Published online Jan 7, 2013. doi: 10.3748/wjg.v19.i1.92
Revised: October 20, 2012
Accepted: November 14, 2012
Published online: January 7, 2013
Processing time: 164 Days and 21.7 Hours
AIM: To investigate the clinical usefulness of a newly developed index, the “index of convexity (IOC)”, for evaluating liver functional reserve using technetium-99m-diethylenetriaminepentaacetic acid-galactosyl-human serum albumin (Tc-GSA scintigraphy).
METHODS: In total, 349 patients underwent Tc-GSA scintigraphy. Dynamic planner images were obtained, and time activity curves of the liver and heart were generated and analyzed. Our focus was on the convex shape of the liver accumulation curve. We developed a method for evaluating the extent of convexity and calculated an index that we named the IOC. Clearance index and receptor index were also calculated. The correlations between each GSA index with other liver function tests and liver histopathology were evaluated.
RESULTS: Among the 3 indices generated by Tc-GSA, the IOC had the highest correlation with all other liver function tests (indocyanine green R15, albumin, prothrombin time, cholinesterase level, platelet count, and total bilirubin level). IOC can also differentiate between normal liver, chronic hepatitis, and liver cirrhosis with highest F ratio among GSA indices as determined by one-way analysis of variance. Receiver operating characteristic analysis demonstrated high diagnostic performance of IOC in the diagnosis of cirrhosis.
CONCLUSION: IOC is a very simple and reliable index for assessing liver functional reserve, which may prove to be useful in combination with the indocyanine green test for preoperative assessment of hepatic resection.
- Citation: Miki K, Matsui Y, Teruya M, Kaminishi M, Kokudo N. Index of convexity: A novel liver function index using Tc-GSA scintigraphy. World J Gastroenterol 2013; 19(1): 92-96
- URL: https://www.wjgnet.com/1007-9327/full/v19/i1/92.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i1.92
Preoperative assessment of liver functional reserve is crucial for hepatobiliary surgeons. Technetium-99m-diethylenetriaminepentaacetic acid-galactosyl-human serum albumin (Tc-GSA) is a radiopharmaceutical developed for evaluating liver function[1,2] and has been widely used for preoperative assessments[3,4]. This asialoglycoprotein (ASGP) analogue is specifically taken up by hepatocytes[5], and its rate of accumulation in the liver can be evaluated using a gamma camera[6]. The liver accumulation process can be assessed by generating a time activity curve (TAC) from dynamic planer images. Several indices of liver function have been reported through the analysis of dynamic planer images[7-11]. Clearance index (HH15) and receptor index (LHL15) have been widely used for almost 20 years[7,8], as they are easy to calculate. On the other hand, Rmax or Rtotal are calculated using kinetic model analysis[9,10], which is highly complex and therefore not widely used. Index LU15 requires measurement of the radioactivity of the injection syringe[11], and the KL index requires curve-fitting software[4]. The use of both of these methods is limited. Although HH15 and LHL15 have been widely used for a long time, both indices have several problems[12,13]. HH15 uses only the radioactivity counts of the heart pool, which is very low compared to liver counts. This index can thus be influenced by counts in the liver through scatter effects or body movements. Index LHL15 is directly influenced by the manner in which the heart regions of interest (ROI) is drawn, generating inter-operator or inter-institutional differences[13,14].
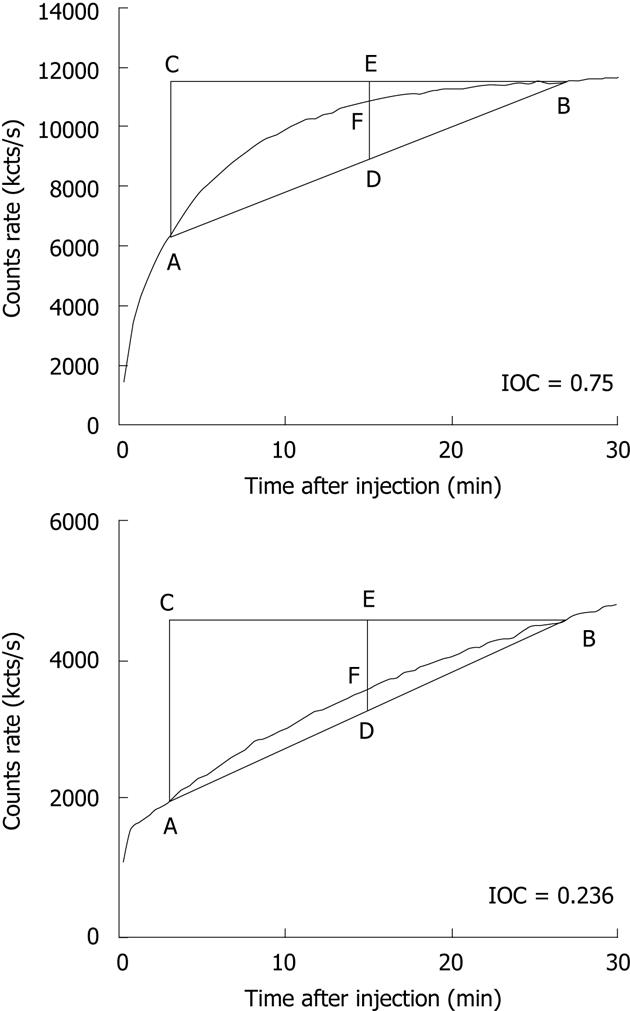
To overcome these problems, we focus on the shape of the liver TAC. Liver TACs have a convex shape in patients with good liver function. In contrast, liver TACs increase in a linear manner in patients with poor liver function. We developed a method for evaluating the convexity of the liver TAC and calculated an index that we have named the index of convexity (IOC).
In this study, we evaluated the significance and usefulness of this index for the assessment of the liver functional reserve.
This study included 349 patients who received Tc-GSA scintigraphy at the University of Tokyo Hospital or Showa General Hospital between 1998 and 2011. Of these patients, 239 had hepatocellular carcinomas, 34 had metastatic liver tumors, and 39 had cholangiocarcinomas. Others were diagnosed with miscellaneous diseases. Liver histology in 236 patients confirmed a diagnosis of chronic hepatitis (48 patients), normal liver (45 patients), and liver cirrhosis (143 patients).
All patients received 3 mg of Tc-GSA (185 MBq) intravenously. After the injection, dynamic images were obtained with the patient in a supine position using a large-field view gamma camera. Digital images were acquired at 30 s intervals for 30 min. TACs were generated by drawing ROI over the whole liver [L(t)] and heart [H(t)] on the digital images.
The HH15 and LHL15 were defined as follows: HH15 = H(15)/H(3); LHL15 = L(15)/(L(15) + L(3).
The convexity of the liver TAC was evaluated by an index defined as follows: ΔABC was drawn over the liver TAC, where A and B were placed on the TAC at the data points corresponding to 3 min and 27 min after injection, respectively. Therefore, the coordinates of A, B, and C were A[3, L(3)], B[27, L(27)], and C[3, L(27)], respectively. D and E were set as the mid points of lines AB and BC, respectively. F was defined as the intersection of line DE and arc AB (Figure 1).
IOC was defined as the ratio of the length of DF to the length of DE, where it is calculated as follows: IOC = [L(15) × 2 - L(3) - L(27)]/[L(27) - L(3)].
Possible values for this index range from 0 to 1.0. The better the liver function, the higher is the index value (Figure 1).
The indocyanine green (ICG) test was carried out, and 2 parameters (ICG R15 and ICG K value) were calculated using the standard methods. Serum albumin level (mg/dL), choline esterase level (IU/L), total bilirubin concentration (mg/dL), platelet counts (× 103/mm3), and prothrombin time (%) were also measured.
Correlations between the 3 parameters of the Tc-GSA study (HH15, LHL15 and IOC) and other liver function tests were estimated as Spearman’s rank correlations. The differences in each Tc-GSA parameter between the 3 groups (normal liver, chronic hepatitis, and liver cirrhosis) were evaluated by one-way analysis of variance (ANOVA). The diagnostic performance for the diagnosis of cirrhosis was evaluated by receiver operating characteristic (ROC) analysis.
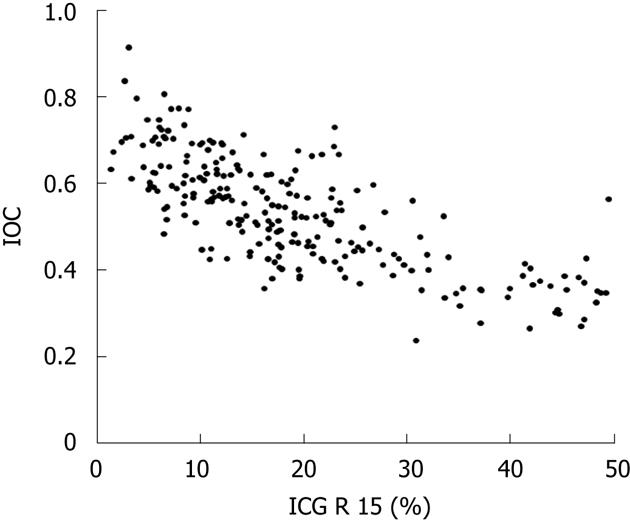
Spearman’s rank correlation coefficients are listed in Table 1. IOC showed higher correlations than the other conventional indices of HH15 and LHL15. In particular, the IOC has a strong correlation to ICG R15 values compared to HH15 or LHL15 (Figure 2). The correlation coefficient between IOC and ICG R15 was statistically higher than that between HH15 and ICG R15 and that between LHL15 and ICG R15.
| IOC | HH15 | LHL15 | ICG R15 | |
| ICG R15 | -0.761 | -0.666 | -0.627 | 1 |
| Albumin | 0.611 | 0.56 | -0.582 | -0.538 |
| PT | 0.556 | 0.555 | -0.521 | -0.549 |
| Platelets | 0.607 | 0.571 | -0.572 | -0.465 |
| ChE | 0.548 | 0.481 | -0.496 | -0.481 |
| T. Bil | -0.552 | -0.508 | 0.51 | 0.53 |
The results of one-way ANOVA also showed that IOC was significantly different between background liver groups with the highest F ratio (Table 2).
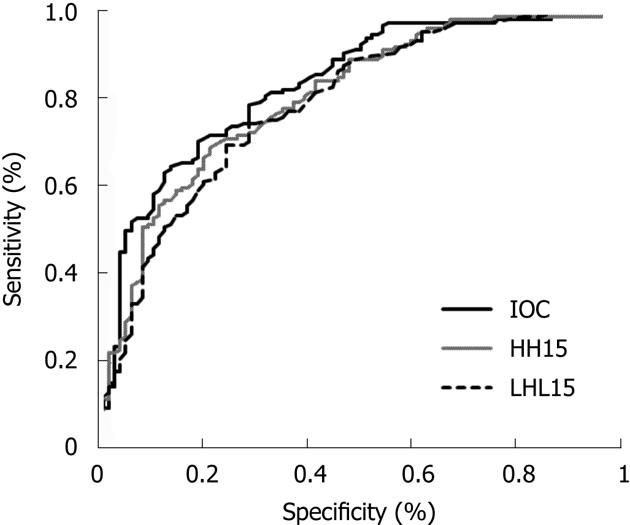
We performed ROC analysis to evaluate the diagnostic performance of IOC in diagnosing cirrhosis (Figure 3). The area under the curve (AUC) of ROC curves for IOC, HH15 and LHL15 were 0.851, 0.801 and 0.821, respectively. However, these differences were not statistically significant.
In this study, we developed a novel index to evaluate liver function using the dynamic images of Tc-GSA scintigraphy. This index is very simple to calculate and has stronger correlations to other liver function tests than do conventional indices such as HH15 or LHL15. This index also has a high diagnostic performance rating for diagnosing liver cirrhosis. IOC would thus be very useful to hepatobiliary surgeons in assessing preoperative liver function.
Tc-GSA is an ASGP analogue labeled with a radioisotope and developed for the assessment of liver functional reserve. Tc-GSA scintigraphy for assessing liver function has several benefits to consider. First, accumulation of Tc-GSA in the liver can be monitored continuously through dynamic planer images. The kinetics of ASGP have been investigated in detail in animals and humans[10,15,16], and several kinetic parameters have been proposed as candidates for indices of liver function[6,9,10]. Second, regional accumulation of Tc-GSA in the liver was measured separately to evaluate regional liver function via single photon emission computed tomography images[17-19], which can be used for the assessment of regional liver function after portal vein embolization[20,21]. Although many parameters of Tc-GSA scintigraphy have been reported, only HH15 and LHL15 are used widely.
Despite their widespread use, we found that both of these indices showed only moderate correlations to other liver functions, and we encountered some cases with a discrepancy between the values of both indices and their liver histology or liver functions[12], Since the TAC of the heart is influenced by background radiation or radioactivity in the liver adjacent to the heart, indicated Tc-GSA concentrations may deviate from the actual blood concentrations[22]. HH15, using only TAC of the heart and ignoring liver accumulation, is not suitable for the ideal index. LHL15 has been shown to be directly influenced by the manner in which the ROI is drawn over the heart[13,14]. The LHL15 index value was also found to be influenced by the shape of the liver and the size of the heart. These observations suggest that HH15 and LHL15 indices are prone to several measurement errors.
To overcome these problems, we focused on the shape of the liver accumulation curve. The shape of the liver accumulation curve seems universally consistent, even if the patients are stout or their liver is deformed.
The convexity of the liver curve seems to be a specific feature of good liver function. The liver curve increased rapidly and afterwards reaches a plateau in the case of good liver function. In contrast, the liver curve increases linearly throughout the examination period, with no plateau, in patients with poor liver function. In order to evaluate the convexity of the liver curve, we calculated the ratio of the length of line DF to line DE as described in Figure 1. IOC decreases as liver function deteriorates. This index correlated very strongly to other liver function tests, including ICG. IOC can be calculated quite easily as calculations require liver radioactivity data at only 3 time points. Results of one-way ANOVA indicate that IOC has a higher correlation to liver histology than does HH15 or LHL15. In fact, IOC seemed to be superior to HH15 or LHL15 in the diagnosis of liver cirrhosis as indicated by ROC analysis, although the differences between the AUC of ROC curves for IOC, HH15, and LHL15 were not statistically significant.
Makuuchi et al proposed that the criteria determining the extent of liver resection include ascites volume, bilirubin levels, and ICG tests[23]. Since then, the ICG test has been widely used in Japan for the preoperative assessment of liver functional reserve. It is well known that hyperbilirubinemia and large port-systemic shunts interfere with the results of ICG tests[24,25]. In addition, some patients are intolerant of ICG[26]. We have encountered many cases with large discrepancies between ICG results and conventional liver function tests. In these cases, Tc-GSA scintigraphy plays a complementary role in deciding on surgical procedures. In this study, IOC showed a stronger correlation with conventional liver function tests than did the ICG test. IOC is a simple and reliable index that is superior to HH15 and LHL15 indices and is a valuable parameter exceeding ICG tests in the preoperative assessment of liver functional reserve. We analyzed the Tc-GSA data retrospectively in this study. In order to prove the usefulness of this index, further prospective studies should be undertaken.
Technetium-99m-diethylenetriaminepentaacetic acid-galactosyl-human serum albumin (Tc-GSA) was a radiopharmaceutical developed in Japan to assess liver functional reserve. The liver uptake of Tc-GSA can be evaluated from dynamic images obtained using a gamma camera. Among the indices for the Tc-GSA scintigraphic analysis of liver functional reserve, only the receptor index (LHL15) and clearance indices (HH15) have been widely used. However, both indices are prone to measurement errors. To date, no appropriate methods have been developed that are superior to LHL15 and HH15 in terms of reliability and accuracy in the preoperative assessment of liver functional reserve.
Several methods of evaluating liver function using Tc-GSA scintigraphy have been reported. In particular, methods using kinetic model analysis are highly complex, and another method requires radioactivity measurements of the injection syringe. Therefore, to overcome the limitations of these methods and increase the use of Tc-GSA scintigraphy for the assessment of hepatobiliary surgical outcomes, it is necessary to develop a simple but reliable index that is superior to LHL15 and HH15.
The authors focused on the shape of the liver time activity curve of Tc-GSA and found that the extent of the convexity correlated with liver function, Developing a new index, the index of convexity (IOC), that is very easy to calculate. The authors demonstrated that this index predicts liver functional reserve better than the conventional LHL15 and HH15 indices.
The IOC is a very simple but reliable index for assessing liver functional reserve, which is, in turn, very useful for preoperative assessment of hepatic resection. Therefore, it can be introduced in any institute without the need for special software.
Tc-GSA is a radiopharmaceutical developed for evaluating liver function. This asialoglycoprotein analogue is specifically absorbed by hepatocytes, and its rate of accumulation in the liver is influenced by the liver functional reserve, which can be evaluated using a gamma camera.
This is a very interesting and well-performed study evaluating the usefulness of a novel index of liver functional reserve based on dynamic Tc-GSA scintigraphic images. The authors developed a new method for analyzing the results of Tc-GSA scintigraphy based on the shape of the liver TAC and introduced the “IOC”. They found that IOC had a strong correlation with conventional liver function test results and a good performance in the diagnosis of cirrhosis. The interesting conclusions of the study were that IOC is a simple but reliable index for assessing liver functional reserve and that it would be useful in deciding on surgical procedures. The study is well designed and written, with clinically relevant conclusions and appropriate data supporting the results.
P- Reviewers Zocco MA, Cheng KS, Tandon RK S- Editor Jiang L L- Editor A E- Editor Xiong L
| 1. | Torizuka K, Ha-Kawa SK, Ikekubo K, Suga Y, Tanaka Y, Hino M, Ito H, Yamamoto K, Yonekura Y. [Phase I clinical study on 99mTc-GSA, a new agent for functional imaging of the liver]. Kaku Igaku. 1991;28:1321-1331. [PubMed] |
| 2. | Torizuka K, Ha-Kawa SK, Kudo M, Kitagawa S, Kubota Y, Tanaka Y, Hino M, Ikekubo K. [Phase II clinical study on 99mTc-GSA, a new agent for functional imaging of the liver]. Kaku Igaku. 1992;29:85-95. [PubMed] |
| 3. | Kwon AH, Ha-Kawa SK, Uetsuji S, Kamiyama Y, Tanaka Y. Use of technetium 99m diethylenetriamine-pentaacetic acid-galactosyl-human serum albumin liver scintigraphy in the evaluation of preoperative and postoperative hepatic functional reserve for hepatectomy. Surgery. 1995;117:429-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 80] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Mitsumori A, Nagaya I, Kimoto S, Akaki S, Togami I, Takeda Y, Joja I, Hiraki Y. Preoperative evaluation of hepatic functional reserve following hepatectomy by technetium-99m galactosyl human serum albumin liver scintigraphy and computed tomography. Eur J Nucl Med. 1998;25:1377-1382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 68] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Morell AG, Gregoriadis G, Scheinberg IH, Hickman J, Ashwell G. The role of sialic acid in determining the survival of glycoproteins in the circulation. J Biol Chem. 1971;246:1461-1467. [PubMed] |
| 6. | Stadalnik RC, Vera DR, Woodle ES, Trudeau WL, Porter BA, Ward RE, Krohn KA, O’Grady LF. Technetium-99m NGA functional hepatic imaging: preliminary clinical experience. J Nucl Med. 1985;26:1233-1242. [PubMed] |
| 7. | Kudo M, Todo A, Ikekubo K, Hino M, Yonekura Y, Yamamoto K, Torizuka K. Functional hepatic imaging with receptor-binding radiopharmaceutical: clinical potential as a measure of functioning hepatocyte mass. Gastroenterol Jpn. 1991;26:734-741. [PubMed] |
| 8. | Kudo M, Todo A, Ikekubo K, Hino M. Receptor index via hepatic asialoglycoprotein receptor imaging: correlation with chronic hepatocellular damage. Am J Gastroenterol. 1992;87:865-870. [PubMed] |
| 9. | Ha-Kawa SK, Tanaka Y. A quantitative model of technetium-99m-DTPA-galactosyl-HSA for the assessment of hepatic blood flow and hepatic binding receptor. J Nucl Med. 1991;32:2233-2240. [PubMed] |
| 10. | Miki K, Kubota K, Kokudo N, Inoue Y, Bandai Y, Makuuchi M. Asialoglycoprotein receptor and hepatic blood flow using technetium-99m-DTPA-galactosyl human serum albumin. J Nucl Med. 1997;38:1798-1807. [PubMed] |
| 11. | Koizumi K, Uchiyama G, Arai T, Ainoda T, Yoda Y. A new liver functional study using Tc-99m DTPA-galactosyl human serum albumin: evaluation of the validity of several functional parameters. Ann Nucl Med. 1992;6:83-87. [PubMed] |
| 12. | Kokudo N, Vera DR, Makuuchi M. Clinical application of TcGSA. Nucl Med Biol. 2003;30:845-849. [PubMed] |
| 13. | Nakajima K, Kinuya K, Mizutani Y, Hwang EH, Michigishi T, Tonami N, Kobayashi K. Simple scintigraphic parameters with Tc-99m galactosyl human serum albumin for clinical staging of chronic hepatocellular dysfunction. Ann Nucl Med. 1999;13:5-11. [PubMed] |
| 14. | Koizumi M, Yamada Y, Nomura E, Takiguchi T, Kokudo N. An easy and reproducible semi-automatic method for the evaluation of 99mTc-galactosyl human serum albumin. Ann Nucl Med. 1997;11:345-348. [PubMed] |
| 15. | Schwartz AL, Fridovich SE, Lodish HF. Kinetics of internalization and recycling of the asialoglycoprotein receptor in a hepatoma cell line. J Biol Chem. 1982;257:4230-4237. [PubMed] |
| 16. | Sawamura T, Nakada H, Hazama H, Shiozaki Y, Sameshima Y, Tashiro Y. Hyperasialoglycoproteinemia in patients with chronic liver diseases and/or liver cell carcinoma. Asialoglycoprotein receptor in cirrhosis and liver cell carcinoma. Gastroenterology. 1984;87:1217-1221. [PubMed] |
| 17. | Matsuzaki S, Onda M, Tajiri T, Kim DY. Hepatic lobar differences in progression of chronic liver disease: correlation of asialoglycoprotein scintigraphy and hepatic functional reserve. Hepatology. 1997;25:828-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Akaki S, Mitsumori A, Kanazawa S, Togami I, Takeda Y, Hiraki Y. Lobar decrease in 99mTc-GSA accumulation in hilar cholangiocarcinoma. J Nucl Med. 1999;40:394-398. [PubMed] |
| 19. | Hwang EH, Taki J, Shuke N, Nakajima K, Kinuya S, Konishi S, Michigishi T, Aburano T, Tonami N. Preoperative assessment of residual hepatic functional reserve using 99mTc-DTPA-galactosyl-human serum albumin dynamic SPECT. J Nucl Med. 1999;40:1644-1651. [PubMed] |
| 20. | Sugai Y, Komatani A, Hosoya T, Yamaguchi K. Response to percutaneous transhepatic portal embolization: new proposed parameters by 99mTc-GSA SPECT and their usefulness in prognostic estimation after hepatectomy. J Nucl Med. 2000;41:421-425. [PubMed] |
| 21. | Beppu T, Hayashi H, Okabe H, Masuda T, Mima K, Otao R, Chikamoto A, Doi K, Ishiko T, Takamori H. Liver functional volumetry for portal vein embolization using a newly developed 99mTc-galactosyl human serum albumin scintigraphy SPECT-computed tomography fusion system. J Gastroenterol. 2011;46:938-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 22. | Ha-Kawa SK, Kojima M, Suga Y, Kurokawa H, Itagaki Y, Tanaka Y. [Dose estimation of Tc-99m-DTPA-galactosyl-human serum albumin (Tc-99m-GSA) in the blood with nonlinear regression method]. Kaku Igaku. 1991;28:425-428. [PubMed] |
| 23. | Miyagawa S, Makuuchi M, Kawasaki S, Kakazu T. Criteria for safe hepatic resection. Am J Surg. 1995;169:589-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 252] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 24. | Stockmann M, Malinowski M, Lock JF, Seehofer D, Neuhaus P. Factors influencing the indocyanine green (ICG) test: additional impact of acute cholestasis. Hepatogastroenterology. 2009;56:734-738. [PubMed] |
| 25. | Miyamoto Y, Oho K, Kumamoto M, Toyonaga A, Sata M. Balloon-occluded retrograde transvenous obliteration improves liver function in patients with cirrhosis and portal hypertension. J Gastroenterol Hepatol. 2003;18:934-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 92] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 26. | Okuda K, Ohkubo H, Musha H, Kotoda K, Abe H, Tanikawa K. Marked delay in indocyanine green plasma clearance with a near-normal bromosulphophthalein retention test: a constitutional abnormality? Gut. 1976;17:588-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |