Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Oct 21, 2014; 20(39): 14185-14204
Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14185
Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14185
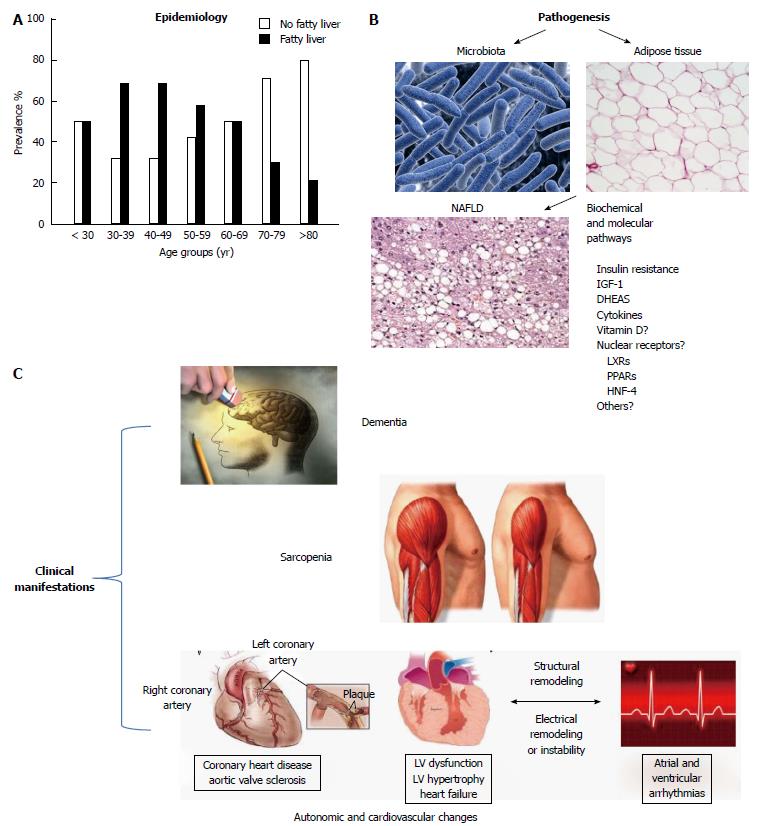
Figure 1 Geriatric nonalcoholic fatty liver disease at a glance (modified from Refs[39,75]).
A: Epidemiology; B: Pathogenesis; C: Clinical manifestations. Schematic representation of chief epidemiological, pathogenic and clinical features of nonalcoholic fatty liver disease (NAFLD) observed in geriatric age based on data critically reviewed in the text. From an epidemiological point of view, NAFLD tends to peak in middle life and its occurrence is reduced in the extreme decades. Pathogenically, altered body fat distribution and changes in gut microbiota predispose to those metabolic changes which tend to be even more closely associated with NAFLD in the elderly than in the young. The biochemical and molecular mechanisms underlying the development of fatty liver may involve insulin resistance and inherent hormonal changes, as well as mediators of inflammation and possibly vitamin D and a number nuclear receptors. Regarding the latter, only indirect evidence can be inferred from the literature (see text for details). Clinically, NAFLD tends to be associated with the typical geriatric syndromes, such as dementia, sarcopenia, autonomic dysfunction, aortic valve sclerosis and autonomic changes predisposing to fatigue, falls and arrhythmia. HNF4: Hepatocyte nuclear factor 4 alpha; IGF-1: Insulin-like growth factor 1; PPAR: Peroxisome proliferator-activated receptor; DHEA: Dehydroepiandrosterone; LXR: Liver X receptor.
- Citation: Bertolotti M, Lonardo A, Mussi C, Baldelli E, Pellegrini E, Ballestri S, Romagnoli D, Loria P. Nonalcoholic fatty liver disease and aging: Epidemiology to management. World J Gastroenterol 2014; 20(39): 14185-14204
- URL: https://www.wjgnet.com/1007-9327/full/v20/i39/14185.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i39.14185