Published online Apr 21, 2014. doi: 10.3748/wjg.v20.i15.4377
Revised: August 6, 2013
Accepted: September 13, 2013
Published online: April 21, 2014
AIM: To investigate the nature and significance of unexpected positron emission tomography with fluorodeoxyglucose (FDG-PET) uptake within the gastrointestinal tract (GIT).
METHODS: Patients with unexpected FDG-PET findings in the GIT were evaluated. All patients had a previous confirmed malignancy, either solid or lymphoproliferative. The radiologic reports were performed by experienced radiologists with an exclusive PET expertise. Endoscopy, i.e., esophagogastroduodenoscopy (EGD) and colonoscopy, and histopathological evaluation of all findings was performed in all patients in accordance to the FDG-PET results. The findings from each of these modalities were compared to each other. Both clinically significant and insignificant findings were assessed.
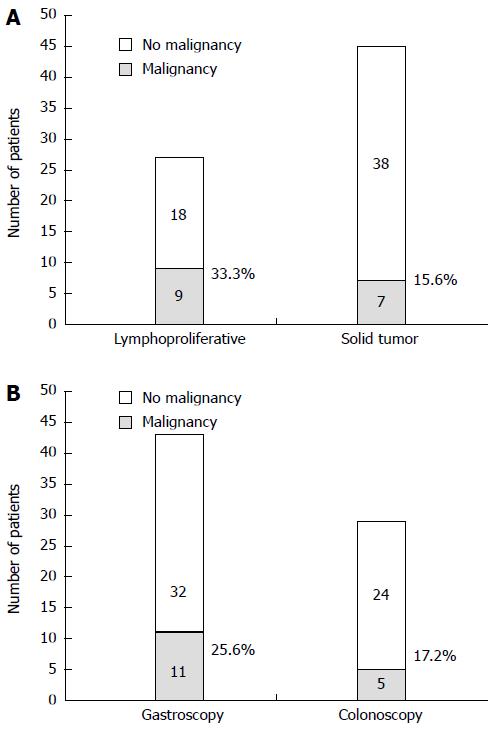
RESULTS: Seventy-two patients were endoscopically evaluated. Twenty-seven patients (37.5%) had primarily a lymphoproliferative tumor and 45 (62.5%) had solid tumors. In 50 patients (69.4%) the endoscopic examination revealed lesions in the same anatomical areas as the FDG-PET findings. Among these 50 patients, malignant and premalignant lesions i.e., adenomatous polyps were found in 16 (32%) and 9 (18%) patients, respectively. Inflammation was noted in an additional 20 patients (40%). Compared to primary solid tumors, a background of primary lymphoproliferative malignancy was more likely to reveal an additional primary malignancy (15.6% vs 33.3%, respectively, P < 0.01). EGD compared to colonoscopy, revealed altogether 11 (25.6%) new malignancies compared to 5 (17.2%), respectively, P = 0.12. No GIT clinically significant findings were overseen by the FDG-PET.
CONCLUSION: Unexpected FDG uptake in the GIT is commonly encountered and may contain significant findings. Endoscopy evaluation is justified in order to detect these additional findings.
Core tip: Positron emission tomography with fluorodeoxyglucose (FDG-PET) is gradually gaining acceptance as a first line radiological modality for both solid and hematological malignancies. While both technology and expertise is improving, incidental findings are more frequently encountered. The gastrointestinal tract is a common source for these unexpected findings. In this manuscript we assessed the significance of these findings and correlated them with upper and lower endoscopy findings. Surprisingly, we encountered much clinical significant information. More so, the FDG-PET was considerably sensitive to gastrointestinal findings. These results suggest that gastrointestinal incidental findings should be evaluated.
- Citation: Goldin E, Mahamid M, Koslowsky B, Shteingart S, Dubner Y, Lalazar G, Wengrower D. Unexpected FDG-PET uptake in the gastrointestinal tract: Endoscopic and histopathological correlations. World J Gastroenterol 2014; 20(15): 4377-4381
- URL: https://www.wjgnet.com/1007-9327/full/v20/i15/4377.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i15.4377
Positron emission tomography (PET) with fluorodeoxyglucose (FDG) has recently been established as a diagnostic tool for the evaluation of patients with suspected or confirmed malignancy[1]. The normal distribution of 18-F FDG uptake has been described in both children and adults[2-4]. A number of physiologic variants are commonly encountered, including normal physiologic uptake in the head and neck, heart, breast, liver, spleen, gastrointestinal tract (GIT), genito-urinary system, bone marrow, muscles, and brown adipose tissue. Benign lesions with increased 18-F FDG uptake are commonly seen and are frequently misinterpreted as malignancies[5-7]. 18-F FDG is glucose analog labeled with a positron-emitting isotope, F (fluorine)-18. It is transported into the cells by glucose transporters, subsequently phosphorylated by hexokinase and trapped within the cell[8]. Malignant tissues accumulate 18-FDG more rapidly than normal tissues due to their increased glucose metabolism rate, increased expression of glucose transporters, and highly active hexokinase bound to tumor mitochondrial compared to normal tissue[9]. 18-F FDG uptake is also known to occur in nonmalignant conditions, mainly inflammation and infection[10]. Increased uptake in inflammation is due to an increased number of glucose transporters[11]. Imaging of inflammation with 18-F FDG PET is also based on the fact that infiltrated granulocytes and tissue macrophages use glucose as an energy source[12]. 18-F FDG uptake in the normal GIT is highly variable and can range from mild to intense with a focal, diffuse, or segmental distribution. The origin of 18-F FDG uptake in the GIT is not fully understood and is most likely multifactorial. Many nonmalignant conditions in the GIT can influence 18-F FDG uptake. Patients with esophagitis caused by gastroesophageal reflux disease or due to radiation therapy may reveal marked uptake in the esophagus. Barrett’s esophagus, a premalignant esophageal finding, may also demonstrate increased uptake in the distal esophagus. Gastric uptake may be associated with Helicobacter pylori infection[13]. Differentiating malignancy or inflammation from a normal variant is quite challenging in colonic uptake. 18-F FDG uptake is also associated with Crohn’s disease (CD), autoimmune pancreatitis, liver and gastrointestinal neoplasms[14-19]. Long-segment diffuse uptake in the GIT is most often associated with physiological uptake, whereas focal uptake in the GIT is more likely to be considered a pathological finding[20].
PET imaging using 18-F FDG (FDG-PET) is well accepted in the imaging work-up or follow-up of many malignancies[1,20]. Incidental or unexpected FDG uptake in the GIT is not rare[21-23], and the significance of such uptake in patients with suspected or confirmed malignancy is yet to be established[24]. The aim of this study was to retrospectively assess the significance of FDG uptake in the gastrointestinal tract in patients who underwent PET-computer tomography (CT) due to a preexisting malignancy.
A dual center retrospective study conducted between October 2009 to December 2011, included 72 patients who underwent a FDG PET-CT scan due to a confirmed malignancy. Patients who were found to have incidental uptake in the GIT were included in the study. Primary malignancy in any solid tumor or hematologic malignancies were included. Patients whose primary malignancy was in the GIT, i.e., colorectal, gastric or esophageal cancer who demonstrated increased uptake in the area of the primary malignancy were excluded. All participants underwent FDG PET-CT following a 6 h fast. In selected cases intravenous furosemide was administered to enhance urinary clearance of excreted FDG. These cases were chosen according to the discretion of the radiologist performing the examination. Intravenous FDG was given at doses that ranged between 185 to 444 MBq. Unenhanced CT scan was routinely obtained for attenuation correction and for diagnostic purposes. PET and PET-CT scans were reviewed on a computer workstation using a 3D-volume and obtaining coronal, sagittal, and trans-axial views by a PET-accredited nuclear physician. The radiographs were all interpreted by a doctor with a minimum of five year experience. Additionally, all cases were presented at a forum which included very experienced radiology experts in PET-CT. The clinical data of all participants were available to the nuclear physician performer. Incidental GIT uptake was the primary inclusion criteria into the study.
Esophagogastroduodenoscopy (EGD) was conducted in all patients with any PET finding that correlated with the upper GIT. A full colonoscopy was performed when findings suggested a lower GIT lesion. All procedures were carried out by an accredited gastroenterologist. The examination was directed to correspond with the FDG uptake in the GIT; if any endoscopic irregularity was detected, multiple biopsies were taken for histopathological analysis. The histopathologic diagnoses were grouped as malignant lesion, premalignant lesion (polyps with any degree of dysplasia), or as inflammation. The outcome was measured as the correlation between the imaging data compared to the endoscopic and histopathology findings.
Case details were computerized and analyzed using SPSS version 17.0 software (Chicago, IL, United States). Data was analyzed using a standard unpaired two-tailed Student’s t-test. All P values were two-sided and considered statistically significant if < 0.05.
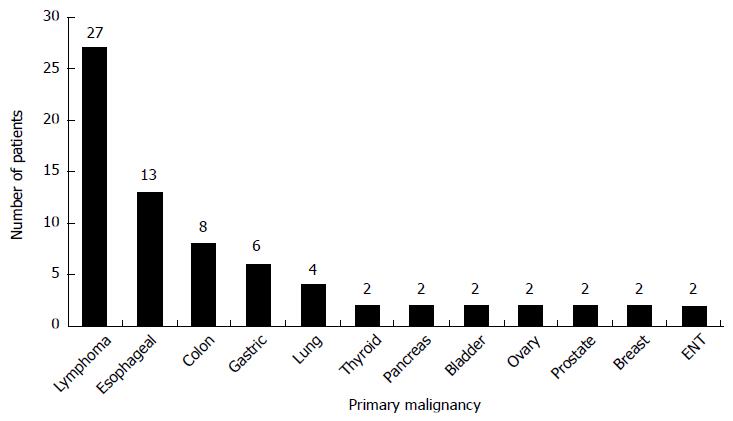
The study population comprised of 72 patients (38 male, 34 female) with a mean age of 62 ± 7 years (range 32-86 years) who were diagnosed with various types of malignancies. The origin of the primary malignancy is listed in Figure 1. Twenty-seven patients (37.5%) had a lymphoproliferative tumor and 45 (62.5%) had solid tumors. Forty-seven patients had undergone surgical intervention and 34 were receiving chemotherapy and/or radiotherapy. Forty-three patients underwent EGD and 29 patients underwent colonoscopy. No participant underwent both examinations.
Fifty patients (69.4%) had a positive endoscopic finding corresponding to the PET-FDG uptake. Among them, 16 (32%) were found to have a malignant lesion and 9 (18%) had a premalignant lesion (i.e., polyps). 19 (38%) patients were found to have an inflammation other than inflammatory bowel disease such as gastritis, duodenitis or nonspecific colitis, and 1 patient (2%) had findings compatible with CD. Five patients (10%) had an endoscopic impression of an irregularity but the histological findings were normal. Excluding these 5 patients with a normal biopsy a total of 45 patients (62.5%) had a significant endoscopic finding corresponding to the FDG uptake. Among the 16 patients with new malignancies, 4 had adenocarcinoma of the stomach, 5 were diagnosed with stomach lymphoma, 2 were found to have adenocarcinoma of the esophagus, and 4 were identified with colorectal cancer. Carcinoma in-situ was found in another patient. Premalignant lesions, i.e., polyps in the colon were found in 9 patients, all corresponding to the PET-FDG uptake. A total of 25/72 patients (34.7%) were diagnosed with malignant or premalignant lesions in areas corresponding to the FDG uptake. 12 (18%) patients had additional endoscopic findings which were not detected by the PET-FDG examination. All of these findings were small polyps less than 5 mm. No malignant lesions were unidentified by the PET-FDG uptake. Among the 72 participants, 27 (37.5%) had a primary lymphoproliferative malignancy, while 45 (62.5%) had a primary solid tumor.
Comparing the primary lymphoproliferative group to the primary solid tumor group, a new malignancy was found in 9/27 (33%) and 7/45 (15.5%), respectively, (P < 0.01) (Figure 2A). When comparing the diagnostic yield of EGD vs colonoscopy, 43/72 (59.7%) underwent EGD and 29/72 (40.3%) underwent a colonoscopy. Eleven malignancies were found by EGD, with a diagnostic yield of 25.6%. Colonoscopy revealed 5 malignancies achieving a diagnostic yield of 17.2% (P = 0.12) (Figure 2B). The difference was not statistically significant.
FDG-PET has been successfully used to aid in the diagnosis, staging, and monitoring of variable malignancies[1,3]. Unfortunately increased FDG uptake is not specific to cancerous cells[5-7]. Accordingly, FDG-PET has a low specificity. FDG is accumulated in several types of inflammatory cells such as lymphocytes, neutrophils, and macrophages due to their increased glucose metabolism[10]. Thus in addition to identification of malignant tumors, the possibility of false-positive findings must be kept in mind to prevent over diagnosis and therapeutic mistakes. Histological analysis is used to distinguish between malignancies and other causes.
Several large sample size studies have shown that FDG-PET is a useful tool for detecting premalignant and malignant lesions. Gutman et al[25] reviewed a series of 1716 PET-CT scans of patients with various malignant diseases other than colorectal cancer and found focal FDG uptake in the colon in 20 patients. These foci were found to be correspondent to three carcinomas and 10 adenomas found during colonoscopy. Israel et al[26] found 58 foci or intense FDG uptake in the GIT in a series of PET-CT scans of 4390 patients. Among the 34 patients who underwent GIT studies, 24 (71%) had abnormal findings, including malignant and premalignant lesions.
This study shows a higher rate of FDG uptake in the GIT than found in previous studies. A partial explanation lies in the advances in the technology and equipment combined with a higher level of interpretation expertise. Additional multifactor explanations are: age, primary malignancy and indication for the exam, which among others may influence GIT uptake.
Our results indicate that patients with a primary lymphoproliferative or solid malignancy with a focal FDG uptake are at a higher risk for an additional primary malignancy. As many as one third of these findings may have a clinical significance and up to one fifth may provide a complete new diagnosis. Primary lymphoproliferative disease adds a considerable risk. As this tool is increasingly being accepted as a primary work up method for both diagnostic and follow up purposes, the likelihood for incidental findings rises. Upper GIT lesions were found to be slightly more specific for malignancy than lower GIT lesions. Premalignant findings were more prevalent in colonoscopy examinations, as expected in the general population. Interestingly, no malignant or significant premalignant findings were found at endoscopy at areas other than those detected by PET-PDG. These findings emphasize the importance and significance of PET-CT findings in the GIT.
Technological advances may lead to better differentiation between physiological and significant pathological findings. Currently the recommendation for patients with an incidental FDG uptake in the GIT should be a complete GIT workup.
In summary, unexpected FDG uptake in the GIT is commonly encountered. Significant findings may be exposed by further evaluation. Endoscopy and pathology evaluation is justified in order to detect these additional findings.
Positron emission tomography with fluorodeoxyglucose (FDG-PET) has been successfully used to aid in the diagnosis, staging, and monitoring of variable malignancies. Unfortunately increased FDG uptake is not specific to cancerous cells.
Several large sample size studies have shown that FDG-PET is a useful tool for detecting premalignant and malignant lesions. These foci were found to be correspondent to three carcinomas and 10 adenomas found during colonoscopy.
This study shows a higher rate of FDG uptake in the gastrointestinal tract than found in previous studies. A partial explanation lies in the advances in the technology and equipment combined with a higher level of interpretation expertise.
The results indicate that patients with a primary lymphoproliferative or solid malignancy with a focal FDG uptake are at a higher risk for an additional primary malignancy.
This paper a very interesting manuscript, well done and well written and of potential interest for the readers. The high sensitivity and specificity in finding new pathologies during follow up is impressive.
P- Reviewers: Shoenfeld Y, Storto G, Wang FZ S- Editor: Zhai HH L- Editor: A E- Editor: Zhang DN
| 1. | Gambhir SS, Czernin J, Schwimmer J, Silverman DH, Coleman RE, Phelps ME. A tabulated summary of the FDG PET literature. J Nucl Med. 2001;42:1S-93S. [PubMed] [Cited in This Article: ] |
| 2. | Hillner BE, Siegel BA, Liu D, Shields AF, Gareen IF, Hanna L, Stine SH, Coleman RE. Impact of positron emission tomography/computed tomography and positron emission tomography (PET) alone on expected management of patients with cancer: initial results from the National Oncologic PET Registry. J Clin Oncol. 2008;26:2155-2161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 296] [Cited by in F6Publishing: 306] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 3. | Tatsumi M, Miller JH, Wahl RL. 18F-FDG PET/CT in evaluating non-CNS pediatric malignancies. J Nucl Med. 2007;48:1923-1931. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Storto G, Nicolai E, Salvatore M. [18F]FDG-PET-CT for early monitoring of tumor response: when and why. Q J Nucl Med Mol Imaging. 2009;53:167-180. [PubMed] [Cited in This Article: ] |
| 5. | Ahmad Sarji S. Physiological uptake in FDG PET simulating disease. Biomed Imaging Interv J. 2006;2:e59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Nakamoto Y, Tatsumi M, Hammoud D, Cohade C, Osman MM, Wahl RL. Normal FDG distribution patterns in the head and neck: PET/CT evaluation. Radiology. 2005;234:879-885. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 203] [Cited by in F6Publishing: 212] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 7. | Cook GJ, Wegner EA, Fogelman I. Pitfalls and artifacts in 18FDG PET and PET/CT oncologic imaging. Semin Nucl Med. 2004;34:122-133. [PubMed] [Cited in This Article: ] |
| 8. | Timmers HJ, Chen CC, Carrasquillo JA, Whatley M, Ling A, Eisenhofer G, King KS, Rao JU, Wesley RA, Adams KT. Staging and functional characterization of pheochromocytoma and paraganglioma by 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography. J Natl Cancer Inst. 2012;104:700-708. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 188] [Cited by in F6Publishing: 176] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 9. | Zhuang H, Alavi A. 18-fluorodeoxyglucose positron emission tomographic imaging in the detection and monitoring of infection and inflammation. Semin Nucl Med. 2002;32:47-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 412] [Cited by in F6Publishing: 422] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 10. | Love C, Tomas MB, Tronco GG, Palestro CJ. FDG PET of infection and inflammation. Radiographics. 2005;25:1357-1368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 338] [Cited by in F6Publishing: 357] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 11. | Basu S, Kumar R, Alavi A. PET and PET-CT imaging in infection and inflammation: its critical role in assessing complications related to therapeutic interventions in patients with cancer. Indian J Cancer. 2010;47:371-379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Kubota R, Yamada S, Kubota K, Ishiwata K, Tamahashi N, Ido T. Intratumoral distribution of fluorine-18-fluorodeoxyglucose in vivo: high accumulation in macrophages and granulation tissues studied by microautoradiography. J Nucl Med. 1992;33:1972-1980. [PubMed] [Cited in This Article: ] |
| 13. | de Groot M, Meeuwis AP, Kok PJ, Corstens FH, Oyen WJ. Influence of blood glucose level, age and fasting period on non-pathological FDG uptake in heart and gut. Eur J Nucl Med Mol Imaging. 2005;32:98-101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 90] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Nakajo M, Jinnouchi S, Fukukura Y, Tanabe H, Tateno R, Nakajo M. The efficacy of whole-body FDG-PET or PET/CT for autoimmune pancreatitis and associated extrapancreatic autoimmune lesions. Eur J Nucl Med Mol Imaging. 2007;34:2088-2095. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Cook GJ, Fogelman I, Maisey MN. Normal physiological and benign pathological variants of 18-fluoro-2-deoxyglucose positron-emission tomography scanning: potential for error in interpretation. Semin Nucl Med. 1996;26:308-314. [PubMed] [Cited in This Article: ] |
| 16. | Nakamoto Y, Saga T, Ishimori T, Higashi T, Mamede M, Okazaki K, Imamura M, Sakahara H, Konishi J. FDG-PET of autoimmune-related pancreatitis: preliminary results. Eur J Nucl Med. 2000;27:1835-1838. [PubMed] [Cited in This Article: ] |
| 17. | Ozaki Y, Oguchi K, Hamano H, Arakura N, Muraki T, Kiyosawa K, Momose M, Kadoya M, Miyata K, Aizawa T. Differentiation of autoimmune pancreatitis from suspected pancreatic cancer by fluorine-18 fluorodeoxyglucose positron emission tomography. J Gastroenterol. 2008;43:144-151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 110] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 18. | Seo S, Hatano E, Higashi T, Hara T, Tada M, Tamaki N, Iwaisako K, Ikai I, Uemoto S. Fluorine-18 fluorodeoxyglucose positron emission tomography predicts tumor differentiation, P-glycoprotein expression, and outcome after resection in hepatocellular carcinoma. Clin Cancer Res. 2007;13:427-433. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 147] [Cited by in F6Publishing: 151] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 19. | Khan MA, Combs CS, Brunt EM, Lowe VJ, Wolverson MK, Solomon H, Collins BT, Di Bisceglie AM. Positron emission tomography scanning in the evaluation of hepatocellular carcinoma. J Hepatol. 2000;32:792-797. [PubMed] [Cited in This Article: ] |
| 20. | Hustinx R, Bénard F, Alavi A. Whole-body FDG-PET imaging in the management of patients with cancer. Semin Nucl Med. 2002;32:35-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 157] [Cited by in F6Publishing: 159] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 21. | Jati A, Tatlı S, Morgan JA, Glickman JN, Demetri GD, Van den Abbele A, Silverman SG. Imaging features of bone metastases in patients with gastrointestinal stromal tumors. Diagn Interv Radiol. 2012;18:391-396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Kamel EM, Thumshirn M, Truninger K, Schiesser M, Fried M, Padberg B, Schneiter D, Stoeckli SJ, von Schulthess GK, Stumpe KD. Significance of incidental 18F-FDG accumulations in the gastrointestinal tract in PET/CT: correlation with endoscopic and histopathologic results. J Nucl Med. 2004;45:1804-1810. [PubMed] [Cited in This Article: ] |
| 23. | Kostakoglu L, Hardoff R, Mirtcheva R, Goldsmith SJ. PET-CT fusion imaging in differentiating physiologic from pathologic FDG uptake. Radiographics. 2004;24:1411-1431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 149] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 24. | Mainenti PP, Iodice D, Segreto S, Storto G, Magliulo M, De Palma GD, Salvatore M, Pace L. Colorectal cancer and 18FDG-PET/CT: what about adding the T to the N parameter in loco-regional staging? World J Gastroenterol. 2011;17:1427-1433. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 20] [Cited by in F6Publishing: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Gutman F, Alberini JL, Wartski M, Vilain D, Le Stanc E, Sarandi F, Corone C, Tainturier C, Pecking AP. Incidental colonic focal lesions detected by FDG PET/CT. AJR Am J Roentgenol. 2005;185:495-500. [PubMed] [Cited in This Article: ] |
| 26. | Israel O, Yefremov N, Bar-Shalom R, Kagana O, Frenkel A, Keidar Z, Fischer D. PET/CT detection of unexpected gastrointestinal foci of 18F-FDG uptake: incidence, localization patterns, and clinical significance. J Nucl Med. 2005;46:758-762. [PubMed] [Cited in This Article: ] |