Published online Dec 7, 2012. doi: 10.3748/wjg.v18.i45.6527
Revised: November 4, 2012
Accepted: November 11, 2012
Published online: December 7, 2012
Delayed gastric emptying (DGE) is a frequent complication after pylorus-preserving pancreatoduodenectomy (PpPD). Kawai and colleagues proposed pylorus-resecting pancreatoduodenectomy (PrPD) with antecolic gastrojejunal anastomosis to obviate DGE occurring after PpPD. Here we debate the reported differences in the prevalence of DGE in antecolic and retrocolic gastro/duodeno-jejunostomies after PrPD and PpPD, respectively. We concluded that the route of the gastro/duodeno-jejunal anastomosis with respect to the transverse colon; i.e., antecolic route or retrocolic route, is not responsible for the differences in prevalence of DGE after pancreatoduodenectomy (PD) and that the impact of the reconstructive method on DGE is related mostly to the angulation or torsion of the gastro/duodeno-jejunostomy. We report a prevalence of 8.9% grade A DGE and 1.1% grade C DGE in a series of 89 subtotal stomach-preserving PDs with Roux-en Y retrocolic reconstruction with anastomosis of the isolated Roux limb to the stomach and single Roux limb to both the pancreatic stump and hepatic duct. Retrocolic anastomosis of the isolated first jejunal loop to the gastric remnant allows outflow of the gastric contents by gravity through a “straight route”.
- Citation: Peparini N, Chirletti P. Does antecolic reconstruction decrease delayed gastric emptying after pancreatoduodenectomy? World J Gastroenterol 2012; 18(45): 6527-6531
- URL: https://www.wjgnet.com/1007-9327/full/v18/i45/6527.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i45.6527
Delayed gastric emptying (DGE) is a major cause of early morbidity following pancreatoduodenectomy (PD). Although it has been recently reported that pylorus-preserving pancreatoduodenectomy (PpPD) and classical Wipple’s PD are equal operations regarding the postoperative development of DGE[1], the occurrence of this complication is usually considered to be associated with PpPD. DGE after PpPD was first described by Warshaw et al[2] in 1985. DGE implies a state of postoperative gastroparesis and gastric stasis for which prolonged gastric drainage is necessary with delay to return to solid food intake. However, the pathogenesis of DGE is still unclear. Postoperative decrease in plasma motilin stimulation after duodenal resection[3], devascularization and denervation of the pylorus with subsequent pylorospasm in PpPD[4,5] and other operative factors such as the route of gastro- or duodeno-enteric reconstruction (antecolic vs retrocolic)[6] and the type of reconstructive technique (Billroth I vs Billroth II reconstruction)[7] may contribute to the occurrence of DGE. Moreover, intra-abdominal postoperative complications such as pancreatic fistula, peripancreatic collections, intraabdominal abscess or postoperative pancreatitis may increase the prevalence of DGE[8-13]. The reported prevalence of DGE after pancreatic surgery is remarkably variable due to different adopted definitions of DGE[10,14,15]. In fact, a consensus definition of DGE based on the impact on the clinical course and on postoperative management was proposed by the International Study Group of Pancreatic Surgery only in 2007[16]. Kawai et al[17] reported a prospective randomized controlled trial (RCT) on the prevalence of DGE in pylorus-resecting pancreatoduodenectomy (PrPD) vs PpPD. The authors proposed PrPD, in which the stomach is nearly entirely preserved and divided just adjacent to the pyloric ring, to obviate DGE occurring after PpPD and avoid the impairment of nutritional status occurring after classical Wipple’s PD. They highlighted that the results of their RCT significantly favored PrPD over PpPD, considering the prevalence of DGE (4.5% vs 17.2%): in these procedures an antecolic gastro- or duodeno-jejunal reconstruction was adopted[18]. A recent RCT comparing the occurrence of DGE after subtotal stomach-preserving pancreatoduodenectomy in pancreaticogastrostomy with retrocolic gastro-jejunostomy reconstruction and in pancreaticogastrostomy with antecolic gastro-jejunostomy reconstruction concluded that antecolic reconstruction, and not retrocolic reconstruction, decreases DGE prevalence. However, in this study, Billroth I (retrocolic) reconstructions were compared with Billroth II (antecolic) reconstructions[19]. After subtotal stomach-preserving pancreatoduodenectomy with pancreaticogastrostomy, Oida et al[20,21] considered retrocolic gastrojejunal reconstruction preferable to antecolic reconstruction for preventing DGE because pancreaticogastric anastomosis is located behind the stomach and the retrocolic route in gastroenteric reconstruction enables the gastric contents to easily reach the jejunum. In the study by Eshuis et al[22], DGE was more frequent in retrocolic reconstructions, but in multivariable analysis no association between the route of reconstruction and DGE was found.
After PD, Billroth I reconstruction is considered to have a higher incidence of DGE than Billroth II reconstruction[7], but Billroth I is considered to be a more physiologic procedure than Billroth II because Billroth I preserves the proximal jejunum in the alimentary circuit and maintains the hormonal stimuli on the remnant pancreas[23]. In evaluation of the prevalence of DGE in antecolic and retrocolic reconstruction in gastro- and duodeno-jejunostomy after classical Wipple’s PD and PpPD, respectively, the two compared procedures should differ only in the manner in which the jejunum is brought up in respect to the transverse colon. Kawai participated in a previously reported prospective RCT in which the adopted reconstructive procedures after PpPD were different only regarding the route; i.e., antecolic or retrocolic, for Billroth II type duodeno-jejunal anastomosis. The prevalence of DGE was significantly lower in the antecolic duodeno-jejunostomy group than in the retrocolic duodeno-jejunostomy group[6]. However, another recent RCT showed no difference in the prevalence of DGE between antecolic and retrocolic gastro/duodeno-jejunostomy following classical Wipple’s PD/PpPD after standardization of both the antecolic and retrocolic types of Billroth II gastro/duodeno-jejunostomy with respect to the distance from the hepatico-jejunostomy and angulation of the jejunal loop. In this study, the occurrence of DGE was not affected by the type of performed PD; i.e., classical Wipple’s PD vs PpPD, or the type of adopted reconstruction of the gastro/duodeno-jejunostomy; i.e., antecolic vs retrocolic[24]. Ueno et al[25] indicated that the transient torsion or angulation in the reconstruction of the alimentary tract is the main cause of DGE after PpPD. Several methods were proposed to promote the alimentary transit from the stomach through the jejunal loop, such as alignment of the stomach contour to avoid angulation of the jejunal loop distally to the duodeno-jejunal anastomosis in a Billroth I type of reconstructive procedure[25], and straight antecolic duodeno-jejunostomy twisting the jejunum 30° counterclockwise to preserve the patency of the efferent jejunum and placing the stomach in the left subcolic fossa to straighten it in a Billroth II type of reconstruction[26]. In the RCT by Chijiiwa et al[27] no significant difference in the prevalence of DGE was found between retrocolic vertically performed duodenojejunostomy and antecolic duodenojejunostomy (Table 1).
| Ref. | Type of study | No. of patients | Studied groups | Significant difference in prevalence of DGE |
| Eshuis et al[22] | CCS | 77 | PD/PpPD + PJ-BIIAG/DJ | Not found |
| 77 | PD/PpPD + PJ-BIIRG/DJ | |||
| Oida et al[20] | CCS | 14 | MSSPPD + PG-BIIAGJ | PG-BIIRGJ < PG-BIIAGJ |
| 28 | MSSPPD + PG-BIIRGJ | |||
| Masui et al[26] | CCS | 12 | PpPD + PJ-BIIADJ | PJ-BIIAMDJ < PJ-BIIADJ |
| 106 | PpPD + PJ-BIIAMDJ | |||
| Kawai et al[17] | RCT | 66 | PrPD + PJ-BIIAGJ | PrPD < PpPD |
| 64 | PpPD + PJ-BIIADJ | |||
| Kurahara et al[19] | RCT | 22 | SSPPD + PG-BIRGJ | PG-BIIAGJ < PG-BIRGJ |
| 24 | SSPPD + PG-BIIAGJ | |||
| Gangavatiker et al[24] | RCT | 35 | PD/PpPD + PJ-BIIAG/DJ | Not found |
| 37 | PD/PpPD + PJ-BIIRG/DJ | |||
| Chijiiwa et al[27] | RCT | 17 | PpPD + PJ-BIIADJ | Not found |
| 18 | PpPD + PJ-BIIVRDJ | |||
| Tani et al[6] | RCT | 40 | PpPD + PJ-BIIADJ | PJ-BIIADJ < PJ-BIIRDJ |
| 40 | PpPD + PJ-BIIRDJ |
Regarding the resection method, Kawai et al[17,18] highlighted that PrPD preserves the capacity of the stomach and obviates to pylorospasm, denervation and devascularization of the pylorus ring, which can occur in PpPD, and demonstrated that PrPD decreases the incidence of DGE in respect to PpPD. Recently, these surgical procedures of subtotal stomach-preserving (or pylorus-resecting) pancreatoduodenectomies have been adopted in surgical treatments of malignant tumors of the periampullary region and of the head of the pancreas. Our group has been adopting subtotal stomach-preserving pancreatoduodenectomy since 1995 for several considerations. After pancreaticoduodenectomy, gastric preservation favors adequate weight gain due to higher caloric intake; moreover, and most of all, normal acid secretion acts as a physiologic stimulus promoting the intestinal secretion of secretin and CCK-PZ, as well as the subsequent stimulation of pancreatic exocrine secretion with better digestion of protein and fat (weight gain). Lastly, preservation of the stomach with resection of the pylorus favors better gastric emptying[28,29]. Regarding the impact of the reconstructive method on DGE, we think that the route of the gastro/duodeno-jejunal anastomosis with respect to the transverse colon (antecolic or retrocolic) or the type of reconstruction performed (Billroth I or Billroth II procedure) are not truly responsible for the differences in the prevalence of DGE after PD. We believe that, after a PD, the impact of reconstructive methods on DGE is related mostly to the angulation or torsion of the reconstruction of the gastro/duodeno-jejunostomy because all the reported modified procedures associated with lower DGE, in Billroth I as well Billroth II types of reconstruction, are related to the reconstructive anatomy of the alimentary circuit and are aimed to facilitate the outflow of the ingests from the gastric/duodenal remnant. An antecolic gastro/duodeno-jejunostomy can favor a straight construction and gastric emptying by gravity in a Billroth II reconstruction after PD or PpPD[24] as well as a retrocolic Billroth II gastrojejunostomy after a subtotal stomach-preserving pancreatoduodenectomy with pancreaticogastrostomy reconstruction can favor the transit of the gastric contents towards the jejunum in consequence of the retrogastric site of pancreaticogastric anastomosis[20,21]. A Billroth II reconstruction can avoid the jejunal angulation produced by a Billroth I procedure in which the anastomosis of the proximal jejunum to the gastric/duodenal stump is performed at first, followed by pancreatico-jejunostomy and hepatico-jejunostomy[25] (or by hepatico-jejunostomy in a case in which a pancreaticogastrostomy is carried out).
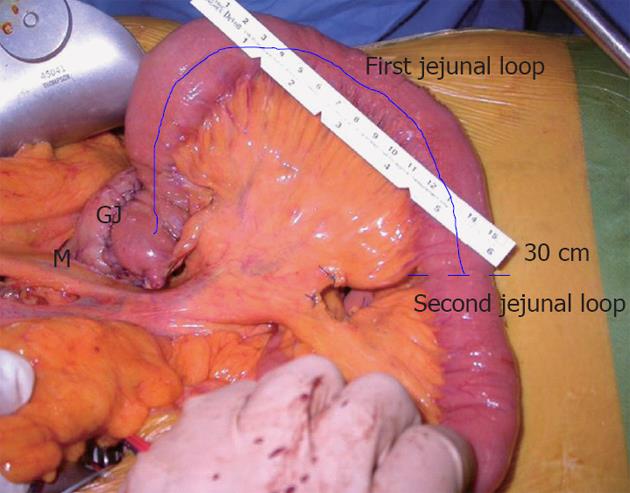
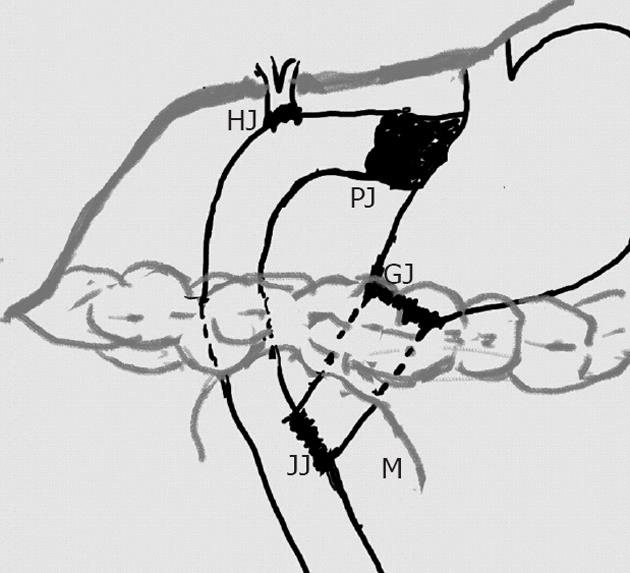
According to the ISGPS clinical criteria[16], we have recently reported a prevalence of 8.9% (8 cases) of grade A DGE and 1.1% (1 case) of grade C DGE in a series of 89 subtotal stomach-preserving PD followed by Roux-en-Y retrocolic reconstruction with anastomosis of the isolated Roux limb (i.e., first jejunal loop) to the stomach and single Roux limb (i.e., second jejunal loop) to the pancreatic stump and hepatic duct[30] (Figure 1).
We chose anastomosing the isolated proximal jejunum to the gastric remnant because, after removal of the duodenal source of CCK and secretin, preservation of the first jejunal loop in the reconstruction of the alimentary circuit maintains the physiologic jejunal secretion of secretin and CCK-PZ subsequent to alimentary transit and can compensate (at least in part) for the abolished duodenal hormonal release[29]. Then, the anastomosis of the isolated first jejunal loop to the gastric remnant, although retrocolic, avoided any angulation and torsion allowed the outflow of the gastric contents by gravity through a “straight route” (Figure 2). It is widely known that postoperative complications are related to the occurrence of DGE. Therefore, controlling the prevalence of other postoperative complications can contribute to reduce the occurrence of DGE. Postoperative pancreatic fistula occurred in seven patients (7.8%) of our series. Six cases of grade A fistula resolved spontaneously and in only one grade B fistula was percutaneous drainage necessary. Postoperative hemorrhage occurred in two of 89 (2.2%) patients, biliary fistula in eight (8.9%) patients and acute pancreatitis in one (1.1%). One patient with pre-existing stenosis of the hepatic artery developed thrombosis of the hepatic artery.
In conclusion, PrPD may contribute to a decrease in the prevalence of DGE due to pylorospasm, denervation and devascularization of the pylorus ring, which may occur after PpPD. A “straight” route, not necessarily an “antecolic” route, may obviate to the prevalence of DGE due to torsion or angulation in the reconstruction of the alimentary tract.
Peer reviewers: Mohamed Hassan, PhD, Laboratory for Moleculat Tumour Therapy, Department of Dermatology, University Hospital of Duesseldorf, Mooren Str. 5, 40225 Duesseldorf, Germany; Cunha JEM, Reprint Author, Rua Oquira 116, BR-05467030 Sao Paulo, Brazil; Izbicki JR, Reprint Author, Univ Hamburg, Dept Surg, Univ Hosp Eppendorf, Martinistr 52, D-20251 Hamburg, Germany
S- Editor Song XX L- Editor A E- Editor Li JY
| 1. | Paraskevas KI, Avgerinos C, Manes C, Lytras D, Dervenis C. Delayed gastric emptying is associated with pylorus-preserving but not classical Whipple pancreaticoduodenectomy: a review of the literature and critical reappraisal of the implicated pathomechanism. World J Gastroenterol. 2006;12:5951-5958. [PubMed] [Cited in This Article: ] |
| 2. | Warshaw AL, Torchiana DL. Delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy. Surg Gynecol Obstet. 1985;160:1-4. [PubMed] [Cited in This Article: ] |
| 3. | Suzuki H, Mochiki E, Haga N, Shimura T, Itoh Z, Kuwano H. Effect of duodenectomy on gastric motility and gastric hormones in dogs. Ann Surg. 2001;233:353-359. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Gauvin JM, Sarmiento JM, Sarr MG. Pylorus-preserving pancreaticoduodenectomy with complete preservation of the pyloroduodenal blood supply and innervation. Arch Surg. 2003;138:1261-1263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Kim DK, Hindenburg AA, Sharma SK, Suk CH, Gress FG, Staszewski H, Grendell JH, Reed WP. Is pylorospasm a cause of delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy? Ann Surg Oncol. 2005;12:222-227. [PubMed] [Cited in This Article: ] |
| 6. | Tani M, Terasawa H, Kawai M, Ina S, Hirono S, Uchiyama K, Yamaue H. Improvement of delayed gastric emptying in pylorus-preserving pancreaticoduodenectomy: results of a prospective, randomized, controlled trial. Ann Surg. 2006;243:316-320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 231] [Cited by in F6Publishing: 237] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 7. | Goei TH, van Berge Henegouwen MI, Slooff MJ, van Gulik TM, Gouma DJ, Eddes EH. Pylorus-preserving pancreatoduodenectomy: influence of a Billroth I versus a Billroth II type of reconstruction on gastric emptying. Dig Surg. 2001;18:376-380. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 48] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Miedema BW, Sarr MG, van Heerden JA, Nagorney DM, McIlrath DC, Ilstrup D. Complications following pancreaticoduodenectomy. Current management. Arch Surg. 1992;127:945-949; discussion 949-950. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 267] [Cited by in F6Publishing: 299] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 9. | Park YC, Kim SW, Jang JY, Ahn YJ, Park YH. Factors influencing delayed gastric emptying after pylorus-preserving pancreatoduodenectomy. J Am Coll Surg. 2003;196:859-865. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 125] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | van Berge Henegouwen MI, van Gulik TM, DeWit LT, Allema JH, Rauws EA, Obertop H, Gouma DJ. Delayed gastric emptying after standard pancreaticoduodenectomy versus pylorus-preserving pancreaticoduodenectomy: an analysis of 200 consecutive patients. J Am Coll Surg. 1997;185:373-379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Kimura F, Suwa T, Sugiura T, Shinoda T, Miyazaki M, Itoh H. Sepsis delays gastric emptying following pylorus-preserving pancreaticoduodenectomy. Hepatogastroenterology. 2002;49:585-588. [PubMed] [Cited in This Article: ] |
| 12. | Riediger H, Makowiec F, Schareck WD, Hopt UT, Adam U. Delayed gastric emptying after pylorus-preserving pancreatoduodenectomy is strongly related to other postoperative complications. J Gastrointest Surg. 2003;7:758-765. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 13. | Räty S, Sand J, Lantto E, Nordback I. Postoperative acute pancreatitis as a major determinant of postoperative delayed gastric emptying after pancreaticoduodenectomy. J Gastrointest Surg. 2006;10:1131-1139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Yeo CJ, Barry MK, Sauter PK, Sostre S, Lillemoe KD, Pitt HA, Cameron JL. Erythromycin accelerates gastric emptying after pancreaticoduodenectomy. A prospective, randomized, placebo-controlled trial. Ann Surg. 1993;218:229-237; discussion 237-238. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 274] [Cited by in F6Publishing: 292] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 15. | Fabre JM, Burgel JS, Navarro F, Boccarat G, Lemoine C, Domergue J. Delayed gastric emptying after pancreaticoduodenectomy and pancreaticogastrostomy. Eur J Surg. 1999;165:560-565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 41] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761-768. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1771] [Cited by in F6Publishing: 2043] [Article Influence: 120.2] [Reference Citation Analysis (0)] |
| 17. | Kawai M, Tani M, Hirono S, Miyazawa M, Shimizu A, Uchiyama K, Yamaue H. Pylorus ring resection reduces delayed gastric emptying in patients undergoing pancreatoduodenectomy: a prospective, randomized, controlled trial of pylorus-resecting versus pylorus-preserving pancreatoduodenectomy. Ann Surg. 2011;253:495-501. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 144] [Cited by in F6Publishing: 149] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 18. | Kawai M, Yamaue H. Pancreaticoduodenectomy versus pylorus-preserving pancreaticoduodenectomy: the clinical impact of a new surgical procedure; pylorus-resecting pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2011;18:755-761. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Kurahara H, Shinchi H, Maemura K, Mataki Y, Iino S, Sakoda M, Ueno S, Takao S, Natsugoe S. Delayed gastric emptying after pancreatoduodenectomy. J Surg Res. 2011;171:e187-e192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Oida T, Mimatsu K, Kano H, Kawasaki A, Fukino N, Kida K, Kuboi Y, Amano S. Antecolic and retrocolic route on delayed gastric emptying after MSSPPD. Hepatogastroenterology. 2012;59:1274-1276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 21. | Oida T, Mimatsu K, Kano H, Kawasaki A, Kuboi Y, Fukino N, Amano S. Preventing delayed gastric emptying in pancreaticogastrostomy by a modified subtotal-stomach-preserving pancreaticoduodenectomy: Oida modification. Hepatogastroenterology. 2011;58:1384-1388. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Eshuis WJ, van Dalen JW, Busch OR, van Gulik TM, Gouma DJ. Route of gastroenteric reconstruction in pancreatoduodenectomy and delayed gastric emptying. HPB (Oxford). 2012;14:54-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 23. | Inoue K, Tobe T, Suzuki T, Hosotani R, Kogire M, Fuchigami A, Miyashita T, Tsuda K, Seino Y. Plasma cholecystokinin and pancreatic polypeptide response after radical pancreatoduodenectomy with Billroth I and Billroth II type of reconstruction. Ann Surg. 1987;206:148-154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Gangavatiker R, Pal S, Javed A, Dash NR, Sahni P, Chattopadhyay TK. Effect of antecolic or retrocolic reconstruction of the gastro/duodenojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a randomized controlled trial. J Gastrointest Surg. 2011;15:843-852. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 25. | Ueno T, Takashima M, Iida M, Yoshida S, Suzuki N, Oka M. Improvement of early delayed gastric emptying in patients with Billroth I type of reconstruction after pylorus preserving pancreatoduodenectomy. J Hepatobiliary Pancreat Surg. 2009;16:300-304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Masui T, Doi R, Kawaguchi Y, Uemoto S. Delayed gastric emptying improved by straight stomach reconstruction with twisted anastomosis to the jejunum after pylorus-preserving pancreaticoduodenectomy (PPPD) in 118 consecutive patients at a single institution. Surg Today. 2012;42:441-446. [PubMed] [Cited in This Article: ] |
| 27. | Chijiiwa K, Imamura N, Ohuchida J, Hiyoshi M, Nagano M, Otani K, Kai M, Kondo K. Prospective randomized controlled study of gastric emptying assessed by (13)C-acetate breath test after pylorus-preserving pancreaticoduodenectomy: comparison between antecolic and vertical retrocolic duodenojejunostomy. J Hepatobiliary Pancreat Surg. 2009;16:49-55. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Caronna R, Cardi M, Sammartino P, Mangioni S, Pittau G, Scozzafava S, Catinelli S, Chirletti P, Stipa V. Functional results of a personal technique of reconstruction after pancreaticoduodenectomy. J Exp Clin Cancer Res. 2003;22:187-189. [PubMed] [Cited in This Article: ] |
| 29. | Chirletti P, Peparini N, Caronna R, Papini F, Vietri F, Gualdi G. Monitoring fibrosis of the pancreatic remnant after a pancreaticoduodenectomy with dynamic MRI: are the results independent of the adopted reconstructive technique? J Surg Res. 2010;164:e49-e52. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Caronna R, Peparini N, Cosimo Russillo G, Antonio Rogano A, Dinatale G, Chirletti P. Pancreaticojejuno anastomosis after pancreaticoduodenectomy: brief pathophysiological considerations for a rational surgical choice. Int J Surg Oncol. 2012;2012:636824. [PubMed] [Cited in This Article: ] |