Published online Dec 28, 2014. doi: 10.3748/wjg.v20.i48.18384
Revised: July 23, 2014
Accepted: August 13, 2014
Published online: December 28, 2014
Processing time: 215 Days and 9.2 Hours
AIM: To assess the outcome of patients treated conservatively vs surgically during their first admission for sigmoid volvulus.
METHODS: We conducted a retrospective study of 61 patients admitted to Aarhus University Hospital in Denmark between 1996 and 2011 for their first incidence of sigmoid volvulus. The condition was diagnosed by radiography, sigmoidoscopy or surgery. Patients treated with surgery underwent either a sigmoid resection or a percutaneous endoscopic colostomy (PEC). Conservatively treated patients were managed without surgery. Data was recorded into a Microsoft Access database and calculations were performed with Microsoft Excel. Kaplan-Meier plotting and Mantel-Cox (log-rank) testing were performed using GraphPad Prism software. Mortality was defined as death within 30 d after intervention or surgery.
RESULTS: Among the total 61 patients, 4 underwent emergency surgery, 55 underwent endoscopy, 1 experienced resolution of the volvulus after contrast enema, and 1 died without treatment because of large bowel perforation. Following emergency treatment, 28 patients underwent sigmoid resection (semi-elective n = 18; elective n = 10). Two patients who were unfit for surgery underwent PEC and both died, 1 after 36 d and the other after 9 mo, respectively. The remaining 26 patients were managed conservatively without sigmoid resection. Patients treated conservatively on their first admission had a poorer survival rate than patients treated surgically on their first admission (95%CI: 3.67-14.37, P = 0.036). Sixty-three percent of the 26 conservatively treated patients had not experienced a recurrence 3 mo after treatment, but that number dropped to 24% 2 years after treatment. Eight of the 14 patients with recurrence after conservative treatment had surgery with no 30-d mortality.
CONCLUSION: Surgically-treated sigmoid volvulus patients had a higher long-term survival rate than conservatively managed patients, indicating a benefit of surgical resection or PEC insertion if feasible.
Core tip: The present study is the first international publication on sigmoid volvulus using a Kaplan-Meier analysis to illustrate the differences in mortality and recurrence after surgical vs conservative treatment. The long-term survival rate was higher for patients who underwent sigmoid resection as treatment than it was for patients who were managed conservatively. The results indicate that more patients should undergo sigmoid resection after emergency sigmoidoscopic decompression.
- Citation: Ifversen AKW, Kjaer DW. More patients should undergo surgery after sigmoid volvulus. World J Gastroenterol 2014; 20(48): 18384-18389
- URL: https://www.wjgnet.com/1007-9327/full/v20/i48/18384.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i48.18384
Sigmoid volvulus is the most common type of volvulus[1]. In the Western world it represents 3% to 5% of all acute intestinal obstructions. The male:female ratio of this condition is 1.4:1, and the average age of development is 68 years[2]. From an anatomical perspective, sigmoid volvulus is characterized by an axial twisting of the sigmoid colon to a minimum of 180 degrees[3]. The predisposing factors are assumed to be a long mesocolon and a sigmoid colon with a narrow mesentery[4,5]. Whether this condition is congenital, acquired, or a combination of the two, has not yet been determined[2]. Presenting populations vary widely throughout the world; for example, most Western patients are institutionalized and elderly with many comorbidities[6-8] but in the rest of the world, where the condition is endemic and not sporadic, sigmoid volvulus patients are younger with no comorbidities[2]. Studies have shown that the condition is associated with a high fiber diet, megacolon, former abdominal surgery, high altitude, chronic constipation and neurological diseases. Chronic constipation and neurological diseases are the most common causes in the Western world[6-8].
Sigmoid volvulus is diagnosed by radiography, sigmoidoscopy, or laparotomy[9-11]. Initial treatment involves sigmoidoscopy with decompression and detorsion, with or without placement of a rectal tube[2]. The success rate for sigmoidoscopic decompression is between 79% and 81%[10-13]. Signs of perforation or gangrene are indications for emergency surgery[7]. The condition has a tendency to recur in 45%-71% of patients treated conservatively[10-12,14], with a mortality of 7%[10]; therefore, clinicians recommend that patients undergo sigmoid resection, either with a primary anastomosis or Hartmann’s procedure. Both surgeries can be done as emergency procedures, semi-electively, during the patient’s first admission, or as elective procedures during readmission. Despite the high rate of recurrence without surgery, up to 65% of patients do not undergo a prophylactic resection after their first incidence of sigmoid volvulus[10,12,14].
Information about survival and recurrence has not been clearly stated in previous studies[10-14]. Access to civil registration numbers in Denmark gave us unique data about admissions, surgery, and death. Because of Danish recordkeeping practices, each patient can be followed individually over a long period of time, and data can be evaluated with life-table analysis and Kaplan-Meier plotting[15,16].
Patients were identified by searching for the ICD 10 code for volvulus: K56.2. This code includes all cases of intestinal volvulus. Patients with sigmoid volvulus were identified by manual review of the identified medical records.
Data included sex, age, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status classification system type, comorbidities, diagnostics, treatment during first admission, complications, mortality, and recurrence. Date of death was found by linking to the Danish National Death Registry. Information about admissions to other hospitals in the region was found by searching electronic patient records between the years 2000 and 2012.
A definitive diagnosis of sigmoid volvulus was made based upon radiography, sigmoidoscopy, or surgery. Mortality was defined as death within 30 d after intervention or surgery.
Data was recorded in a Microsoft Access database and calculations were performed with Microsoft Excel. Kaplan-Meier plotting and the Mantel-Cox (log-rank) testing were performed using GraphPad Prism software[15-17].
Between 1996 and 2011, a total of 132 patients were diagnosed with volvulus at the Department of Surgery P, Aarhus University Hospital in Denmark. Seventy of these patients had a definitive diagnosis of sigmoid volvulus. Nine sigmoid volvulus patients had surgery in another hospital or were diagnosed before 1996 and were thus excluded from our analysis. The remaining 61 patients became our study subjects (Table 1).
| All patients, n = 61 | |
| Median age, yr (range) | 78 (23-95) |
| Male/female | 40/21 |
| Median BMI (range) | 23 (17-33) |
| Median ASA score (range) | 3 (1-4) |
| Missing ASA scores, n | 19 |
| Comorbidity | |
| Previous abdominal surgery | 14 (23) |
| Diabetes | 5 (8) |
| Cardiovascular disease | 32 (52) |
| Cancer | 5 (8) |
| Neurological | 32 (52) |
| Total | 53 (87) |
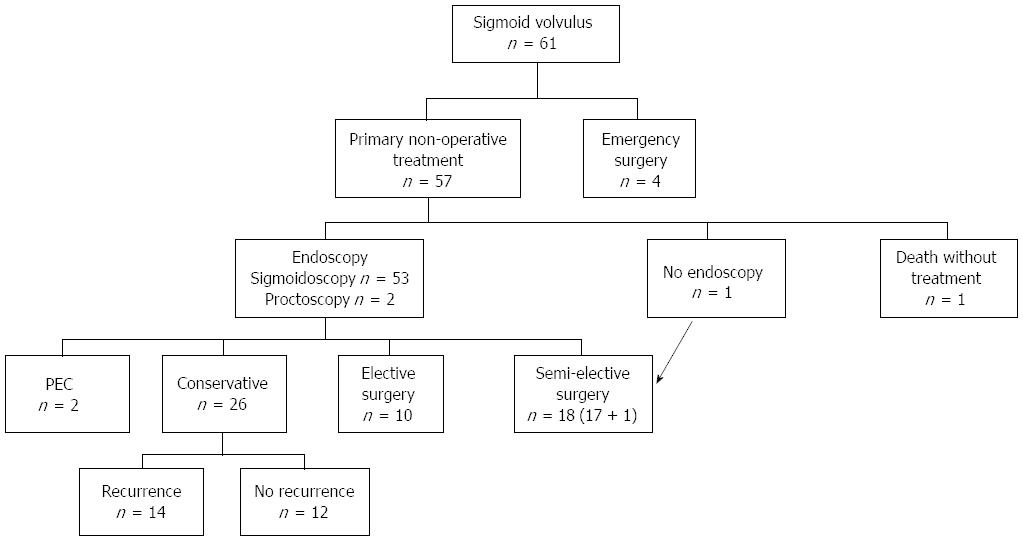
Our subjects’ clinical courses are shown in Figure 1. Four patients (7%) had emergency surgery; among which, 3 had other possible diagnoses (coecal volvulus, malignant stenosis, or ischemia) and 1 had an iatrogenic perforation under sigmoidoscopy (Table 2). One patient with comorbidities died without treatment because of large bowel perforation, and the volvulus condition resolved in another patient after contrast enema. The remaining 55 patients (90%) underwent endoscopy, and 36 of these (65%) were treated with a decompression tube.
| Emergency surgery, n = 4 | Semi-elective surgery, n = 18 | Elective surgery, n = 10 | All patients, n = 32 | |
| Median age, yr (range) | 69 (54-82) | 77 (23-87) | 61 (49-82) | 71 (23-87) |
| Median ASA score (range) | 2 | 3 | 2 | 2 |
| Missing ASA scores, n | 1 | 4 | 1 | 6 |
| Anastomosis: Hartmann | 0:4 | 10:8 | 8:2 | 18:14 |
| Perforation | 1 (25) | 0 | 0 | 1 (3) |
| 30-d mortality | 0 | 6 (33) | 0 | 6 (19) |
| Morbidity | 1 (25) | 5 (36) | 3 (30) | 9 (35) |
Twenty-six patients were conservatively treated without surgery, based on either clinical evaluation or patient preference, even though sigmoid resection was considered the best practice for the management of sigmoid volvulus if the patient’s general condition allowed it. Medical reasons for choosing conservative treatment were mainly advanced age and comorbidities. The remaining patients underwent sigmoid resection, either during the same admission (labeled “semi-elective” surgery, 17 after endoscopy and 1 after contrast enema, n = 18) or during a planned re-admission (labeled “elective” surgery, n = 10). Two patients were deemed unfit for surgery and underwent percutaneous endoscopic colostomy (PEC) and both died after 36 d and 9 mo, respectively.
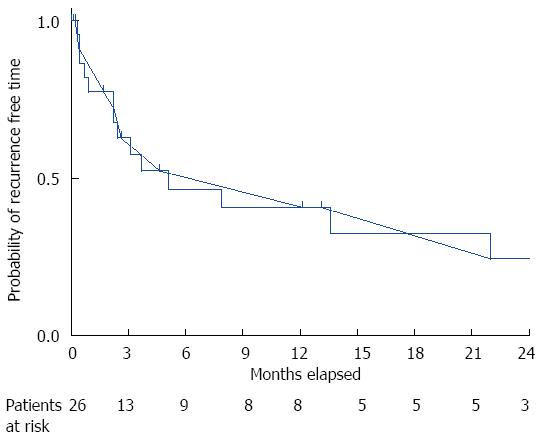
Fourteen of the 26 patients managed conservatively experienced recurrences (Figure 1). Time to recurrence is illustrated in a Kaplan-Meier plot where the accumulated probability of remaining recurrence-free after 3, 6, 12 and 24 mo was 63%, 47%, 41% and 24%, respectively (Figure 2). Eight of the 14 patients with recurrence (57%) had surgery, all semi-electively, with no 30-d mortality. These 8 patients had a median ASA score of 3, a median age of 81 years (range: 49-90 years), and a median time to death or end of the observation period of 33 mo. The 6 patients with recurrence that did not undergo surgery had the same median ASA score of 3 and a median age of 79 years (70-95 years). Median time to death or end of the observation period was 6 mo, and 2 of the 6 patients died within 30 d, meeting the criteria for mortality.
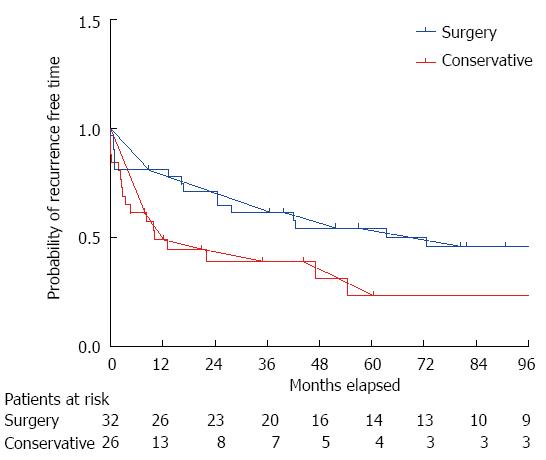
Patients treated conservatively on their first admission for sigmoid volvulus had a poorer survival rate than patients treated surgically on their first admission (95%CI: 3.67-14.37, P = 0.036) as illustrated by the Kaplan-Meier plot in Figure 3. Conservatively treated patients were significantly older and had a significantly higher ASA score than surgically treated patients (Table 3).
| Surgery at first admission and elective surgery, n = 32 | Conservative treatment at first admission, n = 26 | P | |
| Median age, yr (range) | 71 (23-87) | 82 (49-95) | 0.004 |
| Median ASA score | 2 | 3 | 0.012 |
| Missing ASA scores, n | 6 | 12 | - |
| 30-d mortality, n (%) | 6 (19) | 4 (15) | - |
A total of 40 patients (emergency, n = 4; semi-elective, n = 18; elective, n = 10; surgery after recurrence, n = 8) had an operation during the study period, which ran from 1996 to 2012. Only patients undergoing semi-elective surgery died within 30 d, with 3 deaths due to cardiovascular problems, 1 due to anastomotic leakage, 1 due to septicemia without focus, and 1 who had no treatment performed after the recurrence. Fifteen of the 40 patients (38%) had a Hartmann’s procedure and 25 (63%) had primary anastomosis. Patients treated with Hartmann’s procedure had a median age of 72 years (23-87 years) and a median ASA score of 3. Three of the 15 patients (20%) died within 30 d. The group of patients with primary anastomosis had a median age of 74 years (42-90 years) and a median ASA score of 2. One patient (4%) died within 30 d.
The present study is the first international publication on sigmoid volvulus using Kaplan-Meier analysis to illustrate mortality and recurrence. By combining clinical data with data from the Danish death registry, we were able to produce very reliable short and long-term information about outcomes after surgical and conservative treatment. The main finding of this study is that patients treated with surgery had a significantly better survival rate than patients treated conservatively. Furthermore, we found that more than half of the patients treated conservatively experienced a recurrence of their sigmoid volvulus within the first 5 mo. This suggests that patients should be treated with surgery after the first incidence of sigmoid volvulus, unless severe comorbidity prohibits this or emergency surgery is necessary.
The main weakness of the present study is its retrospective design, which makes the external validity low and the conclusions weak. The conservative and the surgical group of patients were significantly different in terms of comorbidity and age, so it is not surprising that long-term survival rates were different. The non-randomized design precludes speculations about whether the conservatively treated group would have survived longer if they had been treated surgically. The main strength of the present study is that the Kaplan-Meier plots give important descriptive information about outcomes in both groups.
Sigmoid volvulus is a serious condition independent of the mode of treatment. The conservatively treated group in our study had a 30-d mortality of 15% (4/26) compared to the 9%-36% reported in other studies[10-14]. We found that the 30-d mortality for the conservatively and surgically treated patients was almost the same (Table 3); however, the prognosis and survival for patients who had surgery was considerably better in the long run compared to those for the conservatively treated patients (Figure 3). An explanation could be that the 2 groups were different in both median age and median ASA score. In spite of this, 8 of the 14 conservatively treated patients with recurrence, all of who were elderly and had a high ASA score, later underwent surgery without 30-d mortality. Neither our group nor Tan et al[10] and Larkin et al[12] found any mortality among patients who underwent surgery after recurrence. This indicates that the better long-term survival for surgically treated patients cannot be exclusively explained by differences in age and ASA scores, and indicates that more patients could have undergone surgery during their first admission.
For patients treated conservatively during their first admission, recurrent volvulus was very likely to occur in the months to follow. The literature reports recurrence rates of 45% to 71%, depending on the length of follow-up[10-14]. Less than half of our conservatively treated patients were free of recurrence after 6 mo; moreover, according to our Kaplan-Meier analysis, only 24% had not experienced a recurrence after 2 years. It has to be noted that this group of patients were either found to be unfit to undergo a sigmoid resection or had refused to undergo such a procedure. It may very well be that too few of our patients were encouraged to undergo surgery during their first admission. The fact that 30-d mortality was zero in the small group of patients that was operated on when they had a recurrence indicates that such encouragement would be appropriate.
There is little doubt, however, that a certain number of patients will never undergo sigmoid resection. Fortunately, promising results have been reported in other studies after the insertion of PEC tubes[18-21], placed with the aid of a colonoscope. Important aspects of therapeutic success are de-rotation, decompression, and fixation. In 1 of our 2 patients treated with PEC insertion, colonoscopic derotation of the sigmoid colon was not achieved, which may be one reason for the early death of this patient. Other studies have reported a fairly low mortality after this procedure (0%-5%)[18-21], so it might be wise to offer PEC tube insertion to patients that would otherwise be treated conservatively as it may improve survival and lower the risk of recurrence. The technical difficulties with derotation may be overcome by combining the colonoscopic procedure with laparoscopy as illustrated in the study by Gordon-Weeks et al[19].
Our data do not enable us to draw conclusions regarding the choice between resection with primary anastomosis or a Hartmann type of resection. We only experienced one anastomotic leak, but our limited results do not allow us to make a general recommendation for either procedure.
In conclusion, If gangrene or perforation is suspected, patients with sigmoid volvulus should undergo emergency surgery. Otherwise, they should undergo emergency sigmoidoscopic decompression and be recommended for surgery if their general condition allows it. The high recurrence rate in conservatively treated patients indicates that more patients should be encouraged to undergo either surgical resection or PEC insertion.
Sigmoid volvulus is the most common type of volvulus and, in general, patients with sigmoid volvulus are institutionalized, elderly, and have significant comorbidities. Initial conservative treatment of sigmoid volvulus is sigmoidoscopy with decompression and detorsion. The disease has a tendency to recur in 45%-71% of conservatively treated patients, so most patients are encouraged to undergo sigmoid resection, either with a primary anastomosis or Hartmann’s procedure. Despite the fact that the incidence of recurrence is high, up to 65% of patients with sigmoid volvulus do not undergo a prophylactic resection after the first incidence of the condition. This study investigated the short- and long-term outcomes of initial treatment with both conservative and surgical methods, and the safety of surgical treatment after recurrence.
The main findings of this study are that patients treated with surgery had a significantly better survival rate than patients treated conservatively, and more than half of the patients treated conservatively experienced a recurrence within the first 5 mo after their initial treatment. Since sigmoid resection after recurrence and percutaneous endoscopic colostomy (PEC) insertion were both effective treatments and did not produce 30-d mortality, even in patients initially considered too physically fragile for surgery. Sigmoid resection or PEC insertion should be considered initial treatments for more patients in the future.
Important information about survival and recurrence was not clearly defined in previous studies. In this retrospective study, each patient was followed individually over a long period of time and the data was evaluated with life-table analysis and Kaplan-Meier plotting. For example, the 30-d mortality for the conservatively and surgically treated patients was almost the same, but the prognosis and survival for patients who had surgery were considerable better in the long run than the prognosis and survival for conservatively treated patients. This is new and important information for clinicians. The literature reports recurrence rates of 45%-71%, depending on the length of follow-up. Less than half of our conservatively treated patients were free of recurrence after 6 mo; moreover, after 2 years, only 24% had not experienced a recurrence according to Kaplan-Meier analysis. The main strength of the present study is that the Kaplan-Meier plots give important descriptive information about outcome in the different groups.
The high recurrence rate after conservative treatment and the significantly better long-term survival rate for patients who underwent surgery indicate that more patients should undergo sigmoid resection after emergency sigmoidoscopic decompression.
Sigmoid volvulus is characterized by an axial twisting of the sigmoid colon at a minimum of 180 degrees.
Notwithstanding the inherent weaknesses of a retrospective study and the small number of patients included in the analysis, this manuscript provides evidence-based proofs of better long-term survival in surgically treated patients. As such, this paper constitutes a notable addition to the literature and will benefit treating clinicians in their clinical management of sigmoid volvulus.
P- Reviewer: Koukoulis G, Rabinowitz SS, Venkatachalam RV S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
| 1. | Kabara JJ, Riggin RM, Kissinger PT. Abnormal levels of urinary catecholamines in dystrophic mice and hamsters. Proc Soc Exp Biol Med. 1976;151:168-172. [PubMed] |
| 2. | Peña AS, Lems-van Kan PH, Kuiper I, van Duijn W, Lamers CB. Measurement of mucosa-specific antibodies against gliadin by a sensitive technique using the biotin-streptavidin system. Acta Gastroenterol Belg. 1986;49:423-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 88] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Bruusgaard C. Volvulus of the sigmoid colon and its treatment. Surgery. 1947;22:466-478. [PubMed] |
| 4. | Grigg MM, Costanzo-Nordin MR, Celesia GG, Kelly MA, Silver MA, Sobotka PA, Robinson JA. The etiology of seizures after cardiac transplantation. Transplant Proc. 1988;20:937-944. [PubMed] |
| 5. | Bhatnagar BN, Sharma CL, Gupta SN, Mathur MM, Reddy DC. Study on the anatomical dimensions of the human sigmoid colon. Clin Anat. 2004;17:236-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Sonnenberg A, Tsou VT, Müller AD. The “institutional colon”: a frequent colonic dysmotility in psychiatric and neurologic disease. Am J Gastroenterol. 1994;89:62-66. [PubMed] |
| 7. | Osiro SB, Cunningham D, Shoja MM, Tubbs RS, Gielecki J, Loukas M. The twisted colon: a review of sigmoid volvulus. Am Surg. 2012;78:271-279. [PubMed] |
| 8. | Margolin DA, Whitlow CB. The Pathogenesis and Etiology of Colonic Volvulus. Semin Colon Rectal Surg. 1999;10:129-138. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Oren D, Atamanalp SS, Aydinli B, Yildirgan MI, Başoğlu M, Polat KY, Onbaş O. An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases. Dis Colon Rectum. 2007;50:489-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 112] [Article Influence: 6.2] [Reference Citation Analysis (1)] |
| 10. | Tan KK, Chong CS, Sim R. Management of acute sigmoid volvulus: an institution’s experience over 9 years. World J Surg. 2010;34:1943-1948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Swenson BR, Kwaan MR, Burkart NE, Wang Y, Madoff RD, Rothenberger DA, Melton GB. Colonic volvulus: presentation and management in metropolitan Minnesota, United States. Dis Colon Rectum. 2012;55:444-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Larkin JO, Thekiso TB, Waldron R, Barry K, Eustace PW. Recurrent sigmoid volvulus - early resection may obviate later emergency surgery and reduce morbidity and mortality. Ann R Coll Surg Engl. 2009;91:205-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Grossmann EM, Longo WE, Stratton MD, Virgo KS, Johnson FE. Sigmoid volvulus in Department of Veterans Affairs Medical Centers. Dis Colon Rectum. 2000;43:414-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Mulas C, Bruna M, García-Armengol J, Roig JV. Management of colonic volvulus. Experience in 75 patients. Rev Esp Enferm Dig. 2010;102:239-248. [PubMed] |
| 15. | Jager KJ, van Dijk PC, Zoccali C, Dekker FW. The analysis of survival data: the Kaplan-Meier method. Kidney Int. 2008;74:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 154] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 16. | Rich JT, Neely JG, Paniello RC, Voelker CC, Nussenbaum B, Wang EW. A practical guide to understanding Kaplan-Meier curves. Otolaryngol Head Neck Surg. 2010;143:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Bewick V, Cheek L, Ball J. Statistics review 12: survival analysis. Crit Care. 2004;8:389-394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 280] [Cited by in RCA: 296] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 18. | Cowlam S, Watson C, Elltringham M, Bain I, Barrett P, Green S, Yiannakou Y. Percutaneous endoscopic colostomy of the left side of the colon. Gastrointest Endosc. 2007;65:1007-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Gordon-Weeks AN, Lorenzi B, Lim J, Cristaldi M. Laparoscopic-assisted endoscopic sigmoidopexy: a new surgical option for sigmoid volvulus. Dis Colon Rectum. 2011;54:645-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Baraza W, Brown S, McAlindon M, Hurlstone P. Prospective analysis of percutaneous endoscopic colostomy at a tertiary referral centre. Br J Surg. 2007;94:1415-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Daniels IR, Lamparelli MJ, Chave H, Simson JN. Recurrent sigmoid volvulus treated by percutaneous endoscopic colostomy. Br J Surg. 2000;87:1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 1.4] [Reference Citation Analysis (0)] |