Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Nov 14, 2013; 19(42): 7292-7301
Published online Nov 14, 2013. doi: 10.3748/wjg.v19.i42.7292
Published online Nov 14, 2013. doi: 10.3748/wjg.v19.i42.7292
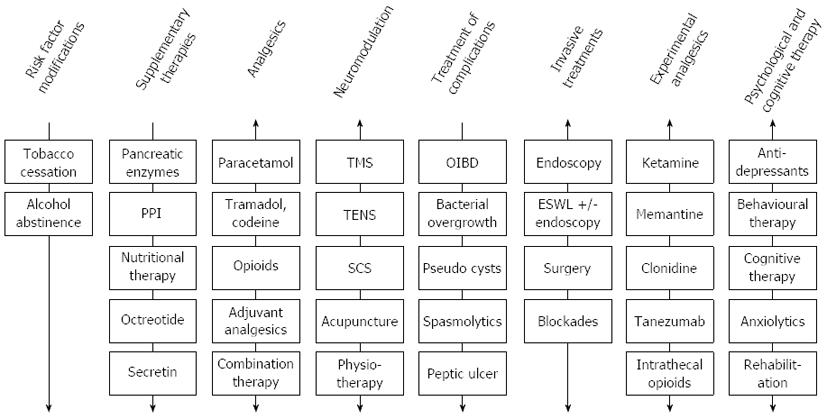
Figure 1 An illustration of the multidisciplinary approach recommended for managing pain in chronic pancreatitis.
The mechanisms underlying pain in chronic pancreatitis (CP) are highly variable in the individual patient and there is no single approach that is effective for all patients. Hence, choosing the right algorithm for the pain treatment is highly depending of the pathogenesis of pain in the individual situation. Some treatments follow a typical step-up approach as indicated by the unidirectional arrows. Other treatments follow either a step-up or a top-down approach depending on the specific situation as illustrated by the bidirectional arrows. The latter is seen for example for analgesic therapies, where weak analgesics may be appropriate to control pain in one situation. On the other hand a more aggressive approach, using opioids combined with adjuvant analgesics as first line therapy (i.e., top-down), is useful in patients with a more aggressive and debilitating pain pattern to control pain and prevent sensitization of central pain pathways. Often combination therapies of e.g., opioids or adjuvant analgesics are used. Surgery, endoscopic therapies etc. are included in the figure for completeness, although these therapies are beyond the scope of this review. PPI: Proton pump inhibitor; TENS: Transcutaneous electrical nerve stimulation; SCS: Spinal cord stimulation; OIBD: Opioid-induced bowel dysfunction; TMS: Transcranial magnetic stimulation; ESWL: Extracorporeal shock wave lithotripsy.
- Citation: Olesen SS, Juel J, Graversen C, Kolesnikov Y, Wilder-Smith OH, Drewes AM. Pharmacological pain management in chronic pancreatitis. World J Gastroenterol 2013; 19(42): 7292-7301
- URL: https://www.wjgnet.com/1007-9327/full/v19/i42/7292.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i42.7292