Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Dec 28, 2014; 20(48): 18375-18383
Published online Dec 28, 2014. doi: 10.3748/wjg.v20.i48.18375
Published online Dec 28, 2014. doi: 10.3748/wjg.v20.i48.18375
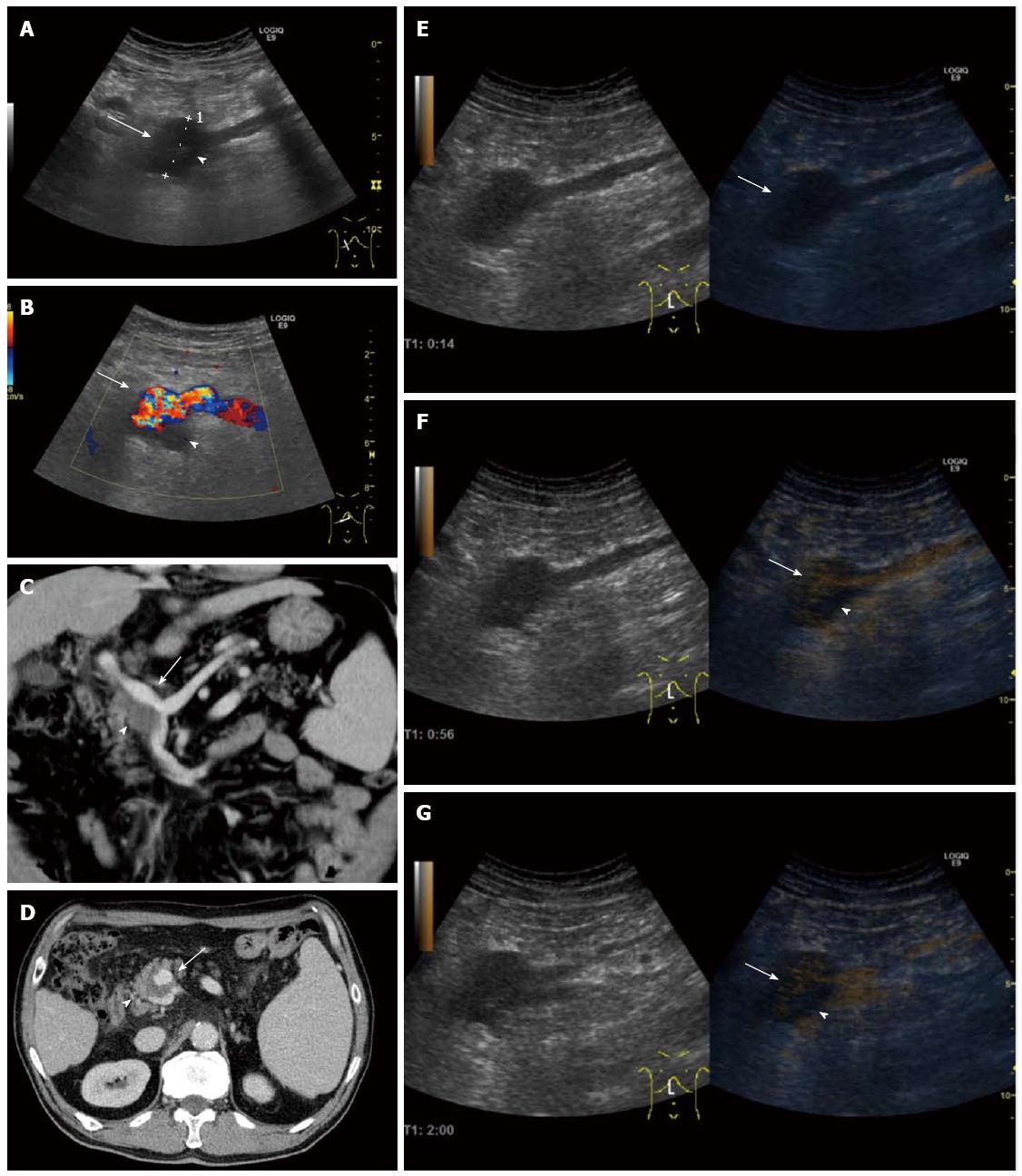
Figure 2 Patient 2: Portal venous system aneurysm in a 65-year-old man with a history of alcoholic liver cirrhosis, who presented with hematemesis secondary to rupture of esophageal varices (grade III), which were successfully treated with endoscopic ligation.
A: Right oblique sagittal view shows a focal fusiform dilatation of the portal venous system at the splenomesenteric confluence (arrow), with a maximum diameter of 37 mm (caliper 1) and lumen partially filled with a slightly echogenic area (arrowhead); B: Right oblique transverse view with color Doppler shows turbulent flow with mosaic color within patent lumen (arrow) and absence of flow within echogenic area (arrowhead); C-G: Contrast-enhanced ultrasound (CEUS) and computed tomography (CT) findings: Right oblique sagittal view shows the CEUS characteristics of the portal venous system aneurysm (PVSA), which is not enhanced in the arterial phase (14 s, arrow, E) and partially hyperenhancing through the portal venous (56 s, arrow, F) and late phase (2 min, arrow, G), with a persistent non-enhancing area in both phases (arrowheads), suggestive of incomplete appositional thrombosis of the PVSA. Axial (D) and coronal maximum intensity projection CT (C) images show the fusiform aneurysm during the portal venous phase, without enhancement in its dependent portion, confirming the diagnosis of partially thrombosed PVSA.
- Citation: Tana C, Dietrich CF, Badea R, Chiorean L, Carrieri V, Schiavone C. Contrast-enhanced ultrasound in portal venous system aneurysms: A multi-center study. World J Gastroenterol 2014; 20(48): 18375-18383
- URL: https://www.wjgnet.com/1007-9327/full/v20/i48/18375.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i48.18375