Published online Nov 28, 2009. doi: 10.3748/wjg.15.5620
Revised: October 28, 2009
Accepted: November 4, 2009
Published online: November 28, 2009
Lymphangioma, a benign neoplasm of the lymphatic system, is common in children but rare in adults. Its clinical manifestations include abdominal pain, nausea, vomiting and a palpable mass. However, abdominal sonography or abdominal computed tomography (CT) scan can also incidentally reveal lymphangioma. A larger or symptomatic lymphangioma is treated with total resection to prevent recurrence, infection, torsion and enlargement. Although lymphangioma rarely becomes malignant, its prognosis is generally good. We report a cystic lymphangioma of the spleen and retroperitoneum, which was incidentally found in a 56-year-old man who was hospitalized due to a colon mass. Physical examination showed no specific findings. Abdominal CT revealed a 5.7 cm, non-enhanced multilobulated cystic mass with multiple septa in the spleen and a 10 cm lobulated cystic mass in the paraaortic area. Splenectomy and retroperitoneal resection of the cystic mass were conducted. The endothelium of splenic and retroperitoneal cyst was immunohistochemically stained with D2-40 antibody. The patient was finally diagnosed with splenic cystic and retroperitoneal cavernous lymphangioma.
- Citation: Chung SH, Park YS, Jo YJ, Kim SH, Jun DW, Son BK, Jung JY, Baek DH, Kim DH, Jung YY, Lee WM. Asymptomatic lymphangioma involving the spleen and retroperitoneum in adults. World J Gastroenterol 2009; 15(44): 5620-5623
- URL: https://www.wjgnet.com/1007-9327/full/v15/i44/5620.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.5620
Lymphangioma, a very uncommon neoplasm, is mainly found in children but rarely in adults[1,2]. In 1885, Frink reported the first lymphangioma in the spleen. Cases of splenic and retroperitoneum lymphangioma are rarely reported in adults. In our case, lymphangioma involved both the spleen and the retroperitoneum. Cases like ours, involving two organs, are extremely rare[3-5]. The clinical manifestations of lymphangioma include abdominal pain, fever, fatigue, weight loss and hematuria. However, it is sometimes asymptomatic[6,7]. We report, here, a case of a 56-year-old man who was hospitalized due to a colon mass. Lymphangioma in his spleen and retroperitoneum was incidentally found in abdominal computed tomography (CT). This case is very rare because lymphangioma was found both in his spleen and in his retroperitoneum.
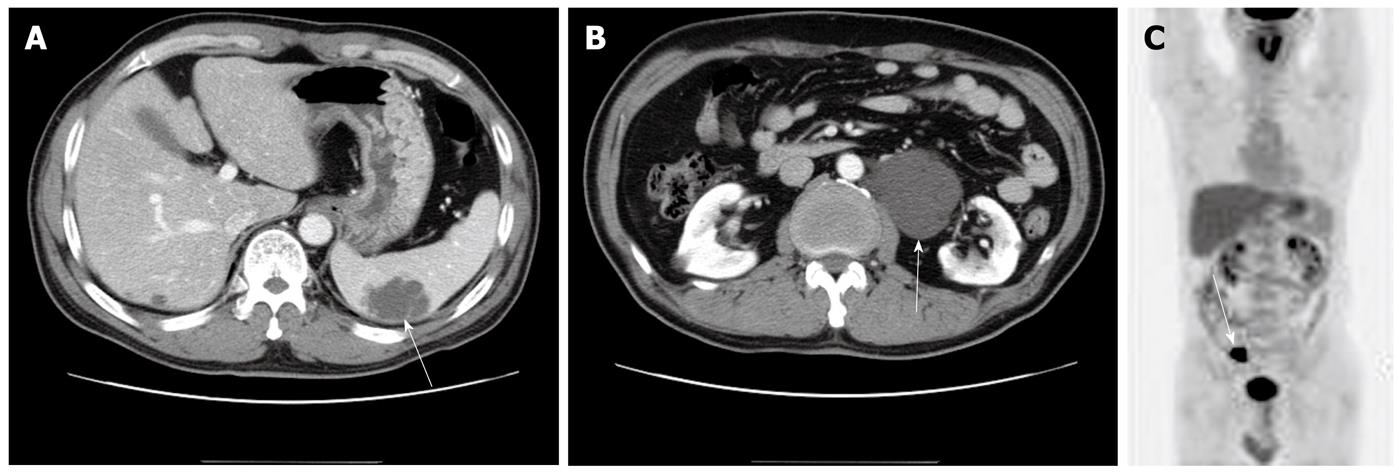
A 56-year-old man was hospitalized at a private clinic due to a suspected colon cancer detected at colonoscopy. He had no history of any medical disease, and no weight loss, abdominal pain and dyspepsia. Physical examination revealed no palpable mass, tenderness or rebound tenderness in his abdomen with normal bowel sound. Laboratory studies had no specific findings except for creatinine (1.4 mg/dL). Abdominal X-ray did not reveal calcification, but abdominal CT showed a 5.7 cm non-enhanced cystic mass with septum in the spleen and a 10 cm lobulated cystic mass in the left paraaortic area (Figure 1A and B). PET CT revealed a hypermetabolic lesion in the sigmoid colon where the maxSUV was 23. However, no hypermetabolic lesion was found in the spleen or in the left paraaortic area (Figure 1C).
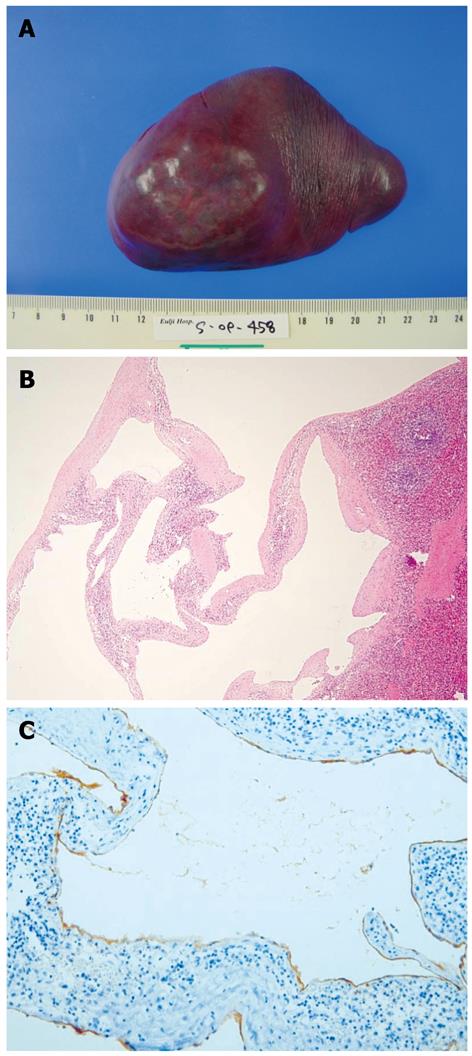
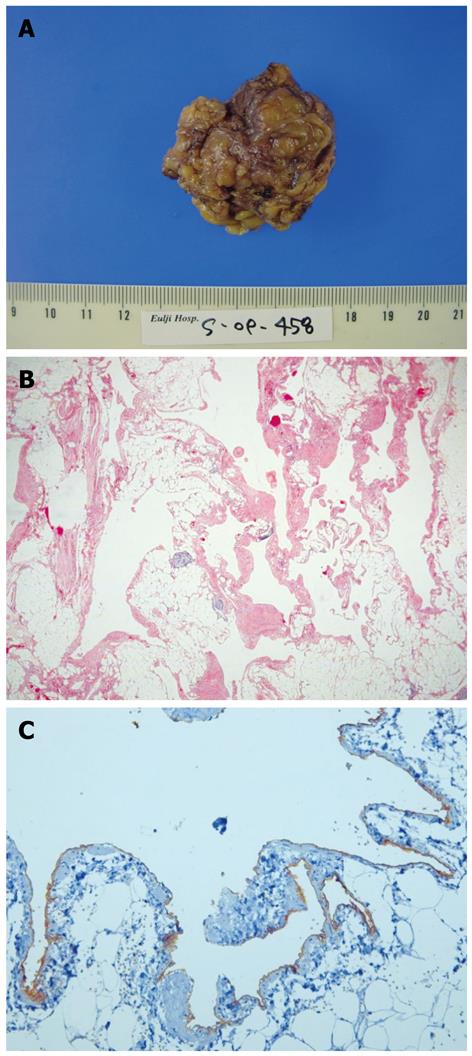
A 5 cm × 3 cm colon polyp with a neck and an intramural adenocarcinoma invading the lamina propria were found in the sigmoid colon. Splenectomy and resection of the retroperitoneal mass were conducted, during which a 4.5 cm × 3.5 cm bulging mass was exposed in the lower pole of the spleen (Figure 2A). The cut surface was composed of a multilobular cyst with a smooth inner surface. Histology showed thin fibrous walls of the cyst, which were different in size with no bleeding or necrosis (Figure 2B). In immunohistochemical study, the endothelium of splenic cystic mass was stained with D2-40 antibody (Figure 2C) and finally diagnosed as a cystic lymphangioma. The retroperitoneal mass was 4.5 cm × 4.5 cm × 2.5 cm in size, and its outer surface was lobular and yellow to brown in color (Figure 3A). The cut surface showed a sponge-like and ill-defined cyst.
Histology showed small cysts interspersed among fat, which were different in size, but had no calcification, bleeding, or necrosis (Figure 3B). In immunohistochemical study, the endothelium of retroperitoneal cystic mass was stained with D2-40 antibody (Figure 3C). The retroperitoneal mass was finally diagnosed as a cavernous lymphangioma. The patient was discharged 10 d after operation without complication.
Cystic lymphangioma is a benign neoplasm composed of a malformation of the lymphatic system[1,2]. The incidence of lymphangioma occurring after 20 years of age is very low. Lymphangioma generally occurs under the age of 2 years. There is no difference in the incidence between males and females[2]. The most commonly involved sites are the neck (75%) and axilla (20%). Lymphangioma is infrequently encountered in the mediastinum, adrenal gland, kidney, bone, omentum, gastrointestinal track, retroperitoneum, spleen, liver and pancreas[2,5]. There are two hypotheses for the causes and pathogenesis of lymphangioma, namely abnormal congenital development and bleeding or inflammation of the lymphatic system which causes an obstruction leading to additional lymphangiomas. The clinical manifestations of lymphangioma are left upper quadrant pain, abdominal distension, loss of appetite, nausea, vomiting and a palpable mass. However, lymphangioma can also occur without any symptoms[6,7]. Our case had no symptoms of lymphangioma and no palpable mass in the abdomen, and is unique because lymphangioma was found both in his spleen and in his retroperitoneum. Even if there are reports on cystic lymphangioma involving mesentery and retroperitoneum[2], no report is available on lymphangioma involving both the spleen and the retroperitoneum in an asymptomatic patient. Lymphangioma involving more than two abdominal organs is rarely reported[2]. In our case, renal vein penetrated through the retroperitoneal lymphangioma, but retroperitoneal lymphangioma could be resected without impairment of the kidneys. Abdominal sonography can show a lowly attenuated mass and a highly attenuated inner part of lymphangioma, while abdominal CT may demonstrate multiple lowly attenuated, thin-walled, well-demarcated cysts and calcification in the cyst wall. The cystic surface can be divided by a septum and multiple lobules[7]. MRI may reveal a highly attenuated space in multiple lobules. Only a radiological image may have limitations in its diagnosis[6,7]. In this case, abdominal CT revealed a 5.7 cm cystic mass in the spleen and a 10 cm cystic mass composed of lobules in the paraaortic area. PET CT did not show highly metabolized lesions in the spleen or in the retroperitoneum of our case. Generally, lymphangioma is divided into capillary, cavernous and cystic types, with the cystic type being the most common[3]. Histology can show dilated lymphatic vessels surrounded by flat endothelial cells between fat, fibrotic and lymphatic structures. Immunohistochemical staining can show a lymphangioma which is positive for keratin and HBME, and is negative for FV III-Rag, CD 31, CD 34 because it develops from the middle lobe[8]. Lymphatic vessel endothelial receptor-1, vascular endothelial growth factor-3, prox-1, and monoclonal antibody D2-40 are the markers for specific endothelial cells of lymphatic tissues, which are used in immunochemical studies of lymphangioma. In this case, the endothelium of splenic and retroperitoneal cystic mass was stained with D2-40 antibody and the splenic and retroperitoneal cystic mass was finally diagnosed as splenic cystic and retroperitoneal cavernous lymphangioma, based on the microscopic findings. Surgical treatment is needed to prevent recurrence, infection, rupture, and bleeding[5]. Conservative treatment modalities include aspiration, drainage and sclerosis, with a high risk of recurrence. However, an incidentally found small cyst needs not be resected, and the current treatment is a partial splenectomy to remove it[5]. The post-operative recurrence rate is low and the rate of transformation into malignancy is very low as well. Complications are peritonitis, bleeding, abscess and torsion[9]. The natural regression rate is very low. If multiple lymphangiomas progress rapidly and are invasive, their prognosis could be poor[10]. In this case, a 5.7 cm splenic lymphangioma and a 10 cm lymphangioma were surgically removed and the patient was discharged 10 d later without any complication. Our case may be the first reported case of lymphangioma involving both the spleen and the retroperitoneum in an asymptomatic patient.
Peer reviewers: Domenico Sansonno, Professor, Department of Internal Medicine and Clinical Oncology, University of Bari Medical School, Policlinico, Piazza Giulio Cesare 11, 70124 Bari, Italy; Qin Su, Professor, Department of Pathology, Cancer Hospital and Cancer Institute, Chinese Academy of Medical Sciences and Peking Medical College, PO Box 2258, Beijing 100021, China
S- Editor Tian L L- Editor Wang XL E- Editor Zheng XM
| 1. | de Perrot M, Rostan O, Morel P, Le Coultre C. Abdominal lymphangioma in adults and children. Br J Surg. 1998;85:395-397. [Cited in This Article: ] |
| 2. | Kim DH, Byun JN, Jang JY. Cystic lymphangioma involving the mesentery and the retroperitoneum: A case report. J Korean Radiol Soc. 2005;52:347-350. [Cited in This Article: ] |
| 3. | Takayama A, Nakashima O, Kobayashi K, Kojiro M. Splenic lymphangioma with papillary endothelial proliferation: a case report and review of the literature. Pathol Int. 2003;53:483-488. [Cited in This Article: ] |
| 4. | Cherk M, Nikfarjam M, Christophi C. Retroperitoneal lymphangioma. Asian J Surg. 2006;29:51-54. [Cited in This Article: ] |
| 5. | Chang CH, Hsieh CB, Yu JC, Jan CI. A case of lymphangioma of the spleen. J Med Sci. 2004;24:109-112. [Cited in This Article: ] |
| 6. | Chan IYF, Khoo J. Retroperitoneal lymphangioma in an adult. J HK Coll Radiol. 2003;6:94-96. [Cited in This Article: ] |
| 7. | Kwon AH, Inui H, Tsuji K, Takai S, Imamura A, Kamiyama Y. Laparoscopic splenectomy for a lymphangioma of the spleen: report of a case. Surg Today. 2001;31:258-261. [Cited in This Article: ] |
| 8. | Kim MJ, Cho KJ, Han EM, Lee YJ. Splenic lymphangioma: A report of three cases. Korean J Pathol. 2002;36:416-419. [Cited in This Article: ] |
| 9. | Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, Hwang HY. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004;24:1353-1365. [Cited in This Article: ] |