Published online Aug 7, 2009. doi: 10.3748/wjg.15.3681
Revised: May 24, 2009
Accepted: May 31, 2009
Published online: August 7, 2009
Bilhemia or bile mixing with blood is a rare clinical problem. The clinical presentation is usually transient self-resolving hyperbilirubinemia, progressive and rapidly rising conjugated hyperbilirubinemia, or recurrent cholangitis. Endoscopic retrograde cholangiopancreatography (ERCP) plays an important role in diagnosis and management. Biliary decompression with endoscopic sphincterotomy is useful in treating these patients. If not recognized and treated in time, the condition can be fatal in a significant proportion of patients. This usually occurs after blunt or penetrating hepatic trauma due to a fistulous connection between the biliary radicle and portal or hepatic venous radical. Cases have been described due to iatrogenic trauma such as liver biopsy and percutaneous biliary drainage. However, the occurrence after trans-jugular intra-hepatic porto-systemic shunt (TIPS) is very rare. We report a case of bilhemia presenting as rapidly rising bilirubin after TIPS. The patient was managed successfully with ERCP and removal of a blood clot from the common bile duct.
- Citation: Singal AK, Kathuria MK, Malhotra A, Goodgame RW, Soloway RD. Bilhemia after trans-jugular intra-hepatic porto-systemic shunt and its management with biliary decompression. World J Gastroenterol 2009; 15(29): 3681-3683
- URL: https://www.wjgnet.com/1007-9327/full/v15/i29/3681.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3681
Transjugular intrahepatic portosystemic shunt (TIPS) is a frequently performed procedure to achieve decompression of the portal venous system in the treatment of (1) uncontrolled acute variceal bleeding, (2) prevention of recurrent variceal bleeding, (3) refractory ascites, and (4) hepatic hydrothorax[1]. Early complications (within 24-48 h) include intraperitoneal bleeding, shunt occlusion, vascular fistulae, and hepatic infarction. We report a case of bilhemia (bile mixing with blood) after TIPS which was successfully managed with endoscopic decompression of the biliary system.
A 73 year-old Caucasian female with sarcoidosis-associated cirrhosis underwent TIPS for the treatment of refractory hepatic hydrothorax. The diagnosis of cirrhosis was made in 2002 based on liver biopsy findings. The patient had a history of cholecystectomy in the remote past. Evaluation of liver function tests in 2002-2003 showed total bilirubin (TB) 1.8 mg/dL, alkaline phosphatase (ALP) 560 IU/L, aspartate aminotransferase (AST) 87 IU/L, alanine aminotransferase (ALT) 63 IU/L, total proteins (TP) 7.1 g/dL and albumin 3.4 g/dL. Ascites was managed with diuretics and salt restriction until December 2008 when she developed shortness of breath. Due to closure of our institution during Hurricane Ike, she was referred to another hospital. On work-up she was found to have pleural effusion on the right side. The pleural fluid was transudate with a serum-fluid albumin gradient > 1.1, consistent with hepatic hydrothorax. As she required repeated thoracocentesis, pleurodesis was tried using talc, however, this was unsuccessful. In mid January, an indwelling pleural catheter was placed in her right pleural cavity. In early February 2009, she came back to us for follow up after our institution reopened. The catheter was draining about 500-1000 cc every day. The patient did not show any clinical evidence of infection. Placement of an indwelling catheter or a chest tube is not recommended for the management of hepatic hydrothorax[2]. Therefore, it was decided to control her hydrothorax with TIPS to be followed by the removal of the chest catheter at a later date.
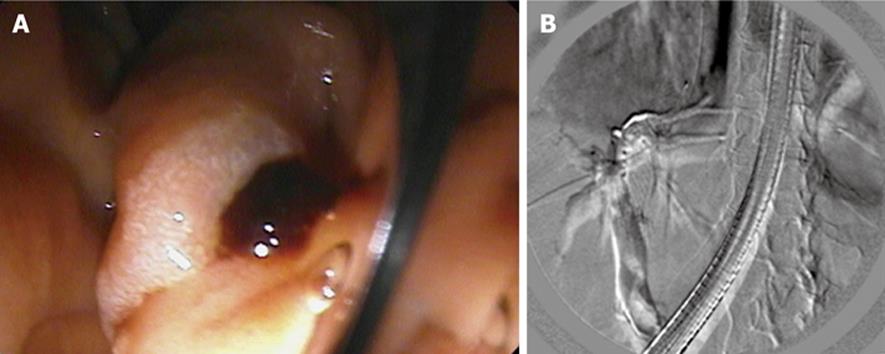
Laboratory parameters prior to TIPS were: TB 0.4 mg/dL, albumin: 2.8 g/dL, ALP 259 IU/L, ALT-33 IU/L, AST52 IU/L, international normalized ratio (INR) 1.1, hemoglobin 11.7 g/dL and serum creatinine 0.7 mg/dL. During the procedure while attempting to cannulate the hepatic vein, the interventional radiologist noticed the presence of bile in the catheter. However, the shunt was placed between the right hepatic vein and the right main branch of the portal vein using a 1 cm × 7 cm polytetrafluorourethane covered stent (Gore Viatorr, USA). The procedure was successful in achieving decompression of the portal venous system with a reduction of the portosystemic gradient from 16 before TIPS to 0 after the procedure. Post -procedure the patient remained in hospital to determine the amount of drainage from the pleural catheter in order to decide on its removal. The patient was doing well until the second day after the procedure, when she was noted to be diffusely yellow. Laboratory evaluation at this time showed hemoglobin to be 11.7 g/dL, white blood cell count 11.9/cubic mL, INR 1.2, creatinine 0.7 mg/dL, TB 15.9 mg/dL, conjugated bilirubin 15.2 g/dL, AST 183 IU/L, ALT 71 IU/L, and ALP 409 IU/L. She denied any abdominal pain or fever and there was no change in her mental status. The next day her bilirubin increased to 22.4 mg/dL. A CT scan of the abdomen showed dilatation of the common bile duct (CBD) and intra-hepatic biliary radicles along with a filling defect in the CBD suggestive of sludge or a blood clot. An emergency endoscopic retrograde cholangio-pancreaticogram (ERCP) was performed at this stage. The endoscopic examination showed clotted blood at the ampulla. Cannulation and contrast injection of the CBD showed a dilated CBD (to 12 mm) with a luminal filling defect due to a blood clot (Figure 1). The blood clot was removed using a balloon. An adequate sphincterotomy was successfully performed for further decompression of the biliary system. On follow up, the TB rapidly decreased to 18.1 mg/dL the next day and to 3 mg/dL within 48 h. She was discharged from hospital in good condition. The pleural catheter drained about 500 cc on day 1 and had to be flushed with TPA for adequate drainage. As the catheter was still draining approximately 500 cc/d, she was discharged home with this catheter in place.
On follow up, one week after discharge, the patient was doing well. As the diuretics were not reinstituted after the TIPS, the patient developed significant leg edema. She denied any respiratory or cardiac symptoms. As the chest catheter did not drain any fluid for 2-3 d it was removed by the interventional radiologist. On the clinic visit her bilirubin had normalized to 0.1 mg/dL. After restarting her diuretics (furosemide 40 mg/d and spironolactone 100 mg/d), the leg edema improved and she lost 16 lbs of bodyweight (137 to 121 lbs) over a 2-wk period.
Conjugated hyperbilirubinemia can result due to hepatocellular or biliary disease. Diversion of portal venous blood (about 70% of total hepatic blood supply) to the systemic circulation after TIPS can potentially result in liver dysfunction. This is the basis of hepatic encephalopathy, a common complication after TIPS[1]. However, this is unlikely in our patient for the following reasons: (1) occurrence of liver dysfunction after TIPS is related to pre-TIPS liver function[2]. Our patient with a pre-TIPS model of end-stage liver disease score of 7 was not at risk for post-TIPS liver dysfunction despite reducing the porto-systemic gradient from 16 to 0 mmHg, (2) patients with ischemic hepatocellular liver damage usually have transaminases > 1000 IU/L and our patient had very minimal elevations in liver enzymes, (3) there was no change in mental status which would have been a significant feature in the patient’s presentation if this level of bilirubin was due to hepatocellular dysfunction, and (4) ability to handle and conjugate the increased load of bilirubin by a well compensated liver.
The presence of a blood clot in the CBD on ERCP examination makes biliary disease the likely cause of hyperbilirubinemia. However, bleeding into the bile duct or hemobilia does not explain the clinical picture in the absence of biliary colic and/or gastrointestinal bleeding. Moreover, the hemoglobin remained stable. In addition, a rapid rise in bilirubin (1-18 mg/dL within 48 h and to 22.4 mg/dL within 72 h of the procedure) does not occur with obstruction of the bile ducts including hemobilia. However, this has been described in cases of bilhemia secondary to the development of biliary-venous fistula[3]. It is likely that hyperbilirubinemia in our patient was the result of biliary-venous fistula resulting in bilhemia. Aspiration of bile by the interventional radiologist while trying to puncture the right hepatic vein raises this suspicion further. After the development of a fistula, the direction of flow depends upon the pressures on either side. Normal pressure in the hepatic vein is 0-5 mmHg and in the CBD is 10-12 mmHg, and in the portal system in this case the pressure was 16 mmHg[3]. Therefore, if the pressure in the venous side is higher than in the CBD, this will result in hemobilia and bilhemia will be a major manifestation if the pressure is higher in the CBD. Lack of visualization of the fistula despite an occlusive cholangiogram could either be due to its presence in the small peripheral biliary radicle or to spontaneous closure by the time cholangiogram was performed.
How do we explain the presence of a blood clot in the CBD? We propose that the following sequence of events occurred: Initially the bile duct radicle was inadvertently punctured creating a fistula with one of the small portal venous radicles. This initiated bleeding into the bile duct due to a higher portal pressure initiating hemobilia. However, successful placement of the TIPS decompressed the portal venous system. This favored leakage of bile into the blood causing bilhemia. In fact, the blood clot resulting from the clinically insignificant bleeding exaggerated the biliary pressure, further favoring leakage of bile into the blood.
Although, the term bilhemia was introduced in 1975, the first case was described in 1952[4]. Most cases of bilhemia are reported after hepatic trauma and its occurrence after TIPS is a rare event[5–7]. The patient can be asymptomatic or present with transient hyperbilirubinemia with spontaneous improvement due to closure of the fistula. If the shunt is infected, recurrent cholangitis and bacteremia could dominate the clinical picture[5–7]. To our knowledge, this is the first report of portal vein-biliary fistula causing bilhemia and presenting with rapidly rising bilirubin within 48 h of the TIPS procedure. This condition can be lethal in about 50% of cases, mostly due to fat embolism from a sudden gush of un-dissolved bile into the bloodstream[48]. ERCP is the most useful tool to diagnose this condition as it follows the direction of flow across the fistula[8]. Scintigraphy may be used if endoscopic expertise is unavailable[8].
Treatment of patients with bilhemia should aim to achieve decompression of the biliary system and to reduce the pressure within the CBD. This will allow drainage of bile towards the gut and prevent leakage into the blood. This is best achieved by endoscopic biliary sphincterotomy. In a series of 20 patients with biliary leaks (four with bilhemia), endoscopic sphincterotomy successfully managed all patients but one who died of bile thromboembolism[9]. In the event of a higher location or lack of available technical expertise for ERCP, percutaneous drainage of the biliary system is an alternative[8]. Unfortunately, if the shunt is infected, liver transplantation is the only option to salvage these patients as when the TIPS is placed it can not be removed[57]. In our patient, the presence of a blood clot added to the severity of the problem and its removal and the performance of endoscopic sphincterotomy achieved successful biliary decompression resulting in a positive patient outcome.
In summary, the occurrence of jaundice after TIPS raises the suspicion of a biliary-venous fistula. A high index of suspicion is required for successful management and the prevention of mortality. ERCP with endoscopic sphincterotomy is an effective modality for managing this potentially lethal complication.
| 1. | Boyer TD, Haskal ZJ. The role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Hepatology. 2005;41:386-400. |
| 2. | Alsatie M, Chalasani N, Kwo PY. Management of hepatitis C infection after liver transplantation. Drugs. 2007;67:871-885. |
| 3. | Haberlik A, Cendron M, Sauer H. Biliovenous fistula in children after blunt liver trauma: proposal for a simple surgical treatment. J Pediatr Surg. 1992;27:1203-1206. |
| 4. | Brown CY, Walsh GC. Fatal bile embolism following liver biopsy. Treat Serv Bull. 1952;7:445-450. |
| 5. | Willner IR, El-Sakr R, Werkman RF, Taylor WZ, Riely CA. A fistula from the portal vein to the bile duct: an unusual complication of transjugular intrahepatic portosystemic shunt. Am J Gastroenterol. 1998;93:1952-1955. |
| 6. | Mallery S, Freeman ML, Peine CJ, Miller RP, Stanchfield WR. Biliary-shunt fistula following transjugular intrahepatic portosystemic shunt placement. Gastroenterology. 1996;111:1353-1357. |
| 7. | Jawaid Q, Saeed ZA, Di Bisceglie AM, Brunt EM, Ramrakhiani S, Varma CR, Solomon H. Biliary-venous fistula complicating transjugular intrahepatic portosystemic shunt presenting with recurrent bacteremia, jaundice, anemia and fever. Am J Transplant. 2003;3:1604-1607. |
| 9. | Singh V, Narasimhan KL, Verma GR, Singh G. Endoscopic management of traumatic hepatobiliary injuries. J Gastroenterol Hepatol. 2007;22:1205-1209. |