Copyright
©2010 Baishideng.
World J Gastroenterol. Mar 21, 2010; 16(11): 1304-1313
Published online Mar 21, 2010. doi: 10.3748/wjg.v16.i11.1304
Published online Mar 21, 2010. doi: 10.3748/wjg.v16.i11.1304
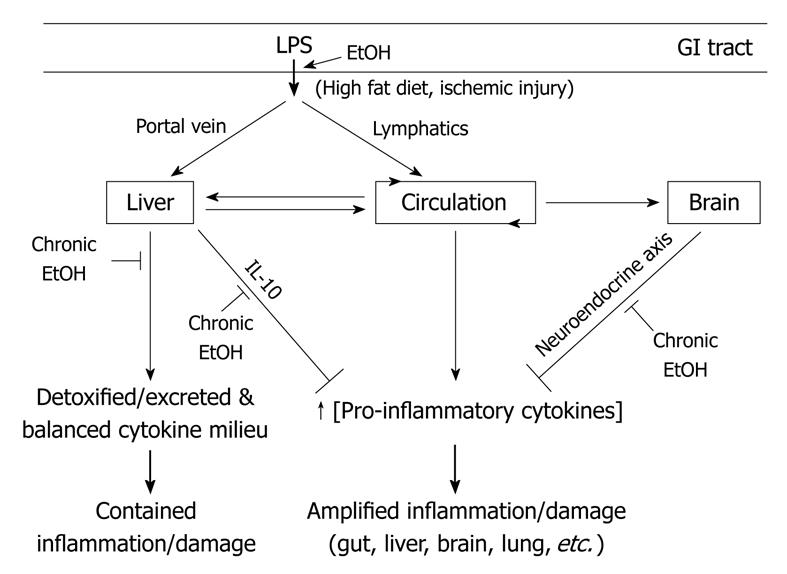
Figure 1 Gut microflora derived lipopolysaccharide (LPS)-dissemination, detoxification, and multi-organ host response and effects of alcohol use.
A number of key events in LPS translocation and host response are depicted. First, upon translocation across the gut barrier, LPS enters circulation via two different routes: the portal vein or lymphatic vessels. LPS in the portal vein is directly delivered to the liver and most of it is detoxified and excreted, whereas most LPS in lymphatics are released into the circulation at the thoracic duct opening. Between the two routes, portal dissemination is dominant under normal conditions whereas a few known conditions including fatty diet and ischemic injury stimulate lymphatic dissemination. Second, a healthy liver plays a key role in the detoxification of LPS in the portal vein and systemic circulation but also generates a balanced cytokine milieu that lead to a contained inflammation and limited damage. Third, LPS in circulation is accessible to many organs and plays a major role in multi-organ damage, especially when LPS detoxification in liver is compromised. Lastly, LPS and its immune mediators (pro-inflammatory cytokines) can activate the neuroendocrine response in the central nervous system (CNS) that leads to the activation of the hypothalamo-pituitary-adrenal (HPA) axis and then the synthesis of cortisol, which down-regulates inflammatory responses in the periphery. A number of key sites under alcohol influence are depicted. First, alcohol enhances LPS translocation across the gut barrier by increasing microflora content and impairing gut barrier function. Second, alcohol stimulates LPS dissemination via lymphatics, evidenced by a rapid rise in circulating LPS in healthy animals fed with acute alcohol. The potential use of the portal route remains to be determined. Third, chronic alcohol use not only adversely affects the liver’s ability to detoxify LPS but also affects the liver’s ability to synthesize a key anti-inflammatory cytokine, interleukin (IL)-10. Lastly, chronic alcohol reduces the synthesis of neuroendocrine effectors that regulate systemic inflammation. Together, chronic alcohol impairs the balance of microflora in the gut, gut barrier function, the liver’s ability to detoxify bacterial products and to generate a balanced cytokine milieu, and the brain’s ability to regulate inflammation in the periphery. GI: Gastrointestinal.
- Citation: Wang HJ, Zakhari S, Jung MK. Alcohol, inflammation, and gut-liver-brain interactions in tissue damage and disease development. World J Gastroenterol 2010; 16(11): 1304-1313
- URL: https://www.wjgnet.com/1007-9327/full/v16/i11/1304.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i11.1304