Published online Mar 21, 2014. doi: 10.3748/wjg.v20.i11.3056
Revised: December 10, 2013
Accepted: January 8, 2014
Published online: March 21, 2014
Processing time: 157 Days and 22.2 Hours
We report a case of Valsalva retinopathy associated with esophagogastroduodenoscopy (EGD) under propofol sedation. A 43-year-old woman who had no previous history of systemic or ocular disease presented with a complaint of decreased vision in her left eye, which developed one day after EGD under propofol sedation. According to the referring physician, the patient had experienced multiple sustained Valsalva maneuvers during EGD. The fundus examination of the left eye showed a large preretinal hemorrhage surrounded by multiple small retinal hemorrhages in the posterior pole. One month later, fundus examination revealed a floating organized vitreous hemorrhage. The pars plana vitrectomy was performed to treat persistent vitreous hemorrhage. One month after vitrectomy, fundus examination showed normal retina and the patient’s vision recovered to 20/20. Valsalva maneuver can occur during EGD under sedation, and Valsalva retinopathy should be considered as a possible cause. Valsalva retinopathy should be included in the differential diagnosis when a patient complains of blurred vision following EGD.
Core tip: This is the first report describing Valsalva retinopathy following esophagogastroduodenoscopy (EGD) under sedation. This case highlights Valsalva retinopathy induced by Valsalva maneuvers during EGD under incomplete propofol sedation, and that this ocular complication should be included in the differential diagnosis when a patient complains of sudden blurred vision following EGD.
- Citation: Park JH, Sagong M, Chang W. Valsalva retinopathy following esophagogastroduodenoscopy under propofol sedation: A case report. World J Gastroenterol 2014; 20(11): 3056-3058
- URL: https://www.wjgnet.com/1007-9327/full/v20/i11/3056.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i11.3056
Valsalva retinopathy was first described in 1972 as a superficial macular hemorrhage that is caused by a forcible exhalation against a closed glottis, resulting in a sudden rise in intrathoracic or intra-abdominal pressure[1]. The true incidence of such cases remains unknown because hemorrhages sparing the macula may be asymptomatic and only severe cases are reported[2]. Valsalva retinopathy is usually identified in healthy adults and has been associated with aerobic exercise[3], vigorous sexual activity[4], inflating balloons[5], prostate biopsy[6], dental surgery[7], episodes of constipation, vomiting and lifting in pregnant women[8,9], paroxysmal coughing[1], oratorical contest[10], colonoscopy[11], and esophagogastroduodenoscopy (EGD) without sedation[12]. The visual prognosis is favorable and the hemorrhage usually resolves spontaneously within several weeks to months. However, some cases with a large and dense hemorrhage may result in permanent vision loss because of the toxic effects of iron and pigmentary change of the macula.
Recently, there is a growing trend to perform EGD under sedation (20%-78%)[13-16]. To our knowledge, this is the first report describing Valsalva retinopathy following EGD under sedation.
A 43-year-old woman who had no previous history of systemic or ocular disease presented with a chief complaint of sudden visual loss in her left eye. EGD under propofol sedation was performed one day prior to the sudden visual loss. According to the referring physician, the patient had experienced multiple sustained Valsalva maneuvers during the procedure.
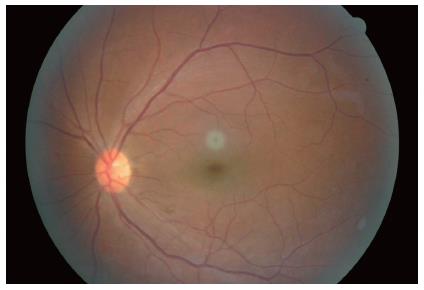
On examination, the patient was found to have the best corrected visual acuity (BCVA) 20/20 in the right eye and hand motion vision in the left eye. The anterior segments and intraocular pressure were normal. The fundus examination of the left eye showed a large preretinal hemorrhage surrounded by multiple small retinal hemorrhages in the posterior pole (Figure 1). The fundus examination of the right eye was unremarkable. We suspected Valsalva retinopathy on the basis of the patient’s history and results from slit lamp examination and fundus examination. Overall, systemic examination was unremarkable, and laboratory findings were normal.
We decided to observe the evolution of the hemorrhage over a period of one month. After one month, fundus examination showed a floating organized vitreous hemorrhage, and the patient’s corrected visual acuity was 20/400. A 20-gauge three-port pars plana vitrectomy was performed to treat the dense organized vitreous hemorrhage. There was no abnormal vascular pathology. One month after vitrectomy, fundus examination showed normal retina without any sequelae, and the patient’s vision had recovered to 20/20 (Figure 2).
Valsalva retinopathy is characterized by the presence of preretinal hemorrhage following a Valsalva maneuver. Valsalva maneuver, including coughing, could be induced by a forcible exhalation against a closed glottis, thereby creating a sudden increase in intrathoracic and intra-abdominal pressures. The increased pressure results in the spontaneous rupture of perifoveal capillaries. Valsalva retinopathy can cause a sudden loss of vision when it involves the macula. Therapeutic options for Valsalva retinopathy include conservative management, vitrectomy, and laser membranotomy[17]. Most cases resolve spontaneously with favorable visual outcomes.
Routine endoscopy can be performed successfully with either moderate or deep sedation. Moderate sedation provides adequate anxiolysis, analgesia, and amnesia for most patients and is safer than deep sedation. Moderate sedation is usually recommended for most patients, although many patients may move into lighter or deeper sedation levels[18]. Generally, for upper endoscopy, adequate sedation preventing any gagging or coughing during esophageal intubation can be achieved[19]. Propofol sedation is expected to eliminate the gagging reflex and fear during EGD[20]. The mean dose of administered propofol in EGD is 161 mg[19], but low-dose propofol sedation is commonly used due to its narrow therapeutic range (1.5-5 μg/mL). In the present case, 50 mg of propofol (1 mg/kg) was administered. In a case of low-dose propofol sedation, awakening can occur during EGD, which could retrigger the cough reflex[21]. Also, in EGD, the endoscopic field should be optimized by the use of gas insufflation in EGD. Gas insufflation can cause gastric distention, leading to an increase in intra-abdominal pressure, which can transmit the pressure directly to the eye. Therefore, coughing and gastric distention may not be inhibited completely with propofol sedation, and the rise in intra-abdominal pressure can cause spontaneous rupture of perifoveal capillary bed.
Valsalva retinopathy associated with vitreous hemorrhage is uncommon, and this is the first reported case of Valsalva retinopathy following EGD under propofol sedation. Only one other reported case of Valsalva retinopathy occurring during EGD exists in the publicly available literature, but it occurred without sedation[12].
In summary, the Valsalva maneuver could be caused in patients under propofol sedation during EGD because of incomplete control of the depth of sedation. Valsalva retinopathy should be considered on the differential diagnosis when observing a patient complaining of blurred vision following EGD under sedation.
A 43-year-old woman presented with a complaint of decreased vision after esophagogastroduodenoscopy (EGD) under propofol sedation.
Valsalva retinopathy was highly suspicious by clinical history.
The differential diagnosis included diabetic retinopathy, leukemic retinopathy, and retinal arterial macroaneurysm.
Laboratory findings were within normal limits.
Fundus examination showed a large preretinal hemorrhage surrounded by multiple small retinal hemorrhages in the posterior pole.
One month later, pars plana vitrectomy was performed to treat persistent vitreous hemorrhage.
Valsalva retinopathy has been reported following aerobic exercise, vigorous sexual activity, vomiting, forceful coughing, and weightlifting.
Valsalva retinopathy is a unilateral or bilateral condition that occurs when increased intrathoracic or intra-abdominal pressure transmitted to the eye causes a sharp rise in the intraocular venous pressure and rupture of superficial retinal capillaries.
Valsalva retinopathy should be included in the differential diagnosis when a patient complains of blurred vision following EGD.
Valsalva retinopathy is not a common ophthalmologic complication associated with Valsalva maneuver. This case report indicate that an unexpected sudden intra-abdominal rise in pressure can occur during EGD under propofol induced sedation, and thus could cause extensive retinal hemorrhage.
P- Reviewers: Chatziralli IP, Sivandzadeh GR S- Editor: Wen LL L- Editor: A E- Editor: Wang CH
| 1. | Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972;70:298-313. [PubMed] |
| 2. | Geddes JF, Talbert DG. Paroxysmal coughing, subdural and retinal bleeding: a computer modelling approach. Neuropathol Appl Neurobiol. 2006;32:625-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Sueke H. Valsalva retinopathy induced by vigorous nightclub dancing. Med J Aust. 2009;190:333. [PubMed] |
| 4. | Markovits AS. Sudden visual loss associated with sexual activity. Arch Ophthalmol. 1996;114:106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Georgiou T, Pearce IA, Taylor RH. Valsalva retinopathy associated with blowing balloons. Eye (Lond). 1999;13:686-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Fanin LA, Thrasher JB, Mader TH, Truxal AR. Valsalva retinopathy associated with transrectal prostate biopsy. Br J Urol. 1994;74:391-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Krepler K, Wedrich A, Schranz R. Intraocular hemorrhage associated with dental implant surgery. Am J Ophthalmol. 1996;122:745-746. [PubMed] |
| 8. | Callender D, Beirouty ZA, Saba SN. Valsalva haemorrhagic retinopathy in a pregnant woman. Eye (Lond). 1995;9:808-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Deane JS, Ziakas N. Valsalva retinopathy in pregnancy. Eye (Lond). 1997;11:137-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Kim JY, Lee DH, Lee JH, Yoon IeN. Valsalva retinopathy associated with an oratorical contest. Korean J Ophthalmol. 2009;23:318-320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Oboh AM, Weilke F, Sheindlin J. Valsalva retinopathy as a complication of colonoscopy. J Clin Gastroenterol. 2004;38:793-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Choi SW, Lee SJ, Rah SH. Valsalva retinopathy associated with fiberoptic gastroenteroscopy. Can J Ophthalmol. 2006;41:491-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Cohen LB, Wecsler JS, Gaetano JN, Benson AA, Miller KM, Durkalski V, Aisenberg J. Endoscopic sedation in the United States: results from a nationwide survey. Am J Gastroenterol. 2006;101:967-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 341] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 14. | Paspatis GA, Manolaraki MM, Tribonias G, Theodoropoulou A, Vardas E, Konstantinidis K, Chlouverakis G, Karamanolis DG. Endoscopic sedation in Greece: results from a nationwide survey for the Hellenic Foundation of gastroenterology and nutrition. Dig Liver Dis. 2009;41:807-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Riphaus A, Rabofski M, Wehrmann T. Endoscopic sedation and monitoring practice in Germany: results from the first nationwide survey. Z Gastroenterol. 2010;48:392-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | Baudet JS, Borque P, Borja E, Alarcón-Fernández O, Sánchez-del-Río A, Campo R, Avilés J. Use of sedation in gastrointestinal endoscopy: a nationwide survey in Spain. Eur J Gastroenterol Hepatol. 2009;21:882-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Gibran SK, Kenawy N, Wong D, Hiscott P. Changes in the retinal inner limiting membrane associated with Valsalva retinopathy. Br J Ophthalmol. 2007;91:701-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Bailey PL, Zuccaro G. Sedation for endoscopic procedures: not as simple as it seems. Am J Gastroenterol. 2006;101:2008-2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Külling D, Orlandi M, Inauen W. Propofol sedation during endoscopic procedures: how much staff and monitoring are necessary? Gastrointest Endosc. 2007;66:443-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Yoshida H, Ayuse T, Ishizaka S, Ishitobi S, Nogami T, Oi K. Management of exaggerated gag reflex using intravenous sedation in prosthodontic treatment. Tohoku J Exp Med. 2007;212:373-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Guglielminotti J, Rackelboom T, Tesniere A, Panhard X, Mentre F, Bonay M, Mantz J, Desmonts JM. Assessment of the cough reflex after propofol anaesthesia for colonoscopy. Br J Anaesth. 2005;95:406-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |