Published online Jan 28, 2014. doi: 10.3748/wjg.v20.i4.1123
Revised: October 12, 2013
Accepted: November 12, 2013
Published online: January 28, 2014
Processing time: 144 Days and 7.9 Hours
Duodenal duplication cysts are rare congenital anomalies. Duodenal duplication should be considered in the differential diagnosis of patients who present with abdominal symptoms with cystic structures neighboring the duodenum. Here, we present an 8-year-old girl with a duodenal duplication cyst treated with partial cystectomy with mucosal stripping performed laparoscopically. Laparoscopic surgery can be considered as a treatment option for duodenal duplication cysts, especially in extraluminal locations.
Core tip: In duodenal duplication cysts, the endoscopic approach has limitations in extraluminal situations. Endoscopic internal derivation cannot remove the mucosal layer where malignancy mainly occurs, therefore, we propose that laparoscopic surgery can be considered as a treatment option for duodenal duplication cysts, especially in extraluminal locations.
- Citation: Byun J, Oh HM, Kim SH, Kim HY, Jung SE, Park KW, Kim WS. Laparoscopic partial cystectomy with mucosal stripping of extraluminal duodenal duplication cysts. World J Gastroenterol 2014; 20(4): 1123-1126
- URL: https://www.wjgnet.com/1007-9327/full/v20/i4/1123.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i4.1123
Duodenal duplication cysts are rare congenital anomalies, which can appear during the neonatal period or later in life depending on the degree of the gastric outlet obstruction[1]. Classical treatment for duodenal duplication cysts is total resection, but in cases requiring pancreaticoduodenectomy, less-invasive approaches have been proposed[2-4]. Here, we describe the laparoscopic technique for partial resection of duodenal duplication cysts in an 8-year-old girl.
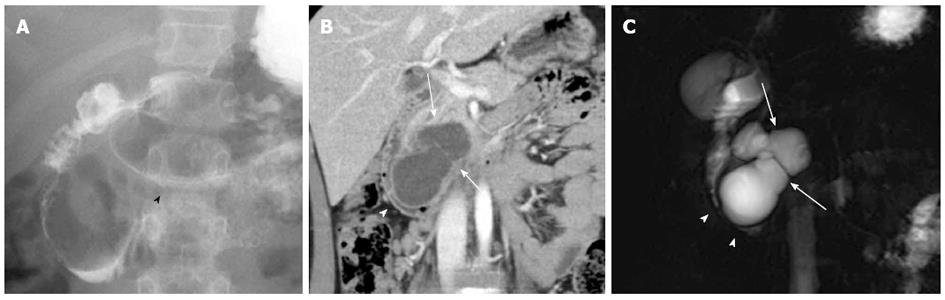
An 8-year-old girl had suffered from intermittent abdominal pain, nausea and vomiting for 2 mo. The patient had no other underlying diseases. The abdomen was flat and no definite mass was palpable. The laboratory studies were normal. The patient did not have jaundice and had normal serum bilirubin level. The tumor markers were not checked before surgery. Abdominal ultrasonography (US) showed 6 cm × 5 cm lobulated retroperitoneal cystic mass, septated between the duodenum and the pancreas. Upper gastrointestinal series revealed luminal narrowing of the second portion of the duodenum (Figure 1A). Abdominal computed tomography (CT) and biliary pancreas magnetic resonance imaging (MRI) showed a multiseptated cystic mass suspected of originating from the uncinate process of the pancreas. Extra compression from this lesion seemed to be causing narrowing of the duodenal lumen (Figure 1B and C). Retroperitoneal lymphangioma of the pancreas was primarily suspected, along with other differential diagnoses including solid and papillary epithelial neoplasms, pancreatoblastoma, unusual cystadenoma, and pancreatic pseudocyst.
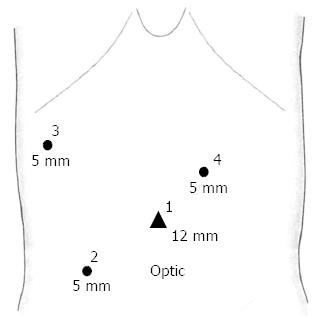
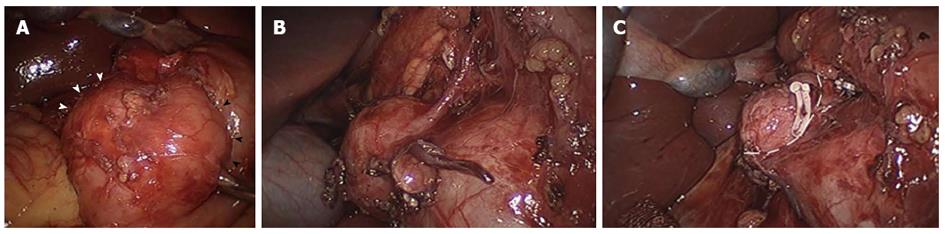
Laparoscopic exploration was performed. The patient was placed in the supine position under general anesthesia and an optical umbilical port was placed under direct vision followed by three additional ports (Figure 2). A Snowden-Pencer Snake Retractor (CareFusion, San Diego, CA, United States) was inserted through port site 3 for liver retraction. After performing a laparoscopic Kocher maneuver, a multiloculated cystic mass was identified in the second portion of the duodenum. The cystic mass originated from the mesenteric border of the duodenum and adhered to the uncinate process of the pancreas (Figure 3A). After adhesiolysis between the cyst and the pancreas, clear demarcation of the cystic surface was identified (Figure 3B). An arterial branch supplying the mass originating from the gastroduodenal artery was ligated with a 5-mm hemoclip and divided (Figure 3C). The proximal border of the mass was easily dissected from duodenum with an ENDOPATH Electrosurgery Probe Plus II System with a Hook electrode (Ethicon Endo-Surgery, Cincinnati, OH, United States), but the distal border was directly attached to the duodenal wall, forming a common wall. A harmonic scalpel (Ethicon Endo-Surgery) was used to resect the mass from the duodenum and the remnant mucosa was cauterized with the ENDOPATH system. The lesion formed a common wall with the duodenum, without communication or fistula. No intraoperative complications were encountered.
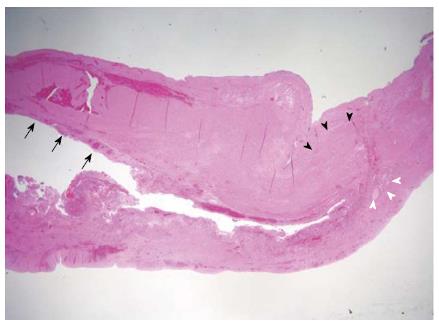
The patient was discharged on Postoperative Day 9 without any complications. Upon histopathological review, a compatible duodenal wall with partially denuded epithelium was consistent with duodenal duplication (Figure 4).
Patients with duodenal duplication cysts present with recurrent nausea, vomiting, abdominal mass, abdominal distension, pancreatitis, and gastrointestinal bleeding[4,5]. Duodenal duplication can be diagnosed with various imaging modalities. The “double-layered wall” of the duodenum seen with US, CT, and endoscopic ultrasound (EUS) are used to reach a diagnosis of duodenal duplication[6-8]. In the present case, the patient had complained of recurrent nausea and vomiting. However, in the US findings, the double-layered wall was not significant, and the lesion seemed to originate from the pancreas in the CT and MR images. Moreover, the lesion showed multiseptations, which turned out to be the folding patterns of the cyst wall upon surgical exploration, and made it difficult to distinguish from other pancreatic tumors, including pancreatic lymphangioma.
The ideal treatment for duodenal duplication cysts is complete surgical resection if their location allows it without endangering the biliopancreatic ducts[4]. However, in cases of duodenal duplication cysts involving important nearby structures, for example, the pancreas or biliary ducts, major surgical procedures like pancreaticoduodenectomy may be required for total resection. This major procedure has a high complication rate resulting in poor quality of life especially in children, therefore, less-invasive approaches, for instance, partial resection or internal marsupialization, have been proposed[2-4]. We have performed partial cystectomy with mucosal stripping without duodenotomy using laparoscopic devices. However, in children, the small abdominal cavity and relatively small organs are limitations to laparoscopic approaches. Compared with conventional open surgery, laparoscopic surgery is less invasive and has more cosmetic advantages if it is performed by an experienced surgeon with the proper equipment.
Endoscopic therapy for duodenal duplication has been suggested recently for minimally invasive treatment. However, the endoscopic approach has limitations for extraluminal cysts. Endoscopic internal derivation cannot remove the mucosal layer where malignancy mainly occurs, therefore, we propose that laparoscopic surgery is a safer method, especially for cases with extraluminal locations[2,9,10].
In summary, although duodenal duplication cysts are rare, they should be considered in the differential diagnosis of patients who present with abdominal symptoms with cystic structures neighboring the duodenum. Laparoscopic partial cystectomy with mucosal stripping can be considered as a treatment option for duodenal duplication cysts even in children.
P- Reviewers: Chiu CC, Shamim D S- Editor: Zhai HH L- Editor: Kerr C E- Editor: Zhang DN
| 1. | Schalamon J, Schleef J, Höllwarth ME. Experience with gastro-intestinal duplications in childhood. Langenbecks Arch Surg. 2000;385:402-405. [PubMed] |
| 2. | Seeliger B, Piardi T, Marzano E, Mutter D, Marescaux J, Pessaux P. Duodenal duplication cyst: a potentially malignant disease. Ann Surg Oncol. 2012;19:3753-3754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Siddiqui AM, Shamberger RC, Filler RM, Perez-Atayde AR, Lillehei CW. Enteric duplications of the pancreatic head: definitive management by local resection. J Pediatr Surg. 1998;33:1117-1120; discussion 1117-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Merrot T, Anastasescu R, Pankevych T, Tercier S, Garcia S, Alessandrini P, Guys JM. Duodenal duplications. Clinical characteristics, embryological hypotheses, histological findings, treatment. Eur J Pediatr Surg. 2006;16:18-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Chen JJ, Lee HC, Yeung CY, Chan WT, Jiang CB, Sheu JC. Meta-analysis: the clinical features of the duodenal duplication cyst. J Pediatr Surg. 2010;45:1598-1606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 87] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Barr LL, Hayden CK, Stansberry SD, Swischuk LE. Enteric duplication cysts in children: are their ultrasonographic wall characteristics diagnostic? Pediatr Radiol. 1990;20:326-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 81] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Antaki F, Tringali A, Deprez P, Kwan V, Costamagna G, Le Moine O, Delhaye M, Cremer M, Devière J. A case series of symptomatic intraluminal duodenal duplication cysts: presentation, endoscopic therapy, and long-term outcome (with video). Gastrointest Endosc. 2008;67:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Okuyama H, Matsuo Y, Fukui Y, Imura K, Kamata S, Okada A. Intrapancreatic duodenal duplication associated with pancreatic pseudocysts. J Pediatr Surg. 1992;27:1573-1574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Jiménez M, Cadière GB, Dapri G, Vasilikostas G, Bruyns J, Capelluto E. Duodenal duplication cyst in an adult: first simultaneous laparoscopic and endoscopic surgery. J Laparoendosc Adv Surg Tech A. 2009;19:207-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Vandenbroucke F, Dagenais M, Létourneau R, Lapointe R, Roy A. Endoscopic treatment of a duodenal duplication cyst. Endoscopy. 2005;37:601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |