Published online Jun 14, 2013. doi: 10.3748/wjg.v19.i22.3447
Revised: April 2, 2013
Accepted: April 18, 2013
Published online: June 14, 2013
AIM: To determine the technical feasibility and safety of an endoscopic gastrojejunostomy with a pure natural orifice transluminal endoscopic surgery (NOTES) technique using a T-anchoring device in a porcine survival model.
METHODS: An endoscopic gastrojejunostomy with a pure NOTES technique using a T-anchoring device was performed on 10 healthy female minipigs weighing approximately 40 kg each under general anesthesia. All procedures were performed with a transgastric approach using a 2-channel therapeutic endoscope.
RESULTS: The transgastric gastrojejunostomy was technically successful in all cases. A total of four to six stitched pairs of a T-anchoring device were used to secure the anastomosis. The median time required to enter the peritoneal cavity and pull the small bowel into the stomach was 34 min (range: 19-41 min); the median time required to suture the anastomosis was 67 min (range: 44-78 min). An obstruction of the efferent limb occurred in one case, and a rupture of the anastomosis site occurred in another case. As a result, the functional success rate was 80% (8/10). Small bowel adhesion to the stomach and liver occurred in one case, but the anastomosis was intact without leakage or obstruction.
CONCLUSION: A transgastric gastrojejunostomy with a T-anchoring device may be safe and technically feasible. A T-anchoring device may provide a simple and effective endoscopic suturing method.
Core tip: Natural orifice transluminal endoscopic surgery (NOTES) have become part of the growing trend of minimally invasive surgery and have been gradually used in more diverse areas. An endoscopic gastrojejunostomy using a pure NOTES technique may be attractive because it can be a simple and less invasive method for bypassing a gastric outlet or duodenal obstruction. An endoscopic transgastric gastrojejunostomy with T-anchoring devices may be a technically feasible, useful alternative to invasive surgery. However, a great deal of care and further improvement is needed because of the risk of procedure-related complications.
- Citation: Song TJ, Seo DW, Kim SH, Park DH, Lee SS, Lee SK, Kim MH. Endoscopic gastrojejunostomy with a natural orifice transluminal endoscopic surgery technique. World J Gastroenterol 2013; 19(22): 3447-3452
- URL: https://www.wjgnet.com/1007-9327/full/v19/i22/3447.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i22.3447
Gastric outlet obstruction or duodenal obstruction is one of the most serious problems that frequently occur in patients with advanced malignancies of the stomach or periampullary region[1-3]. In cases in which an oral diet was impossible due to gastric outlet obstruction or duodenal obstruction, open surgery using hand-sewn techniques, staplers, or compression devices, as well as laparoscopic surgery using staplers, have been the major treatment modalities thus far[4-8]. However, these obstructions usually occur in patients with unresectable malignancies of an advanced stage, and invasive surgery may be impossible or quite burdensome for these end-stage patients[9]. Therefore, less invasive methods to address malignant obstructions may be attractive to these patients[10,11].
Various procedures using natural orifice transluminal endoscopic surgery (NOTES) techniques are part of the growing trend of minimally invasive surgery, and these NOTES techniques have been gradually used in more diverse areas[12-16]. Because NOTES techniques have proven to have many advantages in terms of being less invasive compared with existing surgical methods, they are considered to be effective treatment measures that are not burdensome for terminal-stage patients, particularly those with advanced-stage malignancies[17,18]. The first NOTES anastomosis, a cholecystogastrostomy, was reported in 2005, and subsequent studies have demonstrated that various forms of intraperitoneal surgery performed using laparoscopy could be conducted using a flexible endoscope[19,20]. Performing a gastrojejunostomy using a NOTES technique is attractive because it can be a simple and less invasive method for bypassing a gastric outlet obstruction or duodenal obstruction.
The aim of these experiments was to assess the technical feasibility and safety of an endoscopic peroral transgastric gastrojejunostomy procedure with a prototype T-anchoring device in a porcine model.
For this experiment, 10 minipigs, which were breeds of pig developed for medical research, weighing approximately 40 kg each were used. The anesthesia was performed by one veterinarian, and the gastrojejunostomy was performed by two endoscopists and two nurses. Permission for this study was obtained from the Animal Experiment Review Board of Asan Medical Center.
Pretreatment: The animals were fed a soft liquid diet beginning 48 h before the procedure; then, they abstained from food-except for only a small quantity of water-beginning 24 h before the procedure. They were anesthetized with a combination of anesthetic agents, including tiletamine hydrochloride, zolazepam hypochloride (Zoletil®, Virbac do Brasil Ltda., Brazil), and xylazine (Rompun®, Bayer Korea Co. Ltd., South Korea) before the procedures, and general anesthesia was maintained with 1.5% isoflurane (Forane®, Choongwae Pharma Co. Ltd., South Korea). Premedication was performed 30 min before anesthesia using an intramuscular injection of atropine sulfate (Bayer Korea Co. Ltd., South Korea).
Procedure: A multibending two-channel endoscope (2TQ260®, Olympus Optical Co. Ltd., Japan) was used for the procedures. The minipigs were placed in a supine position, and the endoscope was inserted into the stomach. The anterior wall of the body of the stomach was punctured with a needle knife (Micro knife®, Boston Scientific, Natick, MA, United States). After the puncture, a 0.035-inch guidewire (Jagwire®, Boston Scientific, Natick, MA, United States) was inserted into the peritoneal cavity through the needle knife, and the needle knife was then removed. A papillotome was inserted along the guidewire, and a 2-cm-long incision was made on the stomach wall. The incision was made in four directions-up, down, left, and right-while changing the direction of the papillotome. A dilating balloon with a diameter of 20 mm (CRE®, Boston Scientific, Natick, MA, United States) was inserted along the guidewire, and the puncture site was dilated twice for one minute each. After dilation, the dilating balloon was pushed inside the peritoneal cavity, together with the endoscope, while being deflated. After entry into the peritoneal cavity, the guidewire and inflating balloon were removed from the scope.
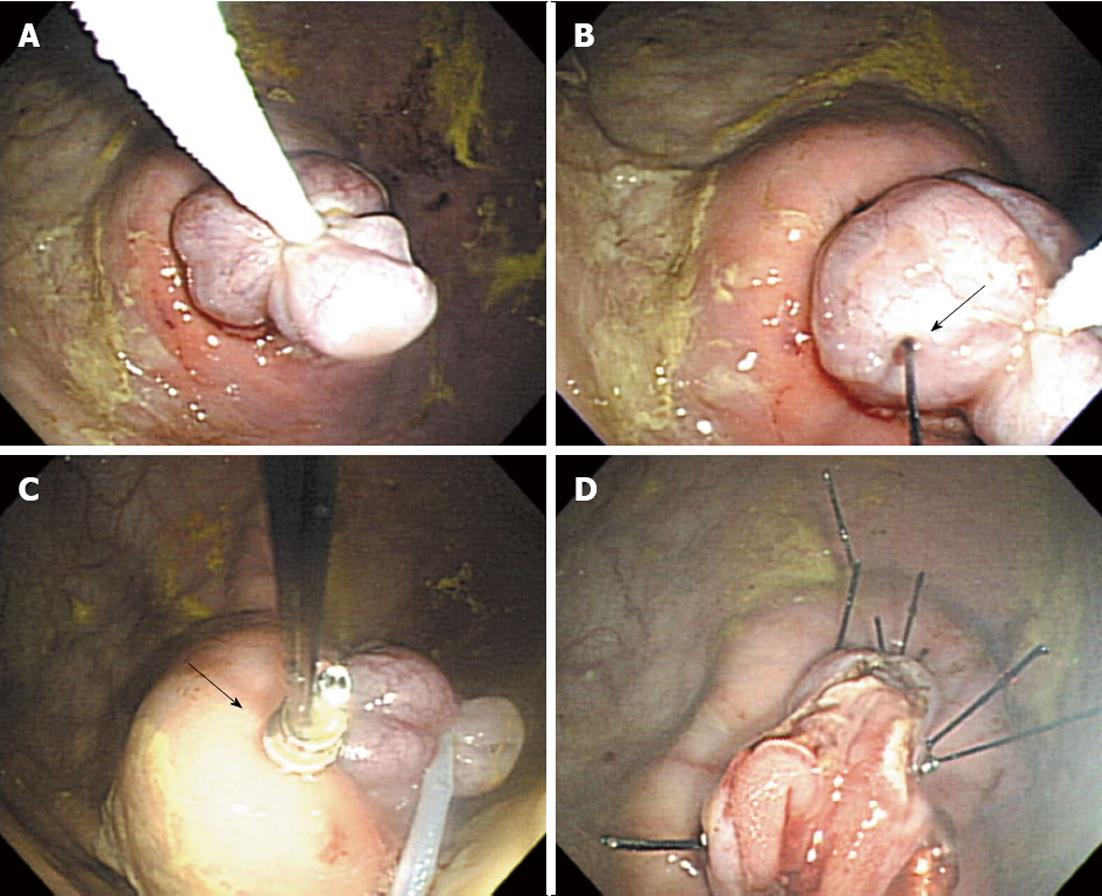
An appropriate loop of the small intestine was selected for the anastomosis. Usually, the mid-jejunum was selected using indications provided by the anatomic position relative to other structures. When the location of the anastomosis in the jejunum had been determined, grasping forceps were inserted into a channel of the endoscope, and a snare was inserted into another channel. After the snare was opened, the grasping forceps were pushed through the inside of the open snare, and the snare was slowly closed. Then, the predetermined antimesenteric site on the mid-jejunum was grasped using the grasping forceps, and the jejunum was drawn into the inside of the snare. Thereafter, the snare was closed to grasp the jejunum, which was brought into the stomach. The jejunum was grasped with care to avoid blocking the mesenteric vessel, and the air in the abdominal cavity was sufficiently aspirated before the jejunum was placed into the stomach. Because the small intestine would go back into the peritoneal cavity after being drawn into the stomach, the snare was held closed to hold the small intestine and prevent it from returning to the abdominal cavity while the grasping forcep was being removed. In the endoscopic channel (from which the grasping forceps had been removed), a needle, installed with the first T-anchoring tag, was inserted. Using the needle, the small intestine was punctured, and the first T-anchoring tag was detached through the inside of the needle. Then, the needle was removed, and the second T-anchoring tag was installed into the needle. This needle was inserted through the same channel, and the stomach wall (i.e., the wall closest to the T-anchoring tag that was inserted first) was punctured. The second T-anchoring tag was detached through the inside of the needle, and the needle was removed. Then, a pair of T-anchoring tags was locked using a locking device. Thereafter, a pair of scissor forceps was inserted to cut the suture thread connected to the T-anchoring tag, thereby completing the suture. These processes were repeated four to six times to fix the jejunum to the stomach. Finally, the snare was opened, and an incision was made on the jejunum using a needle knife to open the jejunal lumen to the inside of the stomach (Figure 1).
Postoperative care: Third-generation cephalosporin and analgesics were administered intravenously after the procedures, and a liquid diet was administered after 24 h. All animals survived for seven days before they were euthanized. Then, autopsies were conducted. The health conditions and abnormal reactions of the animals were monitored for seven days. After seven days, the animals were euthanized, and the anastomosis site, afferent and efferent loops, and peritoneal cavity were observed.
The detailed results of the endoscopic peroral transgastric gastrojejunostomy performed on the 10 animals are shown in Table 1. The transgastric gastrojejunostomy was technically successful in all cases (100%, 10/10). A total of four to six stitched pairs of T-anchoring devices were used to secure the anastomosis. The median time from when the endoscope was inserted through the mouth to puncture the stomach, enter the peritoneal cavity, find an appropriate region of the small intestine, and draw it into the stomach was 34 min (range: 19-41 min). The median time required to complete the anastomosis using the T-anchoring devices was 67 min (range: 44-78 min). During the operations, there were no adverse events, such as bleeding or internal organ injury, and the vital signs of the animals were stable. On the postmortem examination, although the afferent limb was patent, the efferent limb was obstructed in one case. A rupture of the anastomosis site occurred in another case. As a result, the functional success rate was 80% (8/10). Mild adhesion of the short segment of the small intestine to the stomach and liver occurred in one case, but the anastomosis was intact without leakage or obstruction. In all other cases, the small intestine loops of the anastomosis reached the stomach without tension or abnormal rotation.
| Technical success | 10 (100) |
| Functional success | 8 (80) |
| Number of stitched pairs of the T-anchoring device | |
| 4 | 4 |
| 5 | 4 |
| 6 | 2 |
| Median time required to enter the peritoneal cavity and pull the small bowel into the stomach (min, range) | 34 (19-41) |
| Median time required to suture the anastomosis (min, range) | 67 (44-78) |
| Adverse events | |
| Rupture of anastomosis site | 1 |
| Insufficient efferent limb opening | 1 |
| Small bowel adhesion | 1 |
In this study, the peroral transgastric gastrojejunostomy performed with a pure NOTES technique using a flexible endoscope and a T-anchoring device was technically feasible. Peroral transgastric gastrojejunostomy might be another potential therapeutic option for gastric outlet obstruction or duodenal obstruction in addition to surgical anastomosis. The method of using a pure NOTES technique to bypass a malignant obstruction is advantageous over surgical anastomosis because it does not require any abdominal incision; as a result, it induces less surgical stress[21]. Moreover, it can be easily performed using a flexible endoscope and accessories under a conscious sedation state without general anesthesia, which is required for the usual endoscopic procedures[22]. Therefore, this method is considered to be potentially applicable not only to the palliation of malignant obstructions but also to benign diseases in which conventional transabdominal and laparoscopic surgeries are unsuitable, such as bariatric surgery for morbidly obese patients[19].
In this study, the anastomosis was performed using a T-anchoring device. Until recently, conventional hemoclips have been used for the closure of puncture sites during NOTES procedures[23]. Although existing hemoclips can be used easily in various types of conventional endoscopic procedures, they are disadvantageous as full-thickness sutures are impossible to secure, and the sutures may fail if two ends of an opening are distant from each other[24,25]. However, T-anchoring devices are advantageous because their use enables full-thickness sutures to be secured. Moreover, even in cases in which two ends of an opening are distant from each other, T-anchoring devices secure full-thickness sutures if only a needle puncture is possible. Therefore, T-anchoring devices can be used in diverse NOTES procedures, such as the closure of various incision sites or anastomosis, and also in the management of adverse events that may occur in conventional endoscopic procedures (e.g., the closure of a bowel perforation and bleeding control).
In this study, room air, which is usually used in conventional endoscopic procedures, was used for the inflation of the stomach and the peritoneal cavity. During our pure NOTES procedures, air in the stomach may have leaked into the peritoneal cavity during the anastomosis to induce abdominal distension. Although air in the peritoneal cavity was sufficiently aspirated during the process of drawing the small intestine into the stomach, the air that leaked into the peritoneal cavity during the anastomosis was not removed by the suction of the stomach. Abdominal distension occurred immediately after the anastomosis in two cases, and thus, percutaneous needle aspiration was performed after the procedures. When this procedure is performed on humans, CO2 gas, which is easily absorbed and discharged through breathing, will be helpful in reducing this distension[26,27]. A great deal of care must be exercised to prevent pressure inside the stomach from rising too high during the procedure, and an endoscope installed with a pressure gauge at its fore-end should be developed to enable the easy measurement and constant maintenance of the pressure in the pneumoperitoneum[28,29].
In our study, complications occurred with respect to the sizes of the initial incisions on the stomach wall. The case in which there was an obstruction in the efferent loop was the first, and we believe that the obstruction in the efferent loop occurred because the stomach wall incision was not sufficiently large. Although the incision site was further enlarged using a 20-mm dilatation balloon, openings enlarged by balloon dilatation may contract again, unlike direct incisions. Therefore, the initial incisions on the stomach wall are important. In one case in which a rupture occurred in the anastomosis site, the incision was large, exceeding 2.5 cm. Our speculation is that the suture site could not tolerate the pressure in the stomach after the diet because the incision was too large. Therefore, the size of the opening should be appropriate, and a great deal of care must be taken to ensure that it is not too small or too large. In our opinion, in the case of an endoscopic gastrojejunostomy, 2.0 cm is thought to be an appropriate incision size. In the event that a large incision exceeding 2.5 cm has been made, a greater number of sutures and a longer period of fasting after the procedure are necessary. In addition, the T-anchoring tag should be improved to ensure that the suture site can tolerate sufficiently high pressure.
The present T-anchoring device is a prototype. To secure one pair of sutures using this device, a needle should be inserted through an endoscopic channel at least twice, and then, a pair of scissor forceps should be inserted to cut the thread after installing two T-anchoring tags. Given these lengthy processes, coupled with the fact that more than four pairs of sutures are necessary for the anastomosis, the overall procedure time may become too long. In addition, the threads connected to the T-anchoring tags may occasionally become tangled, causing problems during the processes of inserting and removing the needle. Therefore, improving the T-anchoring device is necessary to simplify the suturing process. Many (but not all) of the limitations of the instruments that have been used for the NOTES technique can be overcome by innovative design and engineering improvements[20].
In conclusion, a peroral transgastric gastrojejunostomy with T-anchoring devices may be a technically feasible, useful alternative to invasive surgery. However, a great deal of care is needed because of the risk of complications. The T-anchoring device is still in its early stage and needs further improvements; however, it may provide a simple and effective endoscopic suturing method.
Various natural orifice transluminal endoscopic surgery (NOTES) techniques have become part of the growing trend of minimally invasive surgery, and these NOTES techniques have been gradually used in more diverse areas.
Performing a gastrojejunostomy using a pure NOTES technique is attractive because it can be a simple and less invasive method for bypassing a gastric outlet obstruction or duodenal obstruction.
The transgastric gastrojejunostomy was technically successful in all cases (100%, 10/10). A total of four to six stitched pairs of T-anchoring devices were used to secure the anastomosis. An obstruction of the efferent limb occurred in one case, and a rupture of the anastomosis site occurred in another case. As a result, the functional success rate was 80% (8/10). Small bowel adhesion to the stomach and liver occurred in one case, but the anastomosis was intact without leakage or obstruction in this animal.
T-anchoring devices secure full-thickness sutures if only a needle puncture is possible. Therefore, T-anchoring devices can be used in diverse NOTES procedures, such as the closure of various incision sites or anastomosis, and also in the management of adverse events that may occur in conventional endoscopic procedures.
NOTES is a minimally invasive surgery technique that has been recently devised; the application of this technique has been gradually expanding.
The authors reported an animal study on the transgastric gastrojejunostomy using NOTES technique. This study provides a further potential advances in NOTES, with important potential advantages for use in human in due course.
P- Reviewers Day AS, Marinho RT, Wig JD S- Editor Huang XZ L- Editor A E- Editor Xiong L
| 1. | Alam TA, Baines M, Parker MC. The management of gastric outlet obstruction secondary to inoperable cancer. Surg Endosc. 2003;17:320-323. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Mittal A, Windsor J, Woodfield J, Casey P, Lane M. Matched study of three methods for palliation of malignant pyloroduodenal obstruction. Br J Surg. 2004;91:205-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 151] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | Ly J, O’Grady G, Mittal A, Plank L, Windsor JA. A systematic review of methods to palliate malignant gastric outlet obstruction. Surg Endosc. 2010;24:290-297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 112] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 4. | Dietz UA, Debus ES. Intestinal anastomoses prior to 1882; a legacy of ingenuity, persistence, and research form a foundation for modern gastrointestinal surgery. World J Surg. 2005;29:396-401. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | McGuire J, Wright IC, Leverment JN. Surgical staplers: a review. J R Coll Surg Edinb. 1997;42:1-9. [PubMed] [Cited in This Article: ] |
| 6. | Bergström M, Ikeda K, Swain P, Park PO. Transgastric anastomosis by using flexible endoscopy in a porcine model (with video). Gastrointest Endosc. 2006;63:307-312. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 154] [Cited by in F6Publishing: 161] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 7. | Reed DN, Cacchione RN, Allen JW, Arlauskas V, Casey J, Larson GM, Vitale G. Laparoscopic choledochojejunostomy and gastrojejunostomy in a porcine model. Surg Endosc. 2003;17:86-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Hamad MA, Mentges B, Buess G. Laparoscopic sutured anastomosis of the bowel. Surg Endosc. 2003;17:1840-1844. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Smith AC, Dowsett JF, Russell RC, Hatfield AR, Cotton PB. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet. 1994;344:1655-1660. [PubMed] [Cited in This Article: ] |
| 10. | Jeurnink SM, Steyerberg EW, Hof Gv, van Eijck CH, Kuipers EJ, Siersema PD. Gastrojejunostomy versus stent placement in patients with malignant gastric outlet obstruction: a comparison in 95 patients. J Surg Oncol. 2007;96:389-396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 127] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 11. | Jeurnink SM, van Eijck CH, Steyerberg EW, Kuipers EJ, Siersema PD. Stent versus gastrojejunostomy for the palliation of gastric outlet obstruction: a systematic review. BMC Gastroenterol. 2007;7:18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 250] [Cited by in F6Publishing: 279] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 12. | Solomon D, Lentz R, Duffy AJ, Bell RL, Roberts KE. Female sexual function after pure transvaginal appendectomy: a cohort study. J Gastrointest Surg. 2012;16:183-16; discussion 183-16;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Lehmann KS, Ritz JP, Wibmer A, Gellert K, Zornig C, Burghardt J, Büsing M, Runkel N, Kohlhaw K, Albrecht R. The German registry for natural orifice translumenal endoscopic surgery: report of the first 551 patients. Ann Surg. 2010;252:263-270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 179] [Cited by in F6Publishing: 191] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 14. | Marks JM, Ponsky JL, Pearl JP, McGee MF. PEG “Rescue”: a practical NOTES technique. Surg Endosc. 2007;21:816-819. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Fischer LJ, Jacobsen G, Wong B, Thompson K, Bosia J, Talamini M, Horgan S. NOTES laparoscopic-assisted transvaginal sleeve gastrectomy in humans--description of preliminary experience in the United States. Surg Obes Relat Dis. 2009;5:633-636. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Nau P, Anderson J, Yuh B, Muscarella P, Christopher Ellison E, Happel L, Narula VK, Melvin WS, Hazey JW. Diagnostic transgastric endoscopic peritoneoscopy: extension of the initial human trial for staging of pancreatic head masses. Surg Endosc. 2010;24:1440-1446. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Niu J, Song W, Yan M, Fan W, Niu W, Liu E, Peng C, Lin P, Li P, Khan AQ. Transvaginal laparoscopically assisted endoscopic cholecystectomy: preliminary clinical results for a series of 43 cases in China. Surg Endosc. 2011;25:1281-1286. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Bingener J, Gostout CJ. Update on natural orifice translumenal endoscopic surgery. Gastroenterol Hepatol (NY). 2012;8:384-389. [PubMed] [Cited in This Article: ] |
| 19. | Swain P. NOTES and anastomosis. Gastrointest Endosc Clin N Am. 2008;18:261-77; viii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Park PO, Bergström M, Ikeda K, Fritscher-Ravens A, Swain P. Experimental studies of transgastric gallbladder surgery: cholecystectomy and cholecystogastric anastomosis (videos). Gastrointest Endosc. 2005;61:601-606. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 343] [Cited by in F6Publishing: 362] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 21. | Freeman LJ, Rahmani EY, Al-Haddad M, Sherman S, Chiorean MV, Selzer DJ, Snyder PW, Constable PD. Comparison of pain and postoperative stress in dogs undergoing natural orifice transluminal endoscopic surgery, laparoscopic, and open oophorectomy. Gastrointest Endosc. 2010;72:373-380. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Garud SS, Willingham FF. Natural orifice transluminal endoscopic surgery. Gastrointest Endosc. 2012;76:491-495. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114-117. [PubMed] [Cited in This Article: ] |
| 24. | Lee SS, Oelschlager BK, Wright AS, Soares RV, Sinan H, Montenovo MI, Hwang JH. Assessment of a simple, novel endoluminal method for gastrotomy closure in NOTES. Surg Endosc. 2011;25:3448-3452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Song TJ, Seo DW, Kim SH, Park do H, Lee SS, Lee SK, Kim MH. The Performance of Multiple Transgastric Procedures Using the Natural Orifice Transluminal Endoscopic Surgery Technique: Is Pure NOTES Satisfactory? Gut Liver. 2012;6:457-463. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | von Delius S, Sager J, Feussner H, Wilhelm D, Thies P, Huber W, Schuster T, Schneider A, Schmid RM, Meining A. Carbon dioxide versus room air for natural orifice transluminal endoscopic surgery (NOTES) and comparison with standard laparoscopic pneumoperitoneum. Gastrointest Endosc. 2010;72:161-19, 161-19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Ikechebelu JI, Obi RA, Udigwe GO, Joe-Ikechebelu NN. Comparison of carbon dioxide and room air pneumoperitoneum for day-case diagnostic laparoscopy. J Obstet Gynaecol. 2005;25:172-173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Meireles O, Kantsevoy SV, Kalloo AN, Jagannath SB, Giday SA, Magno P, Shih SP, Hanly EJ, Ko CW, Beitler DM. Comparison of intraabdominal pressures using the gastroscope and laparoscope for transgastric surgery. Surg Endosc. 2007;21:998-1001. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 29. | McGee MF, Rosen MJ, Marks J, Chak A, Onders R, Faulx A, Ignagni A, Schomisch S, Ponsky J. A reliable method for monitoring intraabdominal pressure during natural orifice translumenal endoscopic surgery. Surg Endosc. 2007;21:672-676. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |