (CTE)[8], and magnetic resonance enterography (MRE)[9], correct and timely diagnosis of small intestinal lesions can be achieved without unnecessary surgical intervention in some cases. Capsule endoscopy not only has the advantage of non-invasiveness but also has a high sensitivity and high negative predictive value in predicting rebleeding in patients with OGIB[7]. However, the diagnostic specificity of capsule endoscopy is a concern, because 13% of asymptomatic persons may have minor lesions that are not detected by capsule endoscopic evaluation. In addition, capsule endoscopy cannot be performed with therapeutic intents or in patients with certain contraindications, such as gastrointestinal obstruction, pregnancy, or swallowing difficulty[10]. CTE and MRE are useful methods for detecting small inflammatory and hypervascular lesions in the small intestine[8,9]. Limitations of enterography include exposure to radiation, the need for large volumes of oral contrast agents, adverse reactions to contrast agents (e.g., contrast allergy), and the risk of developing contrast-induced nephropathy[11]. Deep small-bowel enteroscopy can be used to simultaneously detect and treat lesions as well as take biopsy specimens for pathologic analysis[12]; however, the technique requires years of experience to perform and is associated with rare complications, including pancreatitis and perforation[13,14]. Diagnosis and treatment of OGIB could be dramatically improved by adequately combining two or more of the modalities. In our institute we routinely perform second-look upper and lower endoscopy for patients with OGIB, as recommended by a number of clinical guidelines[1,15]. If the second-look endoscopy reveals negative findings, antegrade or retrograde single-balloon enteroscopy guided by capsule endoscopy or CT images is performed.
Small intestinal ectopic varices normally present as tortuous collateral vessels in the mesenteric side of the small intestine on abdominal images[16,17]. Angiographic findings characteristic of OGIB include prolonged contrast agent retention in the collateral vascular tufts[18,19], while endoscopic findings include a spherical bulge, localized prominence, and nodular or serpinginous varices[20,21]. These image findings were identified in our patient. As shown in this and in previous reports, jejunal variceal bleeding can be treated by injecting N-butyl-2-cyanoacrylate under enteroscopy[22]. Radiographic embolization via feeding venous occlusions has been suggested in acute settings[23]. Surgery is only recommended for patients without liver cirrhosis or for patients with compensated liver cirrhosis and extrahepatic portal vein thrombosis[24].
Protein C is a vitamin K-dependent anticoagulant protein that inactivates coagulation factors Va and VIIIa, and its deficiency (< 55%) results in a thrombophilic state[25]. Long-term oral anticoagulants at an INR of 2 to 3 have been shown to be effective in preventing thrombosis in patients with protein C deficiency[25].
In conclusion, OGIB is an uncommonly encountered and difficult-to-treat clinical problem in gastroenterology; however, recent advancements in imaging modalities have greatly enhanced diagnosis and treatment. Ectopic variceal bleeding should be considered in patients with OGIB, and small intestinal variceal bleeding secondary to thrombophilia can be managed by balloon-assisted enteroscopy and anticoagulant therapy.
A 47-year-old man presented with a 10-d history of tarry stool passage.
Esophagogastroduodenoscopic and colonoscopic examinations revealed no evidence of stigmata of recent hemorrhage, and the preliminary diagnosis was obscure gastrointestinal bleeding.
Common differential diagnoses of obscure gastrointestinal bleeding include angiodysplasia, small bowel Crohn’s disease, small bowel tumors, intestinal infections (such as tuberculosis and parasites), nonspecific intestinal ulcers, and variceal bleeding.
HGB 6.9 gm/dL; platelet count of 200 × 103/μL; PT INR 1.01; aPTT 26.8 s; Serologic data disclosed a protein C level of 33.6%.
Abdominal computed tomography revealed multiple vascular tufts around the proximal jejunum with a hypodense filling defect in the superior mesenteric vein, and antegrade single-balloon enteroscopy revealed several serpiginous varicose veins in the proximal jejunum.
No pathological diagnosis in this article.
A mixture of 0.5 mL N-butyl-2-cyanoacrylate and 0.5 mL lipioidol was endoscopically injected into varices, and the patient was placed on long-term oral warfarin therapy (PT INR 2.0).
Ectopic varices account for less than 5% of all variceal bleeding cases, and jejunal variceal bleeding due to superior mesenteric venous thrombosis and protein C deficiency is rare.
Protein C is a vitamin K-dependent anticoagulant protein that inactivates coagulation factors Va and VIIIa, and its deficiency (< 55%) results in a thrombophilic state.
This case report reminds us that the cause of jejunal varices should be carefully evaluated, and small intestinal variceal bleeding secondary to thrombophilia can be managed by balloon-assisted enteroscopy and anticoagulant therapy.
Although single-balloon enteroscopy with N-butyl-2-cyanoacrylate and lipioidol injection for varicose veins had been reported before, it was a rare circumstance that the jejunal varices came from superior mesenteric venous thrombosis and protein C deficiency.
P- Reviewer: Dina I, Lin HC, Wang SJ S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Zhang DN
| 1. | Dye CE, Gaffney RR, Dykes TM, Moyer MT. Endoscopic and radiographic evaluation of the small bowel in 2012. Am J Med. 2012;125:1228.e1-1228.e12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Lebrec D. Ectopic varices in patients with portal hypertension. Arch Surg. 1980;115:890. [PubMed] [Cited in This Article: ] |
| 3. | Kinkhabwala M, Mousavi A, Iyer S, Adamsons R. Bleeding ileal varicosity demonstrated by transhepatic portography. AJR Am J Roentgenol. 1977;129:514-516. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 54] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Lebrec D, Benhamou JP. Ectopic varices in portal hypertension. Clin Gastroenterol. 1985;14:105-121. [PubMed] [Cited in This Article: ] |
| 5. | Khan AA, Sarwar S, Alam A, Butt AK, Shafqat F, Tarique S, Ahmed I, Alvi A, Niazi A. Ectopic intestinal varices as a rare cause of lower gastrointestinal haemorrhage. J Coll Physicians Surg Pak. 2003;13:526-527. [PubMed] [Cited in This Article: ] |
| 6. | Soper NJ, Rikkers LF, Miller FJ. Gastrointestinal hemorrhage associated with chronic mesenteric venous occlusion. Gastroenterology. 1985;88:1964-1967. [PubMed] [Cited in This Article: ] |
| 7. | Lai LH, Wong GL, Chow DK, Lau JY, Sung JJ, Leung WK. Long-term follow-up of patients with obscure gastrointestinal bleeding after negative capsule endoscopy. Am J Gastroenterol. 2006;101:1224-1228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 122] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Fletcher JG, Huprich J, Loftus EV, Bruining DH, Fidler JL. Computerized tomography enterography and its role in small-bowel imaging. Clin Gastroenterol Hepatol. 2008;6:283-289. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Masselli G, Vecchioli A, Gualdi GF. Crohn disease of the small bowel: MR enteroclysis versus conventional enteroclysis. Abdom Imaging. 2006;31:400-409. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Goldstein JL, Eisen GM, Lewis B, Gralnek IM, Zlotnick S, Fort JG. Video capsule endoscopy to prospectively assess small bowel injury with celecoxib, naproxen plus omeprazole, and placebo. Clin Gastroenterol Hepatol. 2005;3:133-141. [PubMed] [Cited in This Article: ] |
| 11. | Graça BM, Freire PA, Brito JB, Ilharco JM, Carvalheiro VM, Caseiro-Alves F. Gastroenterologic and radiologic approach to obscure gastrointestinal bleeding: how, why, and when? Radiographics. 2010;30:235-252. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Pasha SF, Hara AK, Leighton JA. Diagnostic evaluation and management of obscure gastrointestinal bleeding: a changing paradigm. Gastroenterol Hepatol (N Y). 2009;5:839-850. [PubMed] [Cited in This Article: ] |
| 13. | Mehdizadeh S, Ross A, Gerson L, Leighton J, Chen A, Schembre D, Chen G, Semrad C, Kamal A, Harrison EM. What is the learning curve associated with double-balloon enteroscopy? Technical details and early experience in 6 U.S. tertiary care centers. Gastrointest Endosc. 2006;64:740-750. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 201] [Cited by in F6Publishing: 214] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 14. | May A, Nachbar L, Pohl J, Ell C. Endoscopic interventions in the small bowel using double balloon enteroscopy: feasibility and limitations. Am J Gastroenterol. 2007;102:527-535. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 168] [Cited by in F6Publishing: 166] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 15. | Raju GS, Gerson L, Das A, Lewis B. American Gastroenterological Association (AGA) Institute technical review on obscure gastrointestinal bleeding. Gastroenterology. 2007;133:1697-1717. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 379] [Cited by in F6Publishing: 404] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 16. | Lee JY, Song SY, Kim J, Koh BH, Kim Y, Jeong WK, Kim MY. Percutaneous transsplenic embolization of jejunal varices in a patient with liver cirrhosis: a case report. Abdom Imaging. 2013;38:52-55. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Seeger M, Günther R, Hinrichsen H, Both M, Helwig U, Arlt A, Stelck B, Bräsen JH, Sipos B, Schafmayer C. Chronic portal vein thrombosis: transcapsular hepatic collateral vessels and communicating ectopic varices. Radiology. 2010;257:568-578. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Menu Y, Gayet B, Nahum H. Bleeding duodenal varices: diagnosis and treatment by percutaneous portography and transcatheter embolization. Gastrointest Radiol. 1987;12:111-113. [PubMed] [Cited in This Article: ] |
| 19. | Weishaupt D, Pfammatter T, Hilfiker PR, Wolfensberger U, Marincek B. Detecting bleeding duodenal varices with multislice helical CT. AJR Am J Roentgenol. 2002;178:399-401. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Soga K, Tomikashi K, Miyawaki K, Okuda K, Sugiyama Y, Sekikawa S, Wakabayashi N, Konishi H, Mitsufuji S, Kataoka K. Endoscopic injection sclerotherapy with ethanolamine oleate with iopamidol for esophagojejunal varices in idiopathic portal hypertension. Dig Dis Sci. 2009;54:1592-1596. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Almadi MA, Almessabi A, Wong P, Ghali PM, Barkun A. Ectopic varices. Gastrointest Endosc. 2011;74:380-388. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Gubler C, Glenck M, Pfammatter T, Bauerfeind P. Successful treatment of anastomotic jejunal varices with N-butyl-2-cyanoacrylate (Histoacryl): single-center experience. Endoscopy. 2012;44:776-779. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Smith-Laing G, Scott J, Long RG, Dick R, Sherlock S. Role of percutaneous transhepatic obliteration of varices in the management of hemorrhage from gastroesophageal varices. Gastroenterology. 1981;80:1031-1036. [PubMed] [Cited in This Article: ] |
| 24. | Norton ID, Andrews JC, Kamath PS. Management of ectopic varices. Hepatology. 1998;28:1154-1158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 239] [Cited by in F6Publishing: 264] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 25. | Dahlbäck B. Advances in understanding pathogenic mechanisms of thrombophilic disorders. Blood. 2008;112:19-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 215] [Cited by in F6Publishing: 201] [Article Influence: 12.6] [Reference Citation Analysis (0)] |