Published online May 28, 2015. doi: 10.3748/wjg.v21.i20.6409
Peer-review started: November 3, 2014
First decision: December 26, 2014
Revised: January 26, 2015
Accepted: February 11, 2015
Article in press: February 11, 2015
Published online: May 28, 2015
Processing time: 209 Days and 11.8 Hours
Mesenchymal hamartomas of the liver (MHLs) in adults are rare and potentially premalignant lesions, which present as solid/cystic neoplasms. We report a rare case of orthotopic liver transplantation in a patient with a giant MHL. In 2013, a 34-year-old female sought medical advice after a 2-year history of progressive abdominal distention and respiratory distress. Physical examination revealed an extensive mass in the abdomen. Computed tomography (CT) of her abdomen revealed multiple liver cysts, with the diameter of largest cyst being 16 cm × 14 cm. The liver hilar structures were not clearly displayed. The adjacent organs were compressed and displaced. Initial laboratory tests, including biochemical investigations and coagulation profile, were unremarkable. Tumor markers, including levels of AFP, CEA and CA19-9, were within the normal ranges. The patient underwent orthotopic liver transplantation in November 2013, the liver being procured from a 40-year-old man after cardiac death following traumatic brain injury. Warm ischemic time was 7.5 min and cold ischemic time was 3 h. The recipient underwent classical orthotopic liver transplantation. The recipient operative procedure took 8.5 h, the anhepatic phase lasting for 1 h without the use of venovenous bypass. The immunosuppressive regimen included intraoperative induction with basiliximab and high-dose methylprednisolone, and postoperative maintenance with tacrolimus, mycophenolate mofetil, and prednisone. The recipient’s diseased liver weighed 21 kg (dry weight) and measured 41 cm × 32 cm × 31 cm. Histopathological examination confirmed the diagnosis of an MHL. The patient did not experience any acute rejection episode or other complication. All the laboratory tests returned to normal within one month after surgery. Three months after transplantation, the immunosuppressive therapy was reduced to tacrolimus monotherapy, and the T-tube was removed after cholangiography showed no abnormalities. Twelve months after transplantation, the patient remains well and is fulfilling all normal activities. Adult giant MHL is extremely rare. Symptoms, physical signs, laboratory results, and radiographic imaging are nonspecific and inconclusive. Surgical excision of the lesion is imperative to make a definite diagnosis and as a cure. Liver transplantation should be considered as an option in the treatment of a non-resectable MHL.
Core tip: Mesenchymal hamartoma of the liver is a rare disease in adults. Only 45 patients with this condition have been reported worldwide. This report presents a rare case of adult giant mesenchymal hamartoma of the liver that could not be treated by partial hepatectomy. Orthotopic liver transplantation relieved compression of other organs and avoided the risk of malignant change. Liver transplantation should be considered as an option in the treatment of non-resectable benign hepatic tumors.
- Citation: Li J, Cai JZ, Guo QJ, Li JJ, Sun XY, Hu ZD, Cooper DK, Shen ZY. Liver transplantation for a giant mesenchymal hamartoma of the liver in an adult: Case report and review of the literature. World J Gastroenterol 2015; 21(20): 6409-6416
- URL: https://www.wjgnet.com/1007-9327/full/v21/i20/6409.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i20.6409
Mesenchymal hamartoma of the liver (MHL) was first described by Edmondson in 1956[1]. It is a rare mesenchymal tumor affecting almost exclusively infants and children in the first two years of life, with a slight male predilection. Its occurrence in children older than five years is rare (about 5% of cases) and is extremely rare in adults[2-4]. MHL is a potentially premalignant lesion that presents as a solid/cystic neoplasm. The patient’s symptoms are typically nonspecific, though abdominal pain is the most common. Laboratory results are noncontributory and radiographic imaging is variable and inconclusive. Needle biopsy is rarely diagnostic and surgical excision of symptomatic or enlarging lesions is recommended to exclude the possibility of malignancy and to establish a diagnosis[5].
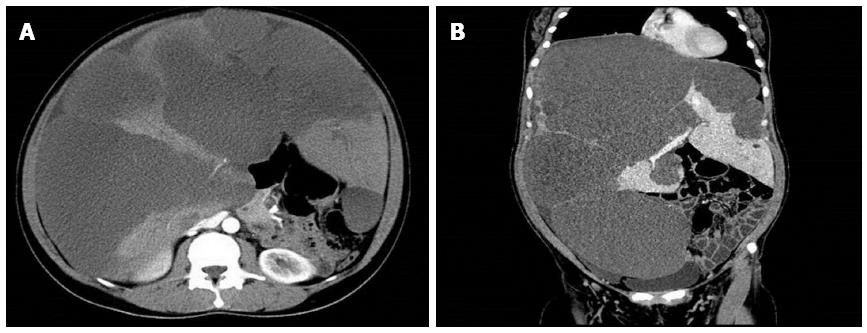
A 34-year-old, previously healthy, woman presented in 2011 with abdominal fullness and loss of appetite. She took no medications, had no history of liver disease, and denied alcohol and drug use, including the use of anabolic steroids. She presented to our hospital with increasing abdominal girth, abdominal pain, and vomiting. Physical examination revealed a grossly distended abdomen without evidence of ascites, a firm and massively enlarged liver extending below the umbilicus, and tenderness in the upper quadrant. Contrast enhanced computed tomography (CT) of the abdomen revealed near replacement of the liver with diffuse cystic masses of low density (Figure 1). Initial laboratory test results were unremarkable. Hematological, biochemical investigations and the coagulation profile were within normal limits. Tumor markers, including levels of α-fetoprotein, and carcinoembryonic antigen, carbohydrate antigen 19-9, were within the normal ranges. Serology for hepatitis B virus, hepatitis C virus and human immunodeficiency virus was negative. The extensive hepatic involvement precluded resection, and so she was evaluated and placed on the waiting list for liver transplantation.
The patient underwent orthotopic liver transplantation in November 2013. Our techniques of organ procurement and preservation have been previously described[6,7]. The liver graft was procured from a 40-year-old male donor after cardiac death. The liver graft was preserved in 4 °C UW solution. The warm ischemia time was 7.5 min and cold ischemia time was 3 h.
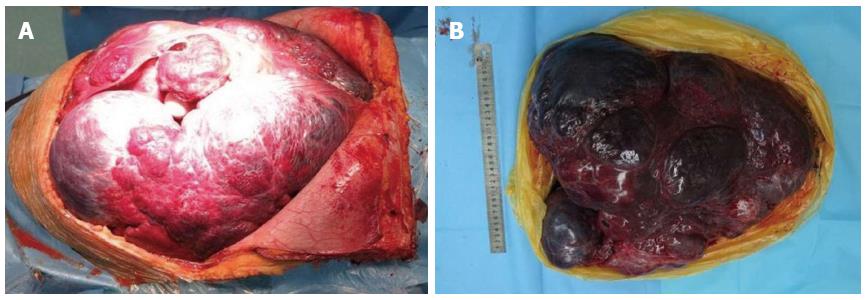
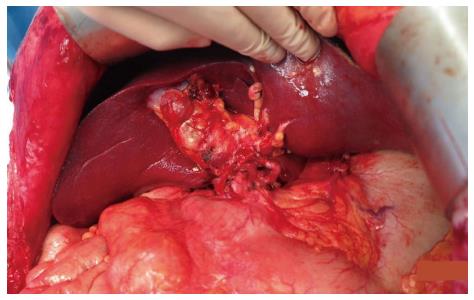
The native diseased liver filled about 80% of the abdominal cavity and displaced the normal vascular anatomy. The excised diseased native liver weighed 20 kg (dry weight) and measured 41 cm × 32 cm × 31 cm (Figure 2). The recipient operation was conducted according to the classical orthotopic liver transplantation procedure[8]. The whole transplant procedure took 8.5 h and the total blood volume loss was 5500 mL. A blood reinfusion system replaced 3000 mL, and an additional 10 units of packed RBC and 1000ml of plasma were infused. The anhepatic phase lasted for 1 h without the use of venovenous bypass. After release of the vascular clamps, Doppler ultrasound demonstrated the liver graft to be well perfused (Figure 3). The patient was extubated on the second day after surgery.
The immunosuppressive regimen included intraoperative induction with basiliximab and high-dose methylprednisolone, and postoperative maintenance with tacrolimus, mycophenolate mofetil and prednisone. No acute rejection episode was documented. The patient was discharged home on postoperative day 20, at which time all laboratory tests were within normal limits. Three months after the operation, the immunosuppressive regimen was reduced to tacrolimus monotherapy, and the T-tube was removed after cholangiography showed no abnormalities. After 12 mo, the patient remains well and is carrying out all normal activities.
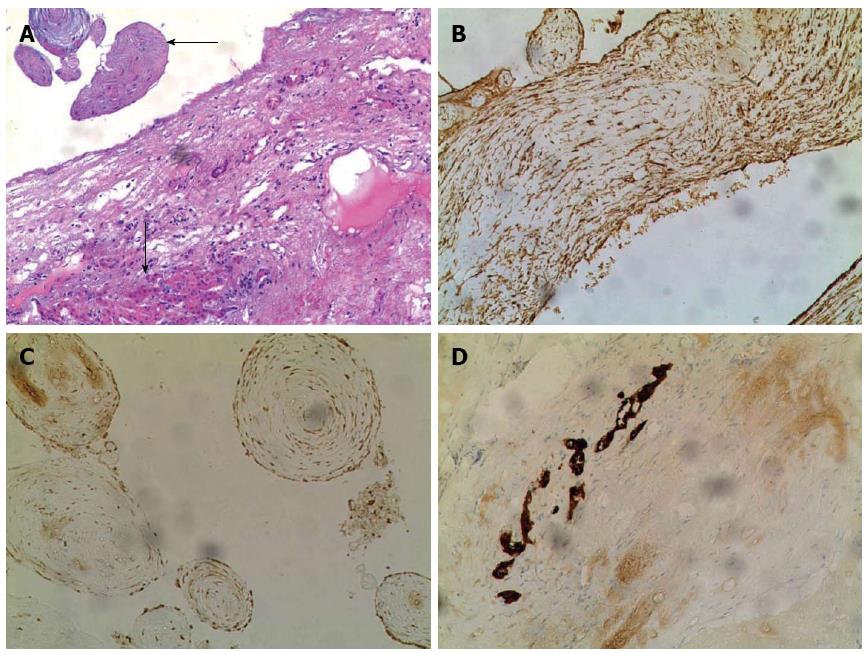
Pathologic examination of the excised diseased native liver was carried out. It contained multiple well-circumscribed masses, ranging in diameter from 2-16 cm. All masses were cystic in the central portion and contained 20-50 mL of muddy yellowish or bloody fluid. The liver mass contained dilated bile ducts with connective tissue forming multiple cysts. Histologically, corresponding to the cystic areas noted grossly, myxoid stroma and spindle cells showed smooth muscle differentiation, confirmed by positive staining for vimentin and smooth muscle actin. Benign dilated bile ducts were confirmed by positive staining for cytokeratin 7. In peripheral areas, only small amounts of liver tissue remained, with a lack of lobular architecture. There was a clear boundary between the liver parenchyma and proliferating connective tissue (Figure 4). The diagnosis of MHL was based on the typical morphological appearance, as described above.
MHL was first reported by Maresch in 1903[9]. Until relatively recently, this disease was known by different names, such as cavernous lymph adenomatoid tumor, bile cell fibroadenoma and benign mesenchymoma. The first definitive description of MHL was provided by Edmondson[1]. While the precise pathogenesis of MHL is uncertain, the most common theory relates to aberrant mesenchymal development in the portal tract, likely related to the bile ducts[10,11].
The clinical presentation of MHL appears to depend on the age of the patient. Most pediatric patients present with painless abdominal enlargement, normally appreciated by their parents[5]. However, in adult patients (age range: 19-87 years; females 62%, mean age 39 years; males 40%, mean age 60 years (Table 1), clinical features included hepatomegaly, and diffuse abdominal pain or pain in the right hypochondrium or left upper quadrant[12-14]. In severe cases, there may be compression of the diaphragm and lungs causing respiratory difficulties[4]. In the present case, the patient suffered from progressive abdominal distention and respiratory distress caused by the expanding multiple cystic masses distributed throughout the liver.
| No. | Ref. | Year | Sex | Age (yr) | Clinical manifestation | Size (cm) | Gross appearance(cystic or solid) | Liver lobe(s)affected | Surgical treatment |
| 1 | Yamamura et al[26] | 1976 | F | 22 | NA | NA | Cystic | Both | NA |
| 2 | Grases et al[27] | 1979 | F | 19 | Abdominal pain, jaundice, hepatomegaly | 24 × 19 × 8 | Cystic | Left | Left hepatic lobectomy |
| 3 | Li et al[28] | 1983 | F | 21 | Asymptomatic | 17 × 10 | Cystic | Right | Hemihepatectomy |
| 4 | Kawata et al[29] | 1984 | F | 43 | NA | 22 × 15 × 10 | Solid | Left | NA |
| 5 | Ishizuka et al[30] | 1985 | M | 59 | NA | 30 × 28 × 12 | Cystic | Right | NA |
| 6 | Kawakami et al[31] | 1986 | M | 67 | NA | NA | Cystic | Right | NA |
| 7 | Jennings et al[32] | 1987 | F | 32 | Asymptomatic | 14 × 11 | Cystic | Left | Left hepatic lobectomy |
| 8 | Kato et al[33] | 1988 | M | 66 | Asymptomatic | NA | Solid | Left | Left hepatic lobectomy |
| 9 | Gutierrez et al[34] | 1988 | F | 30 | NA | 18 | Both | Both | Non-resectable |
| 10 | Gramlich et al[35] | 1988 | F | 28 | Abdominal distention, hepatomegaly | 30 × 20 × 14 | Solid | Right | Right hepatic trisegmentectomy |
| 11 | Alanen et al[36] | 1989 | F | 20 | Asymptomatic | 6 × 8 | Cystic | Left | Left hepatic lobectomy |
| 12 | Ito et al[37] | 1989 | F | 43 | NA | 16 × 16 × 7.7 | Cystic | Both | NA |
| 13 | Urabe et al[38] | 1990 | F | 39 | Asymptomatic | 1.2 | Solid | Left | Left hepatic lobectomy |
| 14 | Drachenb et al[39] | 1991 | F | 69 | Asymptomatic | 26 × 20 × 11.5 | Cystic | Left | NA |
| 15 | Wada et al[40] | 1992 | M | 62 | Asymptomatic | 6 × 6 × 4.5 | Solid | Left | Hepatectomy |
| 16 | Chau et al[41] | 1994 | M | 53 | Abdominal pain | 20 × 14 × 10 | Cystic | Right | NA |
| 17 | Megremis et al[42] | 1994 | F | 56 | Abdominal pain | 7.5 | Cystic | Both | NA |
| 18 | Yamamoto et al[43] | 1994 | M | 52 | Abdominal discomfort, weight loss | 6 × 4 × 3.5 | Cystic | Left | Lateral segmentectomy |
| 19 | Chung et al[44] | 1999 | F | 57 | Abdominal discomfort, weight loss | 6 × 4 × 3.5 | Solid | Right | Right hepatectomy |
| 20 | Papastratis et al[45] | 2000 | F | 21 | Abdominal pain, abdominal mass | 17 × 10 | Cystic | Right | Right hepatectomy |
| 21 | Cook et al[13] | 2002 | F | 46 | Abdominal pain | 6 × 4 × 5 | Cystic | Right | Right hepatectomy |
| 22 | Cook et al[13] | 2002 | F | 66 | Cough and shortness of breath | 5 × 4 × 2 | Cystic | Right | Right hepatectomy |
| 23 | Cook et al[13] | 2002 | F | 63 | Abdominal pain | 11 × 16 × 24 | Solid | Left | Left hepatic lobectomy |
| 24 | Mao et al[46] | 2002 | M | 44 | Abdominal discomfort | 2 × 2 | Solid | Left | Hepatectomy |
| 25 | Mao et al[46] | 2002 | F | 43 | Asymptomatic | 3 × 4 × 4 | Cystic | Right | Right hepatectomy |
| 26 | Mao et al[46] | 2002 | M | 76 | Abdominal pain | 4 × 5 × 4 | Cystic | Right | Right hepatectomy |
| 27 | Brkic et al[47] | 2003 | M | 38 | Abdominal pain | 8 × 5 | Solid | Right | Right hepatectomy |
| 28 | Kim et al[48] | 2003 | M | NA | Asymptomatic | 5 | Both | Right | NA |
| 29 | Yesim et al[12] | 2005 | F | 54 | NA | 2.5 × 2.5 × 1.5 | Cystic | Left | Total cystectomy |
| 30 | Yesim et al[12] | 2005 | F | 51 | NA | 6 × 7 × 8 | Cystic | Right | Unroofing procedure |
| 31 | Kim et al[49] | 2006 | F | 40 | Asymptomatic | 5 × 5 | Cystic | Right | Right hepatectomy |
| 32 | Ayadi-Kaddour et al[50] | 2006 | F | 21 | NA | 11 × 5 | Cystic | Left | NA |
| 33 | Hernández et al[25] | 2006 | M | 51 | NA | 19 × 13 | Solid | Right | Liver transplantation (4th reported1) |
| 34 | Chang et al[51] | 2006 | M | 79 | Asymptomatic | 2 × 2 | NA | Right | NA |
| 35 | Chang et al[51] | 2006 | F | 39 | Asymptomatic | 5 × 5 | Cystic | NA | NA |
| 36 | Li et al[17] | 2007 | F | 33 | Abdominal distention | 16 | Both | Both | NA |
| 37 | Mori et al[52] | 2008 | F | 36 | Abdominal distention | 20 × 15 × 10 | Cystic | Right | Right hemihepatectomy |
| 38 | Giunippero et al[53] | 2009 | M | 87 | Abdominal distention | 20 × 20 | Cystic | Right | Hemihepatectomy |
| 39 | Nakajo et al[54] | 2009 | M | 38 | Asymptomatic | 5 × 5 | Solid | Right | Right hepatectomy |
| 40 | Klaassen et al[5] | 2010 | F | 53 | NA | 9 × 9 × 7.5 | Cystic | Right | Hepatectomy |
| 41 | Kulkarni et al[55] | 2010 | F | 20 | Abdominal mass, abdominal pain | 14 × 11 | cystic | Right | Mass resection |
| 42 | Tucker et al[56] | 2012 | W | 74 | Abdominal distention, abdominal pain | 18 × 15 × 13 | cystic | Left | Left hepatectomy |
| 43 | Liu et al[57] | 2013 | M | 42 | Asymptomatic | 1.5 × 1.0 × 1.0 | solid | Left | Hepatectomy |
| 44 | Lakić et al[58] | 2014 | M | 44 | Asymptomatic | 2.9 × 3.1 × 3.5 | NA | Left | Hepatectomy |
| 45 | Sharma et al[59] | 2014 | M | 81 | Abdominal distention | 21.8 × 12.3 × 18.6 | cystic | Left | Hepatectomy |
| 46 | Current case | 2014 | F | 34 | abdominal discomfort, dyspnea | 41 × 32 × 31 | cystic | Both | Liver transplantation (5th reported1) |
Concerning the localization and structure of the tumor, pediatric and adult populations have different characteristics. MHLs are more common in the left liver lobe in children. In adults, 17 cases (38%) were localized to the left lobe, 22 (49%) to the right lobe, and in six (13%) extended into both lobes (Table 1). All six cases of MHLs involving both lobes occurred in females. Among 45 cases of MHLs, 30 (67%) presented with cystic lesion, 12 (26%) with solid lesions, and three (7%) with both types. Of 30 cases of cystic MHLs, 21 (70%) were reported in females and only nine (30%) in males (Table 1).
MHLs are difficult to diagnose by laboratory tests or other investigations because of its non-specificity. Liver function tests and AFP values for MHLs are usually within normal limits[15]. Additionally, all imaging methods, including ultrasonography, CT and magnetic resonance imaging (MRI), provide nonspecific findings. The differential diagnosis of a cystic MHL includes simple liver cysts, hydatid cysts, biliary cystadenocarcinoma, and cystic metastases. If a lesion consists of a solid mass, the differential diagnosis includes focal nodular hyperplasia, hepatic adenoma, cavernous hemangioma, angiomyolipoma and hepatocellular carcinoma. In the present case, the initial abdominal enhanced CT scan revealed multiple liver cysts, which could easily have been misdiagnosed as a polycystic liver.
The diagnosis of MHL often relies on histological examination of tissue obtained by biopsy or by tumor resection; however, the histological appearance of the stromal component of an MHL can be variable. Hematoxylin and eosin (HE) staining, as well as immunohistochemical studies, have indicated MHLs as having spindle cells positive for vimentin and smooth muscle actin and negative for CD31, CD34 and S100 proteins, while the ducts stain positive for cytokeratin 7 and negative for cytokeratin 20[13,16].
MHLs have premalignant potential, particularly in adult patients[17]. The potential malignant evolution of a subset of MHLs into embryonal sarcoma or angiosarcoma supports the necessity for complete surgical excision both in children and adults[4,18]. Incomplete resection or marsupialization must be avoided because of the possibility of recurrence[19-21]. Laparoscopic liver resection for MHLs has been reported with successful outcomes[22].
Very rarely an MHL is non-resectable, even in an experienced center, and liver transplantation may have to be considered. Tepetes et al[23] reported two children who underwent liver transplantation following partial resections for MHLs. One died from intraoperative bleeding and the other survived. Bejarano et al[24] described a neonate with a recurrent MHL (after resection) who underwent successful liver transplantation. Hernández et al[25] reported the first case of an MHL in an adult that was treated by liver transplantation.
In conclusion, giant MHLs in adults are extremely rare. Clinical features, laboratory results and radiographic imaging are often nonspecific and inconclusive. Surgical excision of the whole lesion is imperative for both definitive diagnosis and cure. Liver transplantation should be considered as an option in the treatment of non-resectable MHLs.
A 34-year-old female with a history of progressive abdominal distention and respiratory distress.
Physical examination revealed a grossly distended abdomen without evidence of ascites, a firm and massively enlarged liver extending below the umbilicus, and tenderness in the upper quadrant.
Polycystic liver, hydatid cyst, biliary cystadenocarcinoma and cystic metastases.
Laboratory test results were unremarkable and non-diagnostic.
Abdominal computed tomography scan showed multiple liver cysts, with the diameter of the largest cyst being 16 cm × 14 cm. The liver hilar structures were not clearly displayed. The adjacent organs were compressed and displaced.
Histological examination showed dilated bile ducts and extensive connective tissue in the liver mass, while immunohistochemical staining showed positivity for vimentin, smooth muscle actin and cytokeratin 7.
The patient underwent orthotopic liver transplantation.
Mesenchymal hamartoma of the liver is a rare disease in adults and only 45 patients with this condition have been reported; the references are cited.
Mesenchymal hamartoma of the liver is a rare and potentially premalignant lesion that presents as a solid/cystic neoplasm. The pathogenesis remains incompletely understood; however, these lesions have generally been considered to represent a developmental abnormality in bile duct plate formation.
This case report represents a successful application of liver transplantation for adult giant mesenchymal hamartomas of the liver, which could not be treated by conventional partial hepatectomy. We recommend that liver transplantation should be considered as an option in the treatment of non-resectable benign hepatic tumors.
This paper is a case report of a 34-year-old woman with liver transplantation for a giant mesenchymal hamartoma of the liver. Mesenchymal hamartoma of liver is a rare disease in adults and only 31 patients have been reported to date worldwide.
P- Reviewer: Nakayama Y, Ohkohchi N S- Editor: Ma YJ L- Editor: Stewart G E- Editor: Wang CH
| 1. | Edmondson HA. Differential diagnosis of tumors and tumor-like lesions of liver in infancy and childhood. AMA J Dis Child. 1956;91:168-186. [PubMed] [Cited in This Article: ] |
| 2. | Stringer MD, Alizai NK. Mesenchymal hamartoma of the liver: a systematic review. J Pediatr Surg. 2005;40:1681-1690. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 142] [Cited by in F6Publishing: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 3. | Isaacs H. Fetal and neonatal hepatic tumors. J Pediatr Surg. 2007;42:1797-1803. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 168] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 4. | Meyers RL. Tumors of the liver in children. Surg Oncol. 2007;16:195-203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 152] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 5. | Klaassen Z, Paragi PR, Chamberlain RS. Adult Mesenchymal Hamartoma of the Liver: Case Report and Literature Review. Case Rep Gastroenterol. 2010;4:84-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | D’Alessandro AM, Hoffmann RM, Knechtle SJ, Eckhoff DE, Love RB, Kalayoglu M, Sollinger HW, Belzer FO. Successful extrarenal transplantation from non-heart-beating donors. Transplantation. 1995;59:977-982. [PubMed] [Cited in This Article: ] |
| 7. | D’alessandro AM, Hoffmann RM, Knechtle SJ, Odorico JS, Becker YT, Musat A, Pirsch JD, Sollinger HW, Kalayoglu M. Liver transplantation from controlled non-heart-beating donors. Surgery. 2000;128:579-588. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 154] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Starzl TE, Groth CG, Brettschneider L, Penn I, Fulginiti VA, Moon JB, Blanchard H, Martin AJ, Porter KA. Orthotopic homotransplantation of the human liver. Ann Surg. 1968;168:392-415. [PubMed] [Cited in This Article: ] |
| 9. | Motiwale SS, Karmarkar SJ, Oak SN, Kalgutkar AD, Deshmukh SS. Cystic mesenchymal hamartoma of the liver--a rare condition. Indian J Cancer. 1996;33:157-160. [PubMed] [Cited in This Article: ] |
| 10. | Dehner LP, Ewing SL, Sumner HW. Infantile mesenchymal hamartoma of the liver. Histologic and ultrastructural observations. Arch Pathol. 1975;99:379-382. [PubMed] [Cited in This Article: ] |
| 11. | von Schweinitz D, Dammeier BG, Glüer S. Mesenchymal hamartoma of the liver--new insight into histogenesis. J Pediatr Surg. 1999;34:1269-1271. [PubMed] [Cited in This Article: ] |
| 12. | Yesim G, Gupse T, Zafer U, Ahmet A. Mesenchymal hamartoma of the liver in adulthood: immunohistochemical profiles, clinical and histopathological features in two patients. J Hepatobiliary Pancreat Surg. 2005;12:502-507. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Cook JR, Pfeifer JD, Dehner LP. Mesenchymal hamartoma of the liver in the adult: association with distinct clinical features and histological changes. Hum Pathol. 2002;33:893-898. [PubMed] [Cited in This Article: ] |
| 14. | Karpelowsky JS, Pansini A, Lazarus C, Rode H, Millar AJ. Difficulties in the management of mesenchymal hamartomas. Pediatr Surg Int. 2008;24:1171-1175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Ito H, Kishikawa T, Toda T, Arai M, Muro H. Hepatic mensenchymal hamartoma of an infant. J Pediatr Surg. 1984;19:315-317. [PubMed] [Cited in This Article: ] |
| 16. | Lauwers GY, Grant LD, Donnelly WH, Meloni AM, Foss RM, Sanberg AA, Langham MR. Hepatic undifferentiated (embryonal) sarcoma arising in a mesenchymal hamartoma. Am J Surg Pathol. 1997;21:1248-1254. [PubMed] [Cited in This Article: ] |
| 17. | Li Q, Wang J, Sun Y, Cui Y, Hao X. Hepatic angiosarcoma arising in an adult mesenchymal hamartoma. Int Semin Surg Oncol. 2007;4:3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | von Schweinitz D. Neonatal liver tumours. Semin Neonatol. 2003;8:403-410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Shuto T, Kinoshita H, Yamada C, Hirohashi K, Shiokawa C, Kubo S, Fujio N, Kobayashi Y. Bilateral lobectomy excluding the caudate lobe for giant mesenchymal hamartoma of the liver. Surgery. 1993;113:215-222. [PubMed] [Cited in This Article: ] |
| 20. | Murray JD, Ricketts RR. Mesenchymal hamartoma of the liver. Am Surg. 1998;64:1097-1103. [PubMed] [Cited in This Article: ] |
| 21. | Sharif K, Ramani P, Lochbühler H, Grundy R, de Ville de Goyet J. Recurrent mesenchymal hamartoma associated with 19q translocation. A call for more radical surgical resection. Eur J Pediatr Surg. 2006;16:64-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Yoon YS, Han HS, Choi YS, Lee SI, Jang JY, Suh KS, Kim SW, Lee KU, Park YH. Total laparoscopic left lateral sectionectomy performed in a child with benign liver mass. J Pediatr Surg. 2006;41:e25-e28. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Tepetes K, Selby R, Webb M, Madariaga JR, Iwatsuki S, Starzl TE. Orthotopic liver transplantation for benign hepatic neoplasms. Arch Surg. 1995;130:153-156. [PubMed] [Cited in This Article: ] |
| 24. | Bejarano PA, Serrano MF, Casillas J, Dehner LP, Kato T, Mitral N, Rodriguez MM, Tzakis A. Concurrent infantile hemangioendothelioma and mesenchymal hamartoma in a developmentally arrested liver of an infant requiring hepatic transplantation. Pediatr Dev Pathol. 2003;6:552-557. [PubMed] [Cited in This Article: ] |
| 25. | Hernández JC, Alfonso C, González L, Samada M, Ramos L, Cepero-Valdez M, Antonio Abdo A, Gómez F, Castellanos R, López O. Solid mesenchymal hamartoma in an adult: a case report. J Clin Pathol. 2006;59:542-545. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Yamamura T, Kameyama Y, Hoshino T, Hayakawa K. A case of mesenchymal hamartoma of the liver coexisting with congenital dilatation of the bile duct (translation of japanese title). J Jpn Soc Clin Surg. 1976;37:862. [Cited in This Article: ] |
| 27. | Grases PJ, Matos-Villalobos M, Arcia-Romero F, Lecuna-Torres V. Mesenchymal hamartoma of the liver. Gastroenterology. 1979;76:1466-1469. [PubMed] [Cited in This Article: ] |
| 28. | Li A, Sherlock S. A giant cystic mesenchymal hamartoma of the liver: Diagnosis, management, and study of cyst fluid. Gastroenterology. 1983;85:958-961. [Cited in This Article: ] |
| 29. | Kawata T, Nakamura S, Nakayama A, Fukuda H, Ebara M, Nagamine T, Minami T, Sakurai H. An improved diagnostic method for chronic hepatic disorder: analyses of metallothionein isoforms and trace metals in the liver of patients with hepatocellular carcinoma as determined by capillary zone electrophoresis and inductively coupled plasma-mass spectrometry. Biol Pharm Bull. 2006;29:403-409. [PubMed] [Cited in This Article: ] |
| 30. | Ishizuka M, Miyashita M, Takahama M. A case of giant mesenchymal hamartoma of the liver found in an adult. Proceedings of the Proc Jpn Cancer Assoc. 1985;490. [Cited in This Article: ] |
| 31. | Kawakami A, Fujii H, Ono Y. A case of hepatic mesenchymal hamartoma in an adult. Nippon Act Radiol. 1986;46:1073. [Cited in This Article: ] |
| 32. | Jennings CM, Merrill CR, Slater DN. The computed tomographic appearances of benign hepatic hamartoma. Clin Radiol. 1987;38:103-104. [PubMed] [Cited in This Article: ] |
| 33. | Kato Y, Yokozaki H. Hepatic mass (mesenchymal hamartoma). J Hiroshima Med Assoc. 1988;41:143. [Cited in This Article: ] |
| 34. | Gutierrez OH, Burgener FA. Mesenchymal hamartoma of the liver in an adult: radiologic diagnosis. Gastrointest Radiol. 1988;13:341-344. [PubMed] [Cited in This Article: ] |
| 35. | Gramlich TL, Killough BW, Garvin AJ. Mesenchymal hamartoma of the liver: report of a case in a 28-year-old. Hum Pathol. 1988;19:991-992. [PubMed] [Cited in This Article: ] |
| 36. | Alanen A, Katevuo K, Toikkanen S. A non-cystic mesenchymal hamartoma of the liver--an unusual case of an unusual entity. Case report and review of the literature. Bildgebung. 1987;56:181-184. [PubMed] [Cited in This Article: ] |
| 37. | Ito Y, Seto Y, Okano H, Ueda T, Imanishi H, Nakamura K, Nakajima T, Okanoue T. [A case of mesenchymal hamartoma of the liver in adult woman with pancreas divisum and marked delay in ICG plasma clearance]. Nihon Shokakibyo Gakkai Zasshi. 1989;86:1534-1539. [PubMed] [Cited in This Article: ] |
| 38. | Urabe S, Furukawa M, Nakata T. A case of mesenchymal hamartoma of the liver in an adult. Jpn J Gastroenterol Surg. 1990;23:664. [Cited in This Article: ] |
| 39. | Drachenberg CB, Papadimitriou JC, Rivero MA, Wood C. Distinctive case. Adult mesenchymal hamartoma of the liver: report of a case with light microscopic, FNA cytology, immunohistochemistry, and ultrastructural studies and review of the literature. Mod Pathol. 1991;4:392-395. [PubMed] [Cited in This Article: ] |
| 40. | Wada M, Ohashi E, Jin H, Nishikawa M, Shintani S, Yamashita M, Kano M, Yamanaka N, Nishigami T, Shimoyama T. Mesenchymal hamartoma of the liver: report of an adult case and review of the literature. Intern Med. 1992;31:1370-1375. [PubMed] [Cited in This Article: ] |
| 41. | Chau K, Ho J, Wu P, Yuen W. Mesenchymal hamartoma of liver in a man: comparison with cases in infants. J Clin Pathol. 1994;47:864-866. [Cited in This Article: ] |
| 42. | Megremis S, Sfakianaki E, Voludaki A, Chroniaris N. The ultrasonographic appearance of a cystic mesenchymal hamartoma of the liver observed in a middle-aged woman. J Clin Ultrasound. 1994;22:338-341. [PubMed] [Cited in This Article: ] |
| 43. | Yamamoto M, Hagihara H, Mogaki M, Iimuro Y, Fujii H, Ainota T, Akahane Y, Matsumoto Y. Adult mesenchymal hamartoma of the liver mimicking bile duct cystadenoma. J Gastroenterol. 1994;29:518-524. [PubMed] [Cited in This Article: ] |
| 44. | Chung JH, Cho KJ, Choi DW, Lee BH, Chi JG. Solid mesenchymal hamartoma of the liver in adult. J Korean Med Sci. 1999;14:335-337. [PubMed] [Cited in This Article: ] |
| 45. | Papastratis G, Margaris H, Zografos GN, Korkolis D, Mannika Z. Mesenchymal hamartoma of the liver in an adult: a review of the literature. Int J Clin Pract. 2000;54:552-554. [PubMed] [Cited in This Article: ] |
| 46. | Mao J, Chen Y, Zhang X. [Misdiagnosis of 3 adult liver hamartomas]. Zhonghua Gan Zang Bing Zazhi. 2002;10:478. [PubMed] [Cited in This Article: ] |
| 47. | Brkic T, Hrstic I, Vucelic B, Jakic-Razumovic J, Skegro M, Romic B, Cukovic-Cavka S, Pulanic R, Ostojic R. Benign mesenchymal liver hamartoma in an adult male: a case report and review of the literature. Acta Med Austriaca. 2003;30:134-137. [PubMed] [Cited in This Article: ] |
| 48. | Kim KA, Park CM, Kim CH, Choi SY, Park SW, Kang EY, Seol HY, Cha IH. An interesting hepatic mass: splenosis mimicking a hepatocellular carcinoma (2003: 9b). Eur Radiol. 2003;13:2713-2715. [PubMed] [Cited in This Article: ] |
| 49. | Kim KA, Kim KW, Park SH, Jang SJ, Park MS, Kim PN, Lee MG, Ha HK. Unusual mesenchymal liver tumors in adults: radiologic-pathologic correlation. AJR Am J Roentgenol. 2006;187:W481-W489. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 50. | Ayadi-Kaddour A, Saïji E, Ben Slama S, Chelly-Ennaiffer I, Lahmar-Boufaroua A, Goutallier-Ben Fadhel C, Ben Sassi L, Khalfallah MT, Mzabi-Regaya S. [Hepatic mesenchymal hamartoma in adulthood: a case report with literature review]. Tunis Med. 2006;84:263-265. [PubMed] [Cited in This Article: ] |
| 51. | Chang HJ, Jin SY, Park C, Park YN, Jang JJ, Park CK, Suh YL, Yu E, Kang DY, Bae HI. Mesenchymal hamartomas of the liver: comparison of clinicopathologic features between cystic and solid forms. J Korean Med Sci. 2006;21:63-68. [PubMed] [Cited in This Article: ] |
| 52. | Mori R, Morioka D, Morioka K, Ueda M, Sugita M, Takeda K, Matsuo K, Tanaka K, Endo I, Sekido H. Giant mesenchymal hamartoma of the liver in an adult. J Hepatobiliary Pancreat Surg. 2008;15:667-669. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 53. | Giunippero A, Maya AM, Gallo A, Bazzana MS, Cosentino V, Aulet FJ. [Mesenchymal hamartoma of the liver in an elderly man]. Medicina (B Aires). 2009;69:554-556. [PubMed] [Cited in This Article: ] |
| 54. | Nakajo M, Jinnouchi S, Hamada N, Sueyoshi K, Matukita S, Tanabe H, Tateno R, Nakajo M. FDG PET/CT findings of mesenchymal hamartoma of the liver in an adult. Clin Nucl Med. 2009;34:327-329. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 55. | Kulkarni MP, Agashe SR, Singh RV, Sulhyan KR. Hepatic angiosarcoma arising in an adult mesenchymal hamartoma. Indian J Pathol Microbiol. 2010;53:322-324. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 56. | Tucker SM, Cooper K, Brownschidle S, Wilcox R. Embryonal (undifferentiated) sarcoma of the liver with peripheral angiosarcoma differentiation arising in a mesenchymal hamartoma in an adult patient. Int J Surg Pathol. 2012;20:297-300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 57. | Liu Q, Liu J, Chen W, Mao S, Guo Y. Primary solitary fibrous tumors of liver: a case report and literature review. Diagn Pathol. 2013;8:195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 58. | Lakić TZ, Živojinov MM, Vuković M, Ilić-Sabo JR, Bošković T. Mesenchymal hamartoma of the liver in adults: Case report. Med Pregl. 2014;67:399-403. [Cited in This Article: ] |
| 59. | Sharma M, Bansal P, Goyal NK. Adult hepatic mesenchymal hamartoma: an unusual case. J Lab Physicians. 2014;6:124-126. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |