Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14510
Revised: May 15, 2014
Accepted: June 21, 2014
Published online: October 21, 2014
Processing time: 233 Days and 3.2 Hours
Foreign body ingestion is a common complaint in gastrointestinal clinics. It is usually not difficult to diagnose because most of the patients report a definitive history of accidental foreign body ingestion. However, in rare cases, patients do not have a clear history. Thus, the actual condition of the patient is difficult to diagnosis or is misdiagnosed; consequently, treatment is delayed or the wrong treatment is administered, respectively. This report describes a fatal case of esophageal perforation caused by an unknowingly ingested fishbone, which resulted in lower esophageal necrosis, chest cavity infection, posterior mediastinum fester, and significant upper gastrointestinal accumulation of blood. However, his clinical symptoms and imaging data are very similar with esophageal hiatal hernia. Unfortunately, because the patient was too late in consulting a physician, he finally died of chest infection and hemorrhage caused by thoracic aortic rupture. First, this case report underlines the importance of immediate consultation with a physician as soon as symptoms are experienced so as not to delay diagnosis and treatment, and thus avoid a fatal outcome. Second, diagnostic imaging should be performed in the early stage, without interference by clinical judgment. Third, when computed tomography reveals esophageal hiatus hernia with stomach incarceration, posterior mediastinal hematoma, and pneumatosis caused by esophageal, a foreign body should be suspected. Finally, medical professionals are responsible for making people aware of the danger of foreign body ingestion, especially among children, those who abuse alcohol, and those who wear dentures, particularly among the elderly, whose discriminability of foreign bodies is decreased, to avoid dire consequences.
Core tip: Foreign body ingestion is associated with a variety of symptoms and complications, including perforation of the esophagus, perforation of the aorta, embedment in the thyroid gland, and perforation of the carotid artery. However, gastrointestinal accumulation has been rarely reported. The clinical symptoms and imaging data of the patient in the current case report are very similar with esophageal hiatal hernia. In the present case, the patient unknowingly ingested a fishbone shaped similarly to a distorted toothpick. The migrating bone caused lower esophageal perforation and upper gastrointestinal accumulation, an unusual presentation after foreign body ingestion.
- Citation: Lu YP, Yao M, Zhou XY, Huang B, Qi WB, Chen ZH, Xu LS. False esophageal hiatus hernia caused by a foreign body: A fatal event. World J Gastroenterol 2014; 20(39): 14510-14514
- URL: https://www.wjgnet.com/1007-9327/full/v20/i39/14510.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i39.14510
Among adults, the most commonly ingested foreign bodies are fishbones and crushed chicken and duck bones[1]. Smith and Sokolove[2] reported a case of a patient who ingested a chicken bone, while Komninos and Tsiligianni[3] reported a case of a patient who ingested a key. Ingested foreign bodies often penetrate the tonsils, tongue base, epiglottis, valleculae, larynx, pyriform fossa, and esophagus[4-6]. Foreign body ingestion is associated with a variety of symptoms and complications, including perforation of the esophagus, perforation of the aorta, embedment in the thyroid gland, and perforation of the carotid artery[7,8]. However, gastrointestinal accumulation has been rarely reported. In the present case, the patient unknowingly ingested a fishbone similarly shaped to a distorted toothpick. The migrating bone caused lower esophageal perforation and upper gastrointestinal accumulation, an unusual presentation after foreign body ingestion. To our knowledge, this is the first report of upper gastrointestinal accumulation caused by a fishbone as the foreign body without the patient being aware of its accidental ingestion.
A 53-year-old Chinese man was admitted to our hospital owing to low back pain that persisted for 8 d, which was aggravated by general abdomen pain since 3 d before admission. Eight days before admission, the patient began to sense a persistent low back pain without an obvious precipitating factor. Three days before admission, the symptoms gradually worsened, with the onset of total abdominal pain accompanied by nausea, vomiting (hemorrhagic), decreased flatulence, and the inability to lie down because of intolerable swelling pain. The patient did not report any history of accidental foreign body ingestion. On physical examination, the patient’s blood pressure was 106/62 mm Hg; heart rate, 97 beats/min; and respiration rate, 22 breaths/min. He was conscious upon admission, with a painful facial expression and pale lips. Respiratory sound was weak and chest percussion produced a slightly turbid sound. Abdominal inspection revealed obvious swelling and no gastric and intestinal convexity or varicose vein in the abdominal wall. Auscultation revealed that the low-bowel sound occurred 1-3 times/min, with occasional gurgling. On palpation of the upper abdomen, muscle tension, tenderness, and obvious rebound tenderness were observed. Percussion of the abdomen produced a tympany, without a change in percussion note on alteration of the position.
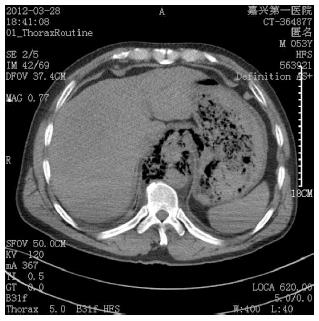
Computed tomography (CT) scans of the chest and anacardium revealed that the posterior mediastinum was broadened and that a portion of the stomach was embedded in the posterior mediastinum (Figure 1). The stomach itself was perforated. The texture of the lower lungs became thickened, with segmental consolidation. Both sides of the pleural cavity were arc-shaped and had near-water density. The right pleural effusion was more severe than the left pleural effusion. On the basis of the CT findings, esophageal hiatus hernia with stomach incarceration was diagnosed, accompanied by perforation of the stomach, bilateral pleural effusion, atelectasis (bilateral lower lobes), and gas collected in the right pleural cavity.
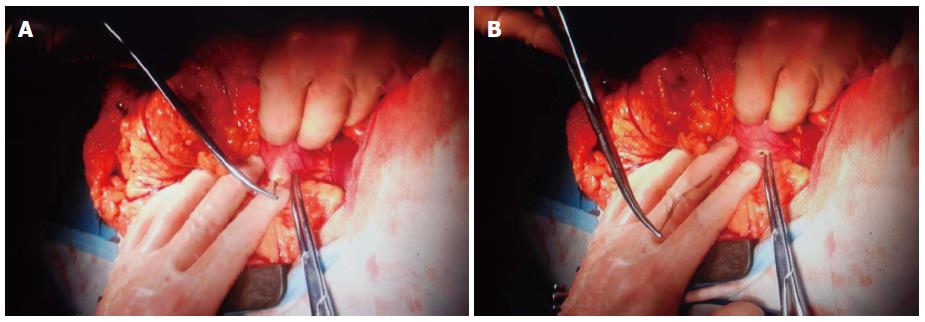
According to the clinical manifestations and CT scans, the patient had an esophageal hiatus hernia with stomach incarceration, acute peritonitis, pleural effusion, necrosis, and stomach perforation. After the patient and his family provided informed consent, the patient underwent an exploratory laparotomy under general anesthesia in March 2012. On examination by laparotomy, we found that the diaphragmatic muscle was intact and that the hiatus esophagus was not expanded. However, the stomach and small intestine were filled with blood. A hard irregular strip was in contact with the stomach. After the stomach wall was cut, an approximately 3-mm (the widest point) × 57-mm irregular fishbone (with pointed ends) was removed (Figure 2A, B), with a large number of blood clots of an approximately 1600-mL total volume (Figure 3). After closure of the abdominal cavity, we performed an exploratory thoracotomy. Because 8 d had elapsed, the lower esophagus had necrotized; in addition, turbid bloody fluid, and a large number of blood clots and pus had accumulated in the chest cavity and posterior mediastinum, respectively. We removed approximately 500 mL of turbid bloody fluid and several blood clots and pus. After flushing the chest cavity, we inserted drainage tubes in the mediastinum and chest cavity. We had intended to perform an esophagectomy after his general condition improved, as his vital signs were unstable and so the patient could not initially tolerate the complex operation.
The following postoperative diagnoses were made: lower esophageal perforation, upper gastrointestinal massive accumulation of blood, and posterior mediastinal hematoma with fester caused by the foreign body. The patient was admitted to the intensive care unit where he received antibiotic and symptomatic treatments. In ICU, septic shock was corrected, and vital signs tended to stability. To further control the infection, we had intended to perform surgery where the perforated esophagus met his stomach, which we would have implemented in two stages. However, the patient died 3 d later owing to severe hemorrhage due to the thoracic aortic rupture.
In the present case, the patient swallowed a hard thick fishbone with sharp ends. The fishbone lacerated the blood vessels of the stomach and esophagus, and caused massive upper gastrointestinal accumulation and lower esophageal perforation. A large amount of blood accumulated in the gastric bowel cavity, which repressed and stimulated the gastrointestinal wall to cause sympathetic hyperexcitability, inhibition of intestinal smooth muscle relaxation, and weakening of intestinal movement, which in turn caused paralytic ileus. Blood and gas migrated from the esophagus through the esophageal holes into the posterior mediastinum, causing blood accumulation and pneumatosis. CT revealed them abreast of the stomach bubble, which was compatible with esophageal hiatus hernia with stomach incarceration (Figure 1). Therefore, the disease was misdiagnosed as esophageal hiatus hernia. However, the symptoms on presentation proved otherwise, given the fact that the patient unknowingly ingested a foreign body, causing a first-onset symptom of low back pain, which was gradually aggravated by general abdomen pain accompanied by nausea, vomiting (hemorrhagic), decreased flatulence, and inability to lie down due to intolerable pain.
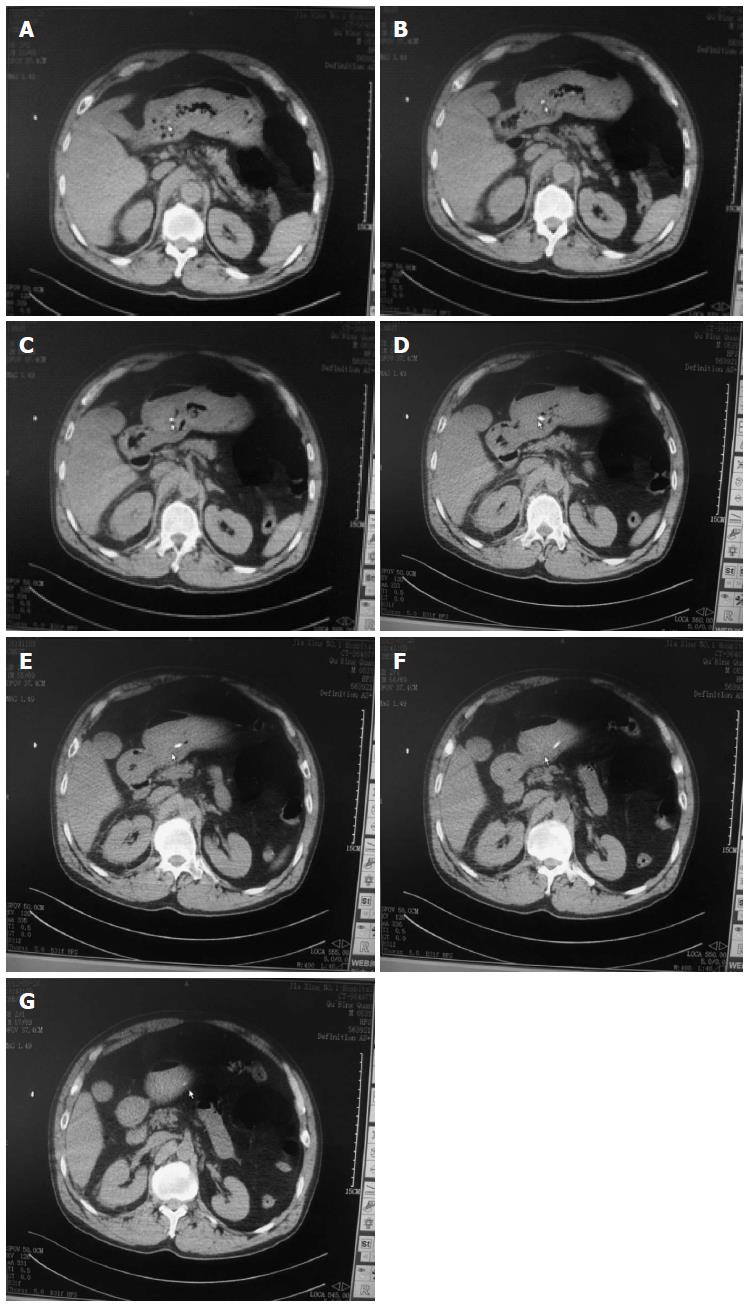
After the operation, we carefully reviewed the patient’s thin-layer (5 mm/layer) scan obtained by thoracic abdominal CT and found that the fishbone obliquely penetrated 7 layers of the stomach wall (Figure 4).
On the basis of our findings from the present case, we gathered the following inferences: First, public awareness should be raised on the importance of immediately consulting a physician as soon as symptoms are experienced so as not to delay diagnosis and treatment, and avoid a fatal outcome. Second, medical professionals are responsible for making people aware of the danger of foreign body ingestion, especially among children, those who abuse alcohol, and those who wear dentures, particularly among the elderly, whose discriminability of foreign bodies is decreased, to avoid dire consequences. Third, diagnostic imaging should be performed at an early stage to guide clinical diagnosis, without interference by clinical judgment. Finally, when CT reveals esophageal hiatus hernia with stomach incarceration, esophageal perforation caused by a foreign body should be suspected. The medical history of the patient should be repeatedly reviewed, and the CT scan should be carefully reviewed and interpreted. To confirm the diagnosis, thin-layer CT should be performed for the upper digestive tract. In this case, the hard thick fishbone was difficult to digest. Fortunately, the fishbone settled in the stomach. If it entered the intestines, exploratory operation and clinical diagnosis would have been more difficult to perform, making it impossible to obtain a definite diagnosis.
A 53-year-old Chinese man presented with back pain and general abdomen pain.
Dullness to percussion, decreased breath sounds in the lungs, and obvious abdominal swelling on inspection.
Esophageal hiatus hernia, Pyothorax, Paralytic ileus.
WBC12.2 × 109/L; HGB 7.8 mg/dL. Prothrombin chart was within normal limits.
Computed tomography (CT) scans of the chest and anacardium revealed that the posterior mediastinum was broadened and that a portion of the stomach was embedded in the posterior mediastinum. The stomach has perforated. Both sides of the pleural cavity were arc-shaped and had near-water density. The right pleural effusion was more severe than the left pleural effusion.
The patient underwent surgical treatment under general anesthesia.
It is rare for significant upper gastrointestinal accumulation of blood and mediastinal empyema to be caused by a foreign body.
Diagnostic imaging should be performed at an early stage to guide clinical diagnosis, without interference by clinical judgment.
This article analyzes the cause of a misdiagnosis by the clinical manifestations and CT examination after the ingestion of foreign bodies.
P- Reviewer: Shim CS S- Editor: Qi Y L- Editor: Rutherford A E- Editor: Liu XM
| 1. | Leong HK, Chan RK. Foreign bodies in the upper digestive tract. Singapore Med J. 1987;28:162-165. [PubMed] |
| 2. | Smith TS, Sokolove PE. Pharyngeal foreign body. J Emerg Med. 2001;21:65-66. [PubMed] |
| 3. | Komninos ID, Tsiligianni IG. Foreign body ingestion mimicking irritable bowel syndrome: a case report. J Med Case Rep. 2010;4:244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Tan AK, Hsu PP, Lu PK. Self-extrusion of a foreign body from the upper digestive tract to the skin. J Laryngol Otol. 2004;118:242-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Pang KP, Pang YT. A rare case of a foreign body migration from the upper digestive tract to the subcutaneous neck. Ear Nose Throat J. 2002;81:730-732. [PubMed] |
| 6. | Al-Sebeih K, Abu-Shara KA, Sobeih A. Extraluminal perforation complicating foreign bodies in the upper aerodigestive tract. Ann Otol Rhinol Laryngol. 2010;119:284-288. [PubMed] |
| 7. | Osinubi OA, Osiname AI, Pal A, Lonsdale RJ, Butcher C. Foreign body in the throat migrating through the common carotid artery. J Laryngol Otol. 1996;110:793-795. [PubMed] |
| 8. | Lim CT, Quah RF, Loh LE. A prospective study of ingested foreign bodies in Singapore. Arch Otolaryngol Head Neck Surg. 1994;120:96-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (0)] |