Published online Apr 7, 2010. doi: 10.3748/wjg.v16.i13.1673
Revised: January 5, 2010
Accepted: January 12, 2010
Published online: April 7, 2010
The most frequent health problems seen in senility are chronic and degenerative diseases. A 75-year-old male patient with the complaints of weight loss and difficulty in swallowing was admitted to our hospital from a nursing home. Upper system fiber-optic gastrointestinal endoscopy was performed and a mass at the junction of the hypopharynx and esophagus just below recessus piriformis obstructing almost the whole of the lumen and blocking the distal passage was detected. Computed tomography revealed marked narrowing secondary to osseous hypertrophy in the air column of the hypopharynx and proximal esophagus. Diffuse idiopathic skeletal hyperostosis or Forestier’s disease is an idiopathic disease characterized by the ossification of the anterior longitudinal ligament of vertebra and some of the extraspinal ligaments. In the present case we aim to discuss an elderly patient who suffered from dysphagia and weight loss and the diagnostic stages.
- Citation: Karadag B, Cat H, Aksoy S, Ozulu B, Ozturk AO, Oguz S, Altuntas Y. A geriatric patient with diffuse idiopathic skeletal hyperostosis. World J Gastroenterol 2010; 16(13): 1673-1675
- URL: https://www.wjgnet.com/1007-9327/full/v16/i13/1673.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i13.1673
Diffuse idiopathic skeletal hyperostosis (DISH) is a common but often unrecognized systemic disorder observed mainly in elderly people[1]. All papers related to DISH demonstrate a consistent and marked increase of the disease with advancing age[2]. Various local structural lesions such as oropharyngeal tumors, vascular pathologies, retropharyngeal abscesses, and anterior cervical osteophytes may lead to mechanical esophageal dysphagia[3-5]. The prevalence of DISH in adults over the age of 50 years is around 25% for men and 15% for women, with an increased incidence in patients with obesity, gout and diabetes[6].
Although most patients with cervical spine involvement are either asymptomatic or have limited cervical spine movement and unspecified pain, possible complications described in the literature are dysphagia[7], stridor[8] dyspnea[9], ossification of the posterior longitudinal ligament and/or myelopathy[10] and hoarseness[11].
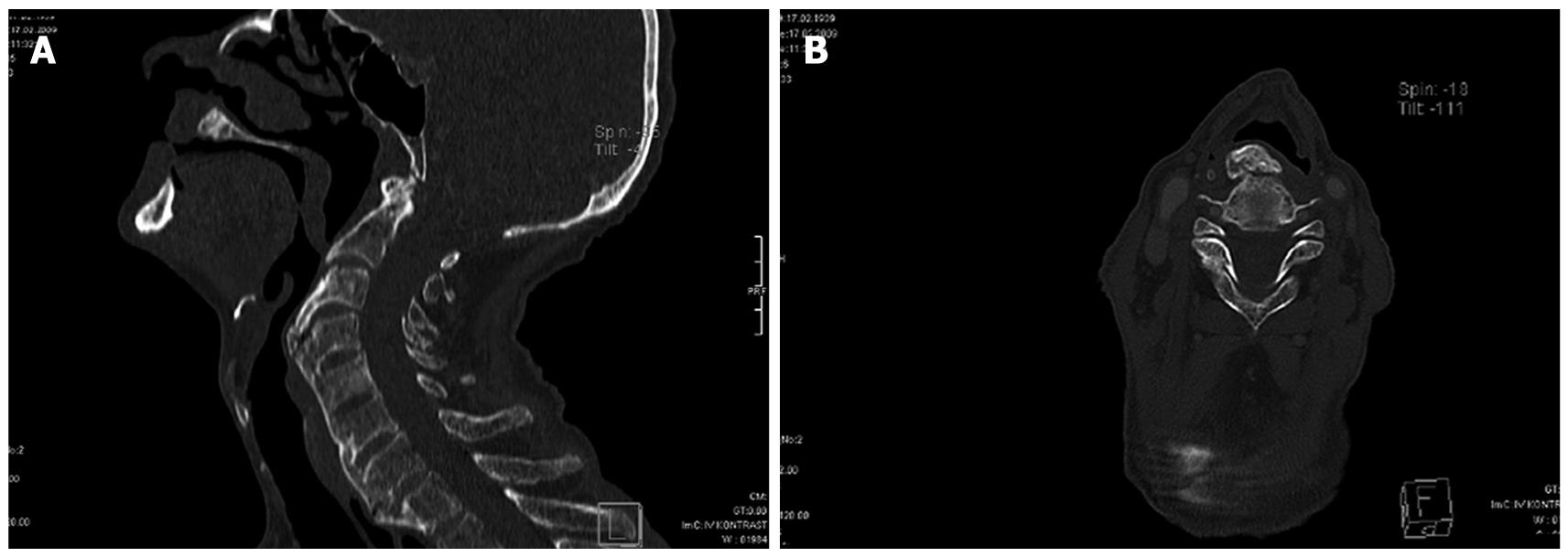
A 75-year-old male patient was found drunk and unconscious on the street in November 9, 2008 and was transferred to the nearest state hospital. After an operation for intertrochanteric femur fracture he was sent to a nursing home. Because of progressive weight loss and swallowing difficulty, some blood tests were done and Hb and erythrocyte sedimentation rate (ESR) were found to be 9 g/dL and 75 mm/h, respectively. The patient was then transferred to our hospital on 28 January, 2009 with the preliminary diagnosis of malignancy. His height was 160 cm, weight 41 kg and body mass index was 16 kg/m2. Physical examination revealed only cachectic appearance and limited neck movements; the other findings were normal, and the thyroid gland was nonpalpable. Due to detected anemia two packs of erythrocyte suspensions were transfused. In the biochemical analyses hepatic and renal functions were normal; he didn’t have any electrolyte imbalance or systemic disease (fasting plasma glucose: 79 mg/dL, blood urea nitrogen: 22 mg/dL, creatinine: 1.0 mg/dL, uric acid: 4.8 mg/dL, aspartate aminotransferase: 8 U/L, alanine aminotransferase: 3 U/L, potassium: 4.3 mmol/L, iron: 41 μg/dL total iron binding capacity: 173 μg/L). His vitamin B12 and folic acid levels were 57 pg/mL and 1.46 ng/mL respectively. Total protein value was 5.7 g/dL and albumin was 2.3 g/dL. Evaluation of cognitive functions revealed his Mini Mental State Examination score was 12. There was not any evidence for malignancy in his thoracic and abdominal CT scans. Upper system fiber-optic gastrointestinal endoscopy was performed and a mass at the junction of the hypopharynx and esophagus just below recessus piriformis obstructing almost whole of the lumen and blocking the distal passage was detected. Biopsy couldn’t be performed because of the risk of bleeding and aspiration. As a result of ear-nose-throat clinic consultation, and after laryngoscopic examination, anesthesia confirmation and cervical CT was performed for taking a biopsy from the mass thought to have originated from the pharyngeal area. Cervical CT revealed hypertrophic bridging alterations of anterior corpus parts at the level of C3-T1 vertebra (Figure 1A and B). At the hypopharynx and proximal parts of esophagus restriction secondary to osseous hypertrophy was demonstrated and this aspect was evaluated as consistent with DISH or Forrestier disease. As a result of multidisciplinary evaluation, an operation wasn’t planned because of the patient’s poor general condition. Patient’s nutrition was regulated with fluid foods. No problem was established during nutrition with fluids. The patient was sent back to nursing home after recovery of general status.
Although mortality decreases and life expectancy gets longer with developing technology and medicine, chronic diseases remain common problems of elderly patients. In the differential diagnosis for dysphagia, larynx, lung and mediastinal tumors, esophagus motility disorders, esophagitis, restriction of esophagus, spinal tumors, vascular abnormalities, Zencker diverticule, Plummer-Vinson syndrome, gastroesophageal reflux and globus histericus should be kept in mind. For differentiating these disorders barium esophagography has a great importance[12].
A medical history should be taken in detail and questions about anatomical structure and functions of the oral cavity, pharynx, larynx, and esophagus should be examined when a patient complaining of dysphagia applies to ear-nose and throat clinics. Physical examination of the oral cavity, pharynx, larynx and neck should be done for determining the possible pathologies. Esophageal cancer, web, achalasia, diffuse esophageal spasm and esophagitis are common causes of esophageal dysphagia. Rarely, mediastinal tumors pressing the esophagus, vertebral bone processes and impressions due to the aorta can be the causes[13]. In our case, the patient’s complaints were anemia, weight loss and difficulty in swallowing and initially esophageal malignancy was thought to be the cause of these complaints and upper gastrointestinal system endoscopy was planned. As a result of these evaluations, hypertrophic bridging alterations of anterior corpus parts at the level of C3-T1 vertebra were revealed. It was reported that perforation during esophagoscopy improves because of compression due to cervical osteophytes[14].
Treatment for DISH is primarily conservative, nonsteroidal anti-inflammatory drugs and myorelaxants are used. But in refractory cases there are two surgical approaches to remove osteophytes by lateral cervical or peroral transpharyngeal ways[15]. In our case, we initially preferred a medical approach and started treatment with anti-inflammatory drugs and nutrition with liquid foods, after recovery of oral intake we maintained with high calorie formulas.
In our case, the patient hadn’t applied to any hospital in the period that he lived alone but after he began to stay in the nursing home for elderly these complaints and problems were established and he was transferred to our hospital. At the present time, it is emphasized that without increasing the quality of the life, longer life will have no meaning and health expectancy is more important than life expectancy. Consequently, while treatment is the target in a young population, in a geriatric population the main target is the preservation of quality of life. We avoided the complications of surgical management and anesthesia, we tried nutrition with liquids and facilitated oral intake. Eventually, recovery in our patient’s status and weight gain started. Gastrostomy may be planned if necessary and the patient is followed at particular intervals. During the evaluation of elderly patients, social status, cognitive functions and exhaustive physical examination should be performed definitely.
In conclusion, DISH should be considered an important, although rare, cause of dysphagia among older adults. However, it should not be accepted as the cause of dysphagia until all other causes have been ruled out.
Peer reviewers: Dr. Shahab Abid, Associate Professor, Department of Medicine, Aga Khan University, Stadium Road, PO Box 3500, Karachi 74800, Pakistan; Jai Dev Wig, MS, FRCS, Former Professor and Head, Department of General Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh 160012, India
S- Editor Wang YR L- Editor O’Neill M E- Editor Ma WH
| 1. | Belanger TA, Rowe DE. Diffuse idiopathic skeletal hyperostosis: musculoskeletal manifestations. J Am Acad Orthop Surg. 2001;9:258-267. |
| 2. | Weinfeld RM, Olson PN, Maki DD, Griffiths HJ. The prevalence of diffuse idiopathic skeletal hyperostosis (DISH) in two large American Midwest metropolitan hospital populations. Skeletal Radiol. 1997;26:222-225. |
| 3. | Lambert JR, Tepperman PS, Jimenez J, Newman A. Cervical spine disease and dysphagia. Four new cases and a review of the literature. Am J Gastroenterol. 1981;76:35-40. |
| 4. | Srinivas P, George J. Cervical osteoarthropathy: an unusual cause of dysphagia. Age Ageing. 1999;28:321-322. |
| 5. | Uzunca K, Birtane M, Tezel A. Dysphagia induced by a cervical osteophyte: Acase report of cervical spondylosis. Chin Med J (Engl). 2004;117:478-480. |
| 6. | Masiero S, Padoan E, Bazzi M, Ponzoni A. Dysphagia due to diffuse idiopathic skeletal hyperostosis: an analysis of five cases. Rheumatol Int. 2010;30:681-685. |
| 7. | Masiero S, Marchese Ragona R, Bottin R, Volante D, Ortolani M. An unusual cause of aspiration pneumonia. Aging Clin Exp Res. 2006;18:78-82. |
| 8. | Curtis JR, Lander PH, Moreland LW. Swallowing difficulties from “DISH-phagia”. J Rheumatol. 2004;31:2526-2527. |
| 9. | Nelson RS, Urquhart AC, Faciszewski T. Diffuse idiopathic skeletal hyperostosis: a rare cause of Dysphagia, airway obstruction, and dysphonia. J Am Coll Surg. 2006;202:938-942. |
| 10. | Epstein NE. Simultaneous cervical diffuse idiopathic skeletal hyperostosis and ossification of the posterior longitudinal ligament resulting in dysphagia or myelopathy in two geriatric North Americans. Surg Neurol. 2000;53:427-431; discussion 431. |
| 11. | Kritzer RO, Rose JE. Diffuse idiopathic skeletal hyperostosis presenting with thoracic outlet syndrome and dysphagia. Neurosurgery. 1988;22:1071-1074. |
| 12. | Rotés-Querol J. Clinical manifestations of diffuse idiopathic skeletal hyperostosis (DISH). Br J Rheumatol. 1996;35:1193-1194. |
| 13. | Alper F, Akgun M, Kantarci M, Eroglu A, Ceyhan E, Onbas O, Duran C, Okur A. Demonstration of vascular abnormalities compressing esophagus by MDCT: special focus on dysphagia lusoria. Eur J Radiol. 2006;59:82-87. |
| 14. | Vrouenraets BC, Been HD, Brouwer-Mladin R, Bruno M, van Lanschot JJ. Esophageal perforation associated with cervical spine surgery: report of two cases and review of the literature. Dig Surg. 2004;21:246-249. |
| 15. | Uppal S, Wheatley AH. Transpharyngeal approach for the treatment of dysphagia due to Forestier's disease. J Laryngol Otol. 1999;113:366-368. |