Published online Jun 28, 2015. doi: 10.3748/wjg.v21.i24.7558
Peer-review started: November 22, 2014
First decision: December 11, 2014
Revised: January 17, 2015
Accepted: February 11, 2015
Article in press: February 11, 2015
Published online: June 28, 2015
Processing time: 219 Days and 21.2 Hours
AIM: To examine whether muscle training with an oral IQoroR screen (IQS) improves esophageal dysphagia and reflux symptoms.
METHODS: A total of 43 adult patients (21 women and 22 men) were consecutively referred to a swallowing center for the treatment and investigation of long-lasting nonstenotic esophageal dysphagia. Hiatal hernia was confirmed by radiologic examination in 21 patients before enrollment in the study (group A; median age 52 years, range: 19-85 years). No hiatal hernia was detected by radiologic examination in the remaining 22 patients (group B; median age 57 years, range: 22-85 years). Before and after training with an oral IQS for 6-8 mo, the patients were evaluated using a symptom questionnaire (esophageal dysphagia and acid chest symptoms; score 0-3), visual analogue scale (ability to swallow food: score 0-100), lip force test (≥ 15 N), velopharyngeal closure test (≥ 10 s), orofacial motor tests, and an oral sensory test. Another twelve patients (median age 53 years, range: 22-68 years) with hiatal hernia were evaluated using oral IQS traction maneuvers with pressure recordings of the upper esophageal sphincter and hiatus canal as assessed by high-resolution manometry.
RESULTS: Esophageal dysphagia was present in all 43 patients at entry, and 98% of patients showed improvement after IQS training [mean score (range): 2.5 (1-3) vs 0.9 (0-2), P < 0.001]. Symptoms of reflux were reported before training in 86% of the patients who showed improvement at follow-up [1.7 (0-3) vs 0.5 (0-2), P < 0.001). The visual analogue scale scores were classified as pathologic in all 43 patients, and 100% showed improvement after IQS training [71 (30-100) vs 22 (0-50), P < 0.001]. No significant difference in symptom frequency was found between groups A and B before or after IQS training. The lip force test [31 N (12-80 N) vs 54 N (27-116), P < 0.001] and velopharyngeal closure test values [28 s (5-74 s) vs 34 s (13-80 s), P < 0.001] were significantly higher after IQS training. The oral IQS traction results showed an increase in mean pressure in the diaphragmatic hiatus region from 0 mmHg at rest (range: 0-0 mmHG) to 65 mmHg (range: 20-100 mmHg).
CONCLUSION: Oral IQS training can relieve/improve esophageal dysphagia and reflux symptoms in adults, likely due to improved hiatal competence.
Core tip: Oropharyngeal dysphagia can be improved by training with an IQoroR screen (IQS). The present study investigated whether IQS training may improve esophageal dysphagia (ED) in a similar manner as surgical repair of a hiatal hernia. Forty-three patients with longstanding ED and reflux symptoms, which were not relieved by treatment with proton pump inhibitors, received IQS training three times daily for six months; all showed increased diaphragm hiatus pressure. ED improved in 42 patients and reflux symptoms improved in 36. IQS training can be a valuable alternative to surgery with restoration of hiatal competence in patients with ED and reflux symptoms.
- Citation: Hägg M, Tibbling L, Franzén T. Esophageal dysphagia and reflux symptoms before and after oral IQoroR training. World J Gastroenterol 2015; 21(24): 7558-7562
- URL: https://www.wjgnet.com/1007-9327/full/v21/i24/7558.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i24.7558
Long-lasting oropharyngeal dysphagia can be successfully treated with oral IQoroR screen (IQS) training[1,2]. Because IQS training involves the entire buccinator mechanism[3,4], the upper esophageal sphincter (UES), and contraction of the diaphragm, it was hypothesized that oral IQS training would also make the hiatus canal more resistant against a pressure load from below, and thereby prevent sliding of a hernia and gastroesophageal reflux. The present study investigated whether esophageal dysphagia (intermittent blocking sensation in the chest at meals) and reflux symptoms can be improved or eliminated by oral IQS training in adult patients.
This study was a prospective therapeutic and clinical study describing the effects of IQS training on esophageal dysphagia and reflux symptoms.
A total of 43 adult patients (21 women and 22 men) were consecutively referred to a swallowing center for oral IQS training[1,2] and evaluation of esophageal dysphagia of a nonstenotic character for a median period of 3 years (range: 1-15 years). Gastroesophageal radiology was performed with barium swallows in the upright position in all patients to exclude stenosis as a cause for dysphagia before enrollment in the study. Hiatal hernia was present in 21 patients (group A; median age 52 years, range: 19-85 years, 13 women, 8 men) but not in the remaining 22 patients (group B; median age 57 years, range: 22-85 years, 8 women, 14 men). All patients had received proton pump inhibitor (PPI) medication for > 1 year without any effect on their dysphagia or reflux symptoms. However, the patients were not asked to withdraw their PPI medication during the study period. Patients with neurologic diseases were excluded. This prospective clinical study was performed during 2013-2014.
At baseline and after the training period, the patients completed a symptom questionnaire regarding symptoms of hiatal incompetence (a blocking feeling in the chest at meals, acid feeling in the chest, or acid regurgitation), which was scored from 0 to 3 (0 = no, 1 = slight, 2 = moderate, 3 = severe)[5], and a visual analogue scale[2] regarding their ability to swallow food was scored from 0 to 100 mm (0 = normal, 100 = total inability). Different orofacial motor tests[6] and oral sensory tests[7] were performed in order to exclude dysphagia of central nervous system origin. On both occasions, a lip force test[8,9] and velopharyngeal closure test[10] were performed to confirm normal oropharyngeal function and training compliance. The training effect was investigated after 6-8 mo; however, all patients were contacted by telephone or in the clinic two or three times before follow-up to verify training compliance. Another twelve patients with hiatal hernia (median age 53 years, range: 22-68 years), as assessed by radiology and endoscopy, were investigated at an esophageal laboratory in the sitting and recumbent positions using esophageal high-resolution manometry (HRM)[11] to determine if oral IQS traction increased the diaphragmatic pressure in the hiatus canal.
IQS traction was measured by esophageal HRM[11], with special attention given to the pressure in the UES (normal resting pressure > 30 mmHg) and the diaphragmatic hiatus (normal resting pressure 10-35 mmHg).
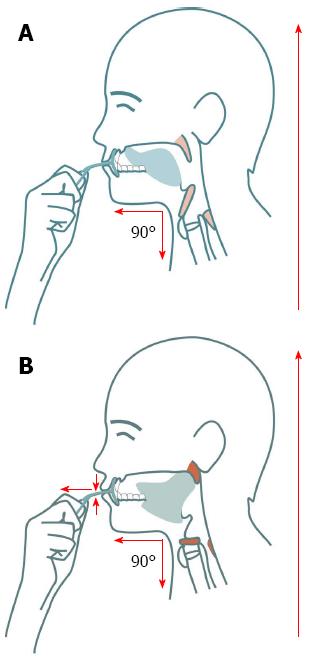
An oral IQS (Figures 1 and 2) was inserted behind closed lips, and the patient was told to draw it forward in a horizontal direction from the lips, gradually increasing the pulling pressure for 5-10 s while trying to resist the force by tightening the lips. The exercise was performed three times per session, with 3 s of rest between each repetition, three times daily before eating.
A professional statistician from Uppsala Clinical Research Centre consolidated and analyzed all collected data according to an initial protocol. The Wilcoxon signed rank test was used to compare data within groups for all symptoms and the results of visual analogue scale tests, lip force tests, and velopharyngeal closure tests before and after IQS training. The Mann-Whitney U test was used to compare dysphagia and reflux symptoms between groups A and B before and after IQS training. P < 0.05 was considered significant. All statistical analyses were performed using SAS version 9.1 software (SAS Institute, Inc., Carey, NC, United States). A statistical review of this study was performed by a biomedical statistician before submission of the manuscript.
Esophageal dysphagia was present in all 43 patients, and 98% of patients showed improvement after IQS training (P < 0.001; Table 1). The visual analogue scale scores were initially classified as pathologic in all 43 patients, and 100% of patients improved after IQS training (P < 0.001). At baseline, reflux symptoms were recorded in 86% of patients who showed significant improvement after training (P < 0.001). No significant difference in symptom frequency was found between groups A and B before or after IQS training. Lip force test and velopharyngeal closure test scores showed significant improvement after IQS training (P < 0.001). All orofacial motor tests and oral sensory test scores were initially normal.
| Parameter | Groups A and B | Group A | Group B | P value | |||
| n = 43 | P value (B vs E) | n = 21 | P value (B vs E) | n = 22 | P value (B vs E) | (group A vs group B) | |
| Esophageal dysphagia (score 0-3) | < 0.001 | < 0.001 | < 0.001 | NS | |||
| B | 2.5 (1-3) | 2.5 (1-3) | 2.5 (2-3) | NS | |||
| E | 0.9 (0-2) | 0.9 (0-2) | 0.9 (0-2) | NS | |||
| Reflux (score 0-3) | < 0.001 | < 0.001 | < 0.001 | NS | |||
| B | 1.7 (0-3) | 2.0 (1-3) | 1.4 (0-3) | NS | |||
| E | 0.5 (0-3) | 0.7 (0-2) | 0.3 (0-1) | NS | |||
| Visual analogue scale (score 0-100) | < 0.001 | < 0.001 | < 0.001 | ||||
| B | 71 (30-100) | 71 (30-100) | 70 (30-100) | ||||
| E | 22 (0-50) | 24 (0-50) | 21 (0-50) | ||||
| Lip force test (index ≥ 15 N) | < 0.001 | < 0.001 | < 0.001 | ||||
| B | 31(12-80) | 26 (12-43) | 39 (14-80) | ||||
| E | 54 (27-116) | 49 (27-84) | 64 (40-116) | ||||
| Velopharyngeal closure test (index ≥ 10 s) | < 0.001 | < 0.001 | < 0.001 | ||||
| B | 28 (5-74) | 26 (10-53) | 29 (5-50) | ||||
| E | 34 (13-80) | 32 (17-65) | 36 (13-60) | ||||
IQS traction significantly increased the pressure in the UES and diaphragmatic hiatus region (Table 2).
| Item | UES (n = 12) | Hiatus canal (n = 12) |
| Resting pressure (mmHg) | 68 (40–110) | 0 (0–0) |
| IQS traction (mmHg) | 95 (80–130) | 65 (20–100) |
This study of IQS training showed significant improvement of long-lasting esophageal dysphagia and symptomatic gastroesophageal reflux in adults. Dysphagia is often a poorly defined symptom and can lead to misinterpretation of investigative and therapeutic results[12]. Long-lasting oropharyngeal dysphagia is mostly of neurologic origin[13], whereas esophageal dysphagia presents either a stenotic character, which causes a blocking feeling with a certain ingested bolus size[14], or an intermittent nonstenotic character, which is common in patients with hiatal hernia[15]. Patients referred to a speech and swallowing center for dysphagia treatment were examined using various oropharyngeal motor tests to ensure the absence of oropharyngeal dysphagia of central nervous system origin. These tests were also found to be valuable for confirming patient compliance with IQS training.
IQS training has been shown to have a training effect on the striated muscles involved in the buccinator mechanism[3,4] and the UES. The present esophageal HRM study showed that traction with an IQS activates striated muscles in the UES and the hiatus region of the diaphragm. Therefore, it seems reasonable that IQS training over a long period of time will have a training effect on the muscles around the hiatus canal and improve hiatal competence. However, determining whether the IQS training effect can be obtained in less than six months and remain after the end of training was beyond the scope of this study. In a surgical study, tightening of the hiatus canal in association with hiatal hernia surgery relieved esophageal dysphagia[16].
The frequency of dysphagia and reflux symptoms at baseline and after IQS training did not differ between patients with and without hiatal hernia in this study. However, radiologic examination could not completely exclude hiatal hernia among patients in group B, as most radiologists do not perform esophageal examination in patients with dysphagia in recumbency[17]. Moreover, a sliding hiatal hernia will be overlooked when the X-ray examination is performed in the upright position[18]. Most patients with hiatal hernia have intermittent esophageal dysphagia, pathologic gastroesophageal reflux, or both[19,20]. In the present study, the frequency of symptoms of dysphagia and reflux and the training effect on these symptoms did not differ between the groups, which indicates that hiatal hernia was likely missed on the radiologic examination in group B. Because no patient was administered PPI medication after entry into this study, medication can be excluded as the cause for improvement.
In conclusion, oral IQS training can relieve/improve symptoms of esophageal dysphagia and gastroesophageal reflux in adults, likely due to improved hiatal competence.
Intermittent meal-related periods of food retention in the chest, termed esophageal dysphagia, and reflux symptoms are common problems in patients with hiatal hernia. Surgical repair of the hiatal hernia is the only option if antireflux medication with proton pump inhibitors is insufficient. However, surgical repair is not without undesired side effects, is expensive, and is not easily available for most patients.
Oropharyngeal dysphagia can be improved by oral and pharyngeal muscle training with an oral IQoroR screen (IQS). The present study aimed to investigate whether IQS training can improve esophageal dysphagia and reflux symptoms in a manner similar to that of hiatal hernia surgery.
Forty-three patients who had received proton pump inhibitors for more than one year, without any effect on esophageal dysphagia and symptomatic reflux, received training with an IQS for six months. Esophageal dysphagia showed significant improvement in 42 patients and reflux symptoms improved in 36 patients. Traction with IQS showed that the diaphragmatic hiatus pressure had increased, which is a prerequisite for training the muscles around the hiatus canal and for improvement of hiatal competence. These results show that IQS training can relieve/improve symptoms of esophageal dysphagia and reflux in adults, likely due to improvement of hiatal competence. IQS training therefore seems to represent a promising, inexpensive, and easily available alternative to hiatal hernia surgery.
The oral IQS screen is inserted predentally behind closed lips, and the patient then draws the screen backwards in a horizontal direction, gradually increasing the pulling pressure for five to ten seconds while trying to resist the force by tightening the lips. This exercise must be performed three times per session, with three seconds of rest between repetitions, three times daily before eating.
Proton pump inhibitors are a group of drugs whose main action is a pronounced and long-lasting reduction of gastric acid production.
The study is innovative and promotes nonsurgical treatment of reflux, which can-when widely accepted and adopted-defer unnecessary surgery. This manuscript shows very interesting and promising data that IQS training is effective at treating patients with esophageal dysphagia and reflux symptoms.
P- Reviewer: Gillessen A, Meshikhes AWN, Nagahara H S- Editor: Ma YJ L- Editor: AmEditor E- Editor: Ma S
| 1. | Hägg M, Anniko M. Lip muscle training in stroke patients with dysphagia. Acta Otolaryngol. 2008;128:1027-1033. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Hägg M, Tibbling L. Longstanding Effect and Outcome Differences of Palatal Plate and Oral Screen Training on Stroke-Related Dysphagia. Open Rehabil Jl. 2013;6:26-33. [Cited in This Article: ] |
| 3. | Perkins RE, Blanton PL, Biggs NL. Electromyographic analysis of the “baccinator mechanism” in human beings. J Dent Res. 1977;56:783-794. [PubMed] [Cited in This Article: ] |
| 4. | Logemann JA. Screening, diagnosis, and management of neurogenic dysphagia. Semin Neurol. 1996;16:319-327. [PubMed] [Cited in This Article: ] |
| 5. | Mjönes AB, Ledin T, Grahn LT, Hultcrantz E. Hoarseness and misdirected swallowing before and after antireflux surgery. Acta Otolaryngol. 2005;125:82-85. [PubMed] [Cited in This Article: ] |
| 6. | Hägg M, Larsson B. Effects of motor and sensory stimulation in stroke patients with long-lasting dysphagia. Dysphagia. 2004;19:219-230. [PubMed] [Cited in This Article: ] |
| 7. | Calhoun KH, Gibson B, Hartley L, Minton J, Hokanson JA. Age-related changes in oral sensation. Laryngoscope. 1992;102:109-116. [PubMed] [Cited in This Article: ] |
| 8. | Hägg M, Olgarsson M, Anniko M. Reliable lip force measurement in healthy controls and in patients with stroke: a methodologic study. Dysphagia. 2008;23:291-296. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Hägg M, Anniko M. Influence of lip force on swallowing capacity in stroke patients and in healthy subjects. Acta Otolaryngol. 2010;130:1204-1208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Netsell R, Hixon TJ. A noninvasive method for clinically estimating subglottal air pressure. J Speech Hear Disord. 1978;43:326-330. [PubMed] [Cited in This Article: ] |
| 11. | Tibbling L, Gezelius P, Franzén T. Factors influencing lower esophageal sphincter relaxation after deglutition. World J Gastroenterol. 2011;17:2844-2847. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 12. | Valdovinos MA, Zavala-Solares MR, Coss-Adame E. Esophageal hypomotility and spastic motor disorders: current diagnosis and treatment. Curr Gastroenterol Rep. 2014;16:421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 10] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 13. | Aydogdu I, Kiylioglu N, Tarlaci S, Tanriverdi Z, Alpaydin S, Acarer A, Baysal L, Arpaci E, Yuceyar N, Secil Y. Diagnostic value of “dysphagia limit” for neurogenic dysphagia: 17 years of experience in 1278 adults. Clin Neurophysiol. 2015;126:634-643. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Kockelkoren E, Sleeboom C, van der Voorn JP, Wilde JC, Koot BG, Kneepkens CM. [Dysphagia after introduction of solid food: typical presentation of congenital oesophageal stenosis]. Ned Tijdschr Geneeskd. 2012;156:A3794. [PubMed] [Cited in This Article: ] |
| 15. | Shin GH, Sankineni A, Parkman HP. Bolus retention in hiatal hernia identified by high-resolution esophageal manometry with impedance. Neurogastroenterol Motil. 2014;26:679-684. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Kang T, Urrego H, Gridley A, Richardson WS. Pledgeted repair of giant hiatal hernia provides excellent long-term results. J Laparoendosc Adv Surg Tech A. 2014;24:684-687. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 17. | Nin CS, Marchiori E, Irion KL, Paludo Ade O, Alves GR, Hochhegger DR, Hochhegger B. Barium swallow study in routine clinical practice: a prospective study in patients with chronic cough. J Bras Pneumol. 2013;39:686-691. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Fransson SG, Sökjer H, Johansson KE, Tibbling L. Radiologic diagnosis of gastro-oesophageal reflux by means of graded abdominal compression. Acta Radiol. 1988;29:45-48. [PubMed] [Cited in This Article: ] |
| 19. | Johansson KE, Ask P, Boeryd B, Fransson SG, Tibbling L. Oesophagitis, signs of reflux, and gastric acid secretion in patients with symptoms of gastro-oesophageal reflux disease. Scand J Gastroenterol. 1986;21:837-847. [PubMed] [Cited in This Article: ] |
| 20. | Tibbling L, Johansson M, Mjönes AB, Franzén T. Globus jugularis and dysphagia in patients with hiatus hernia. Eur Arch Otorhinolaryngol. 2010;267:251-254. [PubMed] [Cited in This Article: ] |