Published online Dec 28, 2012. doi: 10.3748/wjg.v18.i48.7394
Revised: September 27, 2012
Accepted: October 19, 2012
Published online: December 28, 2012
Successful cannulation of the common bile duct may be difficult in patients in whom the papilla is located entirely within a diverticulum. In this study, we report successful biliary cannulation in three patients following intubation of the distal tip of the duodenoscope into the duodenal diverticulum and locating the major papilla. No complications occurred during the operation or during the postoperative period. This method didn’t need second incubation an endoscope and might lower the burden of patients. So this skill is useful to deal with the papilla hidden inside the large diverticulum because of its safety and convenience.
- Citation: Wang BC, Shi WB, Zhang WJ, Gu J, Tao YJ, Wang YQ, Wang XF. Entering the duodenal diverticulum: A method for cannulation of the intradiverticular papilla. World J Gastroenterol 2012; 18(48): 7394-7396
- URL: https://www.wjgnet.com/1007-9327/full/v18/i48/7394.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i48.7394
Periampullary diverticula (PAD) are found in 9% to 32.8% of patients who undergo endoscopic retrograde cholangiopancreatography (ERCP)[1]. The papilla often exists at the superior or inferior border of the PAD. Occasionally, identification of the papillary orifice and successful cannulation of the common bile duct (CBD) may be more difficult in patients in whom the papilla is located entirely within the diverticulum, even for endoscopic experts. In this report, we present three cases where the papilla was hidden in a large duodenal diverticulum. Successful biliary cannulation was achieved following intubation of the distal tip of the duodenoscope into the duodenal diverticulum.
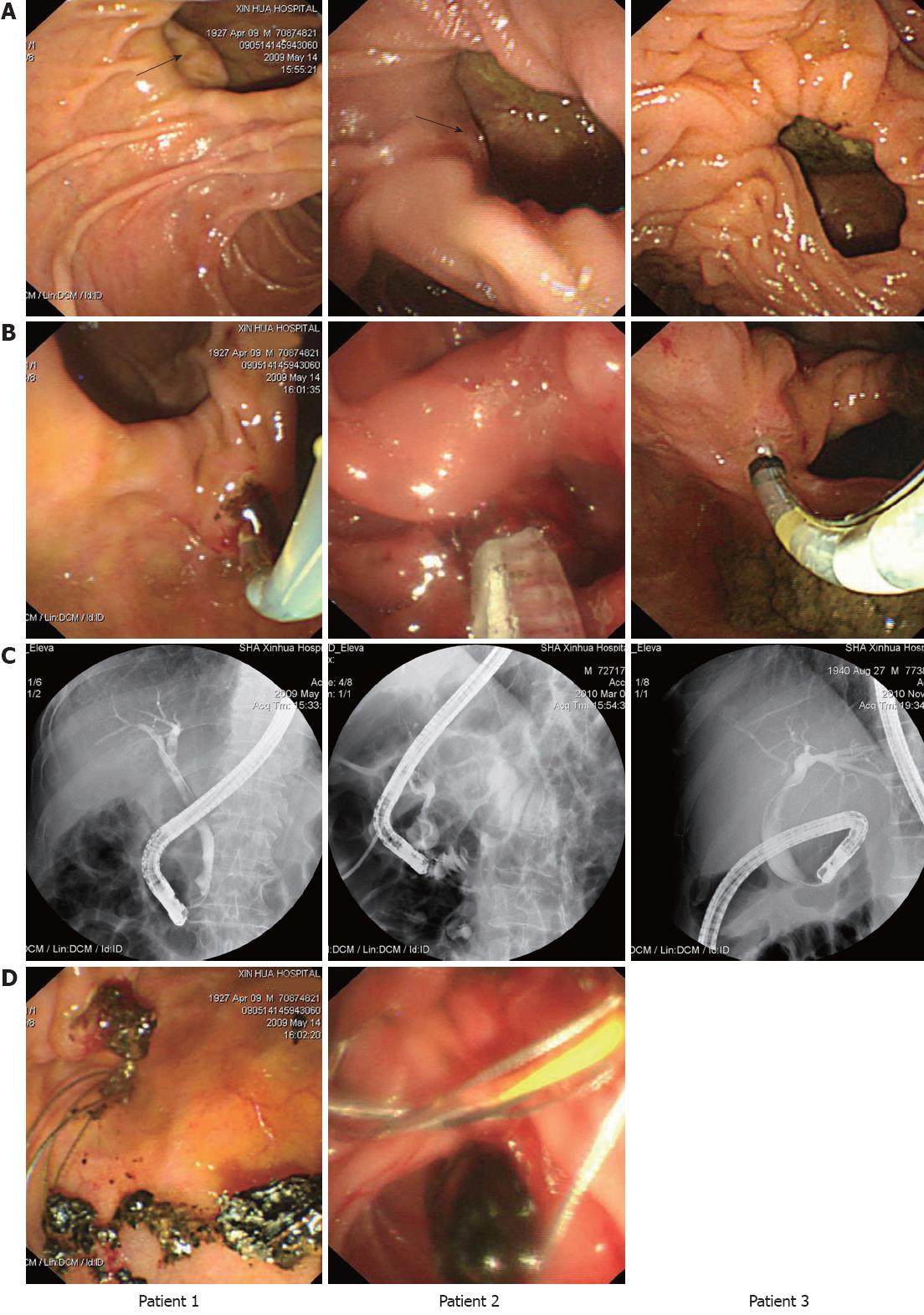
Three male patients (aged 70, 78 and 82 years) were admitted to our hospital as a result of right upper quadrant pain and fever and jaundice. Magnetic resonance cholangiopancreatography revealed intra- and extra-hepatic bile duct dilation (CBD stones were presented in patient one and patient two). On ERCP, the papilla could not be found at the rim of large duodenal diverticula (one with septa). We therefore suspected that the papilla was hidden inside the diverticula. With careful searching, the papillary orifices were indistinctly seen at the left side of the inner diverticular borders in patient one and patient two, but were not visualized in patient three (Figure 1). Several attempts were made to evert the papilla out of the diverticulum, including dilating the diverticular rim, using two devices in one channel (a catheter and a sphincterotome), but without success. As the diverticulum was judged to be large enough to accommodate the distal tip of a duodenoscope, we decided to intubate the duodenoscope (JF-260V, Olympus Medical System, Tokyo, Japan) into the duodenal diverticulum by gently adjusting the knob, and by push-pull the duodenoscope. Eventually, we discovered that the orifices in all three patients were on the left side of the inner diverticular borders, opening towards the medial and posterior wall of the diverticulum. Subsequently, the orifices were faced by finely adjusting the direction of the endoscope, and by carefully exploring the papillary alignment (Figure 1). Biliary cannulation and stone extraction was then conducted using a small biliary sphincterotomy and balloon dilatation (Figure 1). No complications occurred during the procedure or during the postoperative period. All patients were well on discharge shortly after surgery.
PAD is outpunching from the duodenum that represents herniation of the mucosal or submucosal layers through a defect in the muscular wall within a radius of 2 to 3 cm of the ampulla of Vater. The prevalence of PAD increases with age and has been reported in 65% of elderly patients[2]. There is now clear evidence of an association between duodenal diverticula and bile duct stones, particularly in the absence of gallbladder stones[3]. The location of the papilla with respect to the diverticulum is divided into two categories. In typeIthe papilla is at the rim or within 2 cm of the edge of the diverticulum, and this is called a peri-diverticular papilla (PDP). In type II cases, the papilla lies inside or at the middle of the bottom edge of the diverticulum or between two adjacent diverticula, and this is termed an intradiverticular papilla (IDP)[4]. According to a report by Tham et al[3], typeIand type II cases accounted for 74.7% and 25.3%, respectively, in a cohort of 83 patients with diverticular papilla. Previously, successful cannulation in patients with PAD has varied from 61% to 95.4%, which is significantly lower that that observed in those without PAD[1,5]. Two recent studies reported that PAD did not cause any technical difficulties at ERCP or increase the risk of complications, however, this was true only when patients with the undetectable papilla were excluded[3,6]. It is reasonable to speculate an even lower successful cannulation rate in IDP patients in whom papilla are often more difficult to locate than in PDP patients. Therefore great efforts are needed to find new methods to achieve successful cannulation in patients with IDP.
In recent years, new devices and new manipulations for successful biliary cannulation in patients with IDP have been reported. These include using a two-devices-in-one-channel method[7], balloon dilation of a narrow-necked diverticulum[8], using an ultrathin gastroscope to locate the papilla[9], an endoscopic ultrasound-guided rendezvous technique[10], endoclip-assisted biliary cannulation[11], and the double-endoscope method[12].
Our study suggests an alternative skill for biliary cannulation in patients with IDP, which didn’t need second incubation an endoscope. In contrast to colon diverticula, the PAD is relatively fixed as they are located behind the retroperitoneum. Also the adjacent kidney and pancreas could provide further support to diverticula wall. Thus, we can relatively easily control the position of the duodenoscope in the duodenal diverticulum. To avoid sudden movements in the PAD, the duodenoscope can also be pulled back to the duodenal lumen for stone extraction. There were no complications, such as bleeding or perforation, during ERCP treatment of these three patients. So this skill is a safe and convenient method which may lower the burden of patients.
We conclude that intubating the distal tip of the duodenoscope into the large duodenal diveriticulum, thereby locating the hidden papilla, is a safe and convenient skill that facilitates both biliary cannulation and endoscopic treatment in the hands of experienced practitioners, which didn’t need second incubation an endoscope and may lower the burden of patients.
Peer reviewer: Dr. Akio Katanuma, Center for Gastroenterology, Teine-Keijinkai Hospital, 1-40 Maeda 1-jo 12-chome, Teine-ku, Sapporo 006-8555, Japan
S- Editor Wen LL L- Editor A E- Editor Li JY
| 1. | Lobo DN, Balfour TW, Iftikhar SY. Periampullary diverticula: consequences of failed ERCP. Ann R Coll Surg Engl. 1998;80:326-331. [PubMed] [Cited in This Article: ] |
| 2. | Shemesh E, Klein E, Czerniak A, Coret A, Bat L. Endoscopic sphincterotomy in patients with gallbladder in situ: the influence of periampullary duodenal diverticula. Surgery. 1990;107:163-166. [PubMed] [Cited in This Article: ] |
| 3. | Tham TC, Kelly M. Association of periampullary duodenal diverticula with bile duct stones and with technical success of endoscopic retrograde cholangiopancreatography. Endoscopy. 2004;36:1050-1053. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Boix J, Lorenzo-Zúñiga V, Añaños F, Domènech E, Morillas RM, Gassull MA. Impact of periampullary duodenal diverticula at endoscopic retrograde cholangiopancreatography: a proposed classification of periampullary duodenal diverticula. Surg Laparosc Endosc Percutan Tech. 2006;16:208-211. [PubMed] [Cited in This Article: ] |
| 5. | Zoepf T, Zoepf DS, Arnold JC, Benz C, Riemann JF. The relationship between juxtapapillary duodenal diverticula and disorders of the biliopancreatic system: analysis of 350 patients. Gastrointest Endosc. 2001;54:56-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 101] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Panteris V, Vezakis A, Filippou G, Filippou D, Karamanolis D, Rizos S. Influence of juxtapapillary diverticula on the success or difficulty of cannulation and complication rate. Gastrointest Endosc. 2008;68:903-910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Kim HJ, Kim YS, Myung SJ, Seo DW, Lee SK, Kim MH, Min YI. A novel approach for cannulation to the ampulla within the diverticulum: double-catheter method. Endoscopy. 1998;30:S103-S104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 8. | Tóth E, Lindström E, Fork FT. An alternative approach to the inaccessible intradiverticular papilla. Endoscopy. 1999;31:554-556. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | García-Cano J. Use of an ultrathin gastroscope to locate a papilla hidden within a duodenal diverticulum. Endoscopy. 2010;42 Suppl 2:E96-E97. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Mangiavillano B, Arcidiacono PG, Carrara S, Masci E, Testoni PA. EUS-guided rendezvous technique for difficult cannulation of an intradiverticular papilla. Endoscopy. 2008;40 Suppl 2:E87-E88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Huang CH, Tsou YK, Lin CH, Tang JH. Endoscopic retrograde cholangiopancreatography (ERCP) for intradiverticular papilla: endoclip-assisted biliary cannulation. Endoscopy. 2010;42 Suppl 2:E223-E224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 12. | Külling D, Haskell E. Double endoscope method to access intradiverticular papilla. Gastrointest Endosc. 2005;62:811-812. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |