Published online Jun 14, 2009. doi: 10.3748/wjg.15.2763
Revised: May 8, 2009
Accepted: May 15, 2009
Published online: June 14, 2009
AIM: To investigate the effects of gallbladder stones on motor functions of the gallbladder and the dynamics of bile flow in asymptomatic gallstone disease.
METHODS: Quantitative hepatobiliary scintigraphy was performed to detect the parameters of gallbladder motor function [gallbladder ejection fraction (GBEF), gallbladder visualization time (GBVT), gallbladder time to peak activity (GBTmax), gallbladder half emptying time (GBT1/2), and transit time of bile to duodenum (TTBD)] in 24 patients with asymptomatic cholelithiasis who were diagnosed incidentally during routine abdominal ultrasonographic examination and 20 healthy subjects with normal gallbladder.
RESULTS: Even though there was no significant difference in the clinical and laboratory parameters between the patient and control groups, all parameters of gallbladder function except TTBD were found to differ significantly between the two groups. GBEF in the patient group was decreased (P = 0.000) and GBVT, GBTmax, GBT1/2 in the patient group were longer (P = 0.000, P = 0.015, P = 0.001, respectively).
CONCLUSION: Our results showed that even if there were not any clinical and laboratory findings, gallbladder filling and emptying could be impaired in patients with gallstone disease.
- Citation: Çerçi SS, Özbek FM, Çerçi C, Baykal B, Eroğlu HE, Baykal Z, Yıldız M, Sağlam S, Yeşildağ A. Gallbladder function and dynamics of bile flow in asymptomatic gallstone disease. World J Gastroenterol 2009; 15(22): 2763-2767
- URL: https://www.wjgnet.com/1007-9327/full/v15/i22/2763.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.2763
Asymptomatic cholelithiasis is being diagnosed increasingly, mainly as a result of the widespread use of abdominal ultrasonography for the evaluation of patients for unrelated or vague abdominal complaints and in cases of routine checkup. Most studies have indicated that the progression of asymptomatic to symptomatic disease is relatively low[1–4]. Despite some controversy most authors agree that the vast majority of subjects should be managed by observation alone. The major concern when discussing the natural history of asymptomatic cholelithiasis is the possible development of a severe, potentially life-threatening complication, such as acute supurative cholangitis, severe pancreatitis, cholecystoenteric fistula, gallstone ileus or rarely gallbladder cancer. Unfortunately, it is impossible, using local (such as number, size, nature, alteration in wall thickness or gallbladder contractility) or general factors (such as age, gender, or associated comorbidity) to predict who among asymptomatic patients, will develop symptoms or complications and when[5].
Hepatobiliary scintigraphy is used to show both morphological and physiological changes in the gallbladder. Since physiological changes usually precede morphological alterations by several weeks or months, there is great potential for early diagnosis by scintigraphy, before irreversible functional changes take place[6]. The main advantage of hepatobiliary scintigraphy is that the technique is noninvasive, quantitative, and reproducible and has a low interobserver error rate[7–11].
The current study aimed to investigate by quantitative hepatobiliary scintigraphy the effects of gallbladder stones on motor function of the gallbladder and the dynamics of bile flow in a group of patients with asymptomatic gallstone disease.
The study design was approved by the local University ethical committee and was performed according to the Helsinki Declaration. Informed written consent was obtained from all participating subjects before their involvement in the study.
The study was conducted from April 2006 to February 2008, and included 25 patients with asymptomatic cholelithiasis who had been diagnosed incidentally during routine abdominal ultrasonography. There were no gallstone-related symptoms, such as history of biliary pain (pain in the epigastrium or right upper abdominal quadrant that may radiate to the patient’s back or to the right scapula) or gallstone related complications such as acute cholecystitis, cholangitis, or pancreatitis. The only one patient with nonvisualized gallbladder during hepatobiliary scintigraphy was excluded. Twenty-four patients, (10 male and 14 female; aged 54.66 ± 12.59 years) with asymptomatic gallbladder stones, and 20 control cases (12 male, 8 female; aged 50.30 ± 4.15 years) with normal gallbladder were enrolled in the study. None of the subjects had diabetes mellitus, or a history of disease or operation that affected gallbladder motility. None of the patients had received recent medication such as cholic acid, morphine, atropine, calcium channel blockers, octreotide, progesterone, indomethacin, theophyline, benzodiazepines, and histamine-2 receptor antagonists to influence gallbladder motor function. All patients in the study and control group had normal gallbladder wall thickness (no more than 2 mm), common bile duct upon ultrasound examination and liver function as shown by routine biochemical screening measures [aspartate amino transferase (AST), alanine aminotransferase (ALT), γ-glutamyltransferase (GGT), alkaline phosphatase (ALP) and total bilirubin levels].
After the patients had fasted overnight, hepatobiliary scintigraphy was performed using 185 MBq (5 mCi) of 99m-Tc-mebrofenin (BRIDATEC, GIPHARMA S.r.I., Italy) intravenously. Two-phase dynamic images were taken from the right hypochondrium with the patient in the supine position, using a dual-head gamma camera (Siemens E-CAM, Illinois, USA) which included a low-energy high resolution collimator. Phase 1: 2 s × 60 frames (perfusion phase); phase 2: 60 s × 118 frames (hepatobiliary phase). In the mid-term of the second phase, a standard fatty meal (100 g milk chocolate) instead of cholecystokinin was given to the patients in order to stimulate gallbladder contraction. All of the dynamic images were evaluated with the raw data and cine projections from the computer.
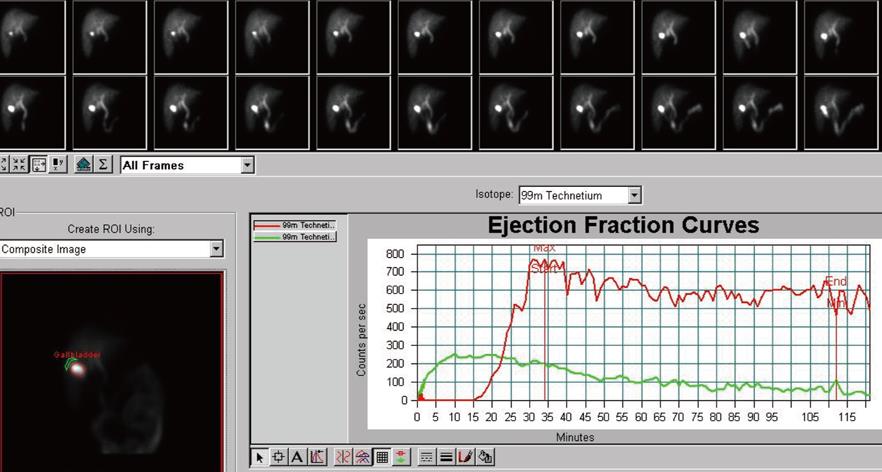
We obtained the following parameters. (1) Gallbladder ejection fraction (GBEF) was calculated by determining count variation in the gallbladder during the filling and emptying period, using a computer program for GBEF. An E-CAM Siemens computer program calculated GBEF according to the time variation curves of these two phase (Figure 1). (2) Gallbladder visualization time (GBVT). (3) Gallbladder time to peak activity (GBTmax). (4) Gallbladder half emptying time (GBT1/2). (5) Transit time of bile to duodenum (TTBD) were evaluated.
The statistical analyses were done using SPSS 13 for Windows (Chicago, IL, USA). The data of the groups were given as mean ± SD and the Mann-Whitney U test was used as a non-parametric test to compare the means between the groups. P < 0.05 was considered as significant.
Table 1 shows the clinical and laboratory features of the patient and control groups (mean ± SD). There was no statistically difference in the clinical and laboratory parameters between the patient and control group (P > 0.05).
| Patients (n = 24) | Controls (n = 20) | P | |
| Number (M/F) | 24 (10/14) | 20 (12/8) | 0.345 |
| Age (yr) | 54.66 ± 12.59 | 50.30 ± 4.15 | 0.267 |
| AST (U/L) | 30.62 ± 13.89 | 27.30 ± 9.99 | 0.547 |
| ALT (U/L) | 34.66 ± 27.86 | 21.60 ± 5.71 | 0.283 |
| GGT (U/L) | 48.20 ± 26.63 | 43.65 ± 10.80 | 0.915 |
| ALP (U/L) | 86.20 ± 23.68 | 86.10 ± 24.03 | 0.972 |
| Total bilirubin (mg/dL) | 0.74 ± 0.28 | 0.69 ± 0.27 | 0.579 |
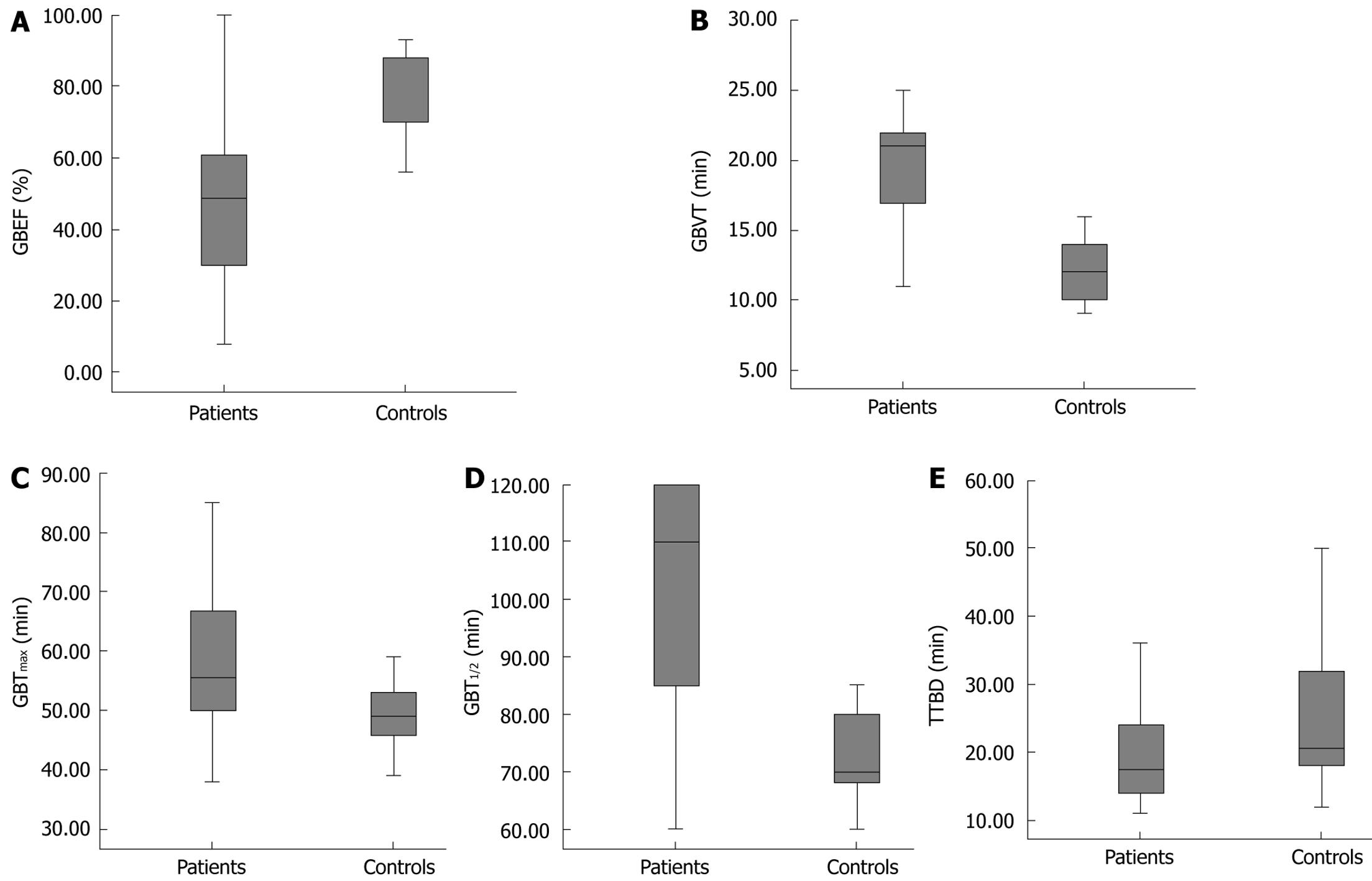
GBEF, GBVT, GBTmax, GBT1/2, and TTBD of the patient and control groups are shown in Figure 2A-E. Mean GBEF in the patient group decreased when compared with that in the control group (49.79 ± 25.42 min vs 78.20 ± 11.23 min; P = 0.000). Mean GBVT (21.83 ± 8.51 min vs 12.20 ± 2.28 min; P = 0.000), GBTmax (59.41 ± 15.09 min vs 49.30 ± 6.74 min P = 0.015), GBT1/2 (99.37 ± 22.95 min vs 74.40 ± 11.12 min P = 0.001) were longer in the patient group than in the control group. There was no significant difference in mean TTBD (22.58 ± 14.08 min vs 27.00 ± 15.36 min) between the two groups.
In the past, the majority of the literature has focused on the pathogenesis of gallstone formation rather than on the association of gallbladder motility and clinical symptoms[12]. Gallbladder stones may be asymptomatic in a considerable number of patients, and the pathogenesis of symptoms is not understood clearly. Theoretically, gallbladder function may be an important predictor of outcome from either cholecystectomy or watchful waiting, because the symptoms traditionally are believed to arise from gallbladder contraction[13].
Several studies using different techniques and protocols have assessed gallbladder function in gallstone disease[814–16]. In these studies, patients groups were generally taken from symptomatic but uncomplicated patients.
Gallbladder emptying is under the control of neural and hormonal stimulation. For normal bile flow, Oddi sphincter relaxation should synchronize with gallbladder contraction. CCK, as a mediator, is responsible for relaxation of the sphincter of Oddi and gallbladder contraction. After a fatty meal is eaten, the gallbladder empties with active contraction, which is regulated mainly by the release of endogenous CCK, which simultaneously induces Oddi sphincter relaxation, therefore allowing maximal bile outflow from the common bile duct into the duodenum at the time of maximal gallbladder contraction[17].
In this manner, it is important to understand how symptoms occur and what the reason is. It is also important to know that, if we perform cholecystectomy the pathological bile flow will resolve. It is still controversial whether impaired gallbladder emptying/contraction is the cause or the result of bile stones[13].
Quantitative hepatobiliary scintigraphy is a well-established method that can be used in the evaluation of hepatocellular function and patency of the biliary system by tracing the production and flow of bile from the liver through the biliary system into the small intestine[18]. Of the quantitative parameters of hepatobiliary scintigraphy, time variables of the gallbladder (GBVT, GBTmax, GBT1/2, and TTBD) and GBEF are regarded as sensitive parameters for diagnosing gallbladder motor function abnormalities.
In previous scintigraphic studies, GBEF and gallbladder emptying time were found to be different in patients with symptomatic gallbladder stones[141519]. Most of these studies, agreed that, although gallbladder emptying was impaired, filling was unaffected. In our study, emptying time was significantly longer in patients with asymptomatic gallstones and GBEF was significantly reduced.
We found that gallbladder filling time was also prolonged compared with the controls and Kao et al[20] have reported that gallbladder stones may impair gallbladder function, especially the filling fraction. Abnormal gallbladder filling and emptying of bile in the gallbladder can result from mechanical obstruction to bile flow, such as altered cystic duct resistance or abnormal sphincter of Oddi tone, decreased gallbladder contractile force, or increased bile viscosity. Patients with organic obstruction at the cystic duct could not be visualized during hepatobiliary scintigraphy and therefore a patient who had a non-visualized gallbladder was excluded from the present study. Increased resistance to bile flow might occur either at the cystic duct or sphincter of Oddi. In our study, there was no difference in TTBD between the control group and asymptomatic gallstone group, thus increased resistance to bile flow in the sphincter of Oddi was not the cause of prolongation in emptying time. On the other hand, viscosity tends to be higher in gallbladder bile of patients with gallstones[21] and may be another cause abnormal gallbladder emptying or filling, but normal TTBD was probably the indicator of normal bile viscosity in our study group. The most likely explanation for the abnormal gallbladder filling in our patients was increased resistance to bile flow at the cystic duct. Similar to our findings Pitt et al[22] have reported increased cystic duct resistance in rodents with gallstones, but we have not been able to find any human study about cystic duct resistance in patients with gallbladder stones. Jazrawi et al[23] have combined ultrasonography with scintigraphy and have shown that turnover of bile is impaired during the refilling phase in patients with gallstones. Moreover Cicala et al[24] have demonstrated that there is decreased turnover of bile that may contribute to cholesterol crystal precipitation and stone growth, as shown by ultrasonographic measurements of gallbladder volume variation. From another point of view, in the patient group, abnormal gallbladder smooth muscle contraction was probably the cause of both impaired emptying time and reduced GBEF.
It is also known that, in patients with impaired emptying, the contractile defect may have developed at a very early stage of gallstone formation[25]. Furthermore, the symptoms in gallstone patients are believed traditionally to arise from gallbladder spasm and normal gallbladder contractility is thought to be a prerequisite for the development of symptoms[12]. The gallbladder motility defect is restricted apparently to asymptomatic patients and appears to protect from symptomatic disease[26].
In conclusion, our results showed that even if there were not any clinical and laboratory findings, gallbladder filling and emptying can be impaired in gallstone patients.
Asymptomatic cholelithiasis is being increasingly, diagnosed today, mainly as a result of the widespread use of abdominal ultrasonography. Hepatobiliary scintigraphy is a noninvasive, quantitative, and reproducible technique that can be used to show morphological and physiological changes in the gallbladder. The authors investigated by hepatobiliary scintigraphy the effects of gallbladder stones on motor function of the gallbladder and the dynamics of bile flow in asymptomatic gallstone disease.
Cholelithiasis is a very common disease, and it is still controversial whether impaired gallbladder emptying/contraction are the cause or result of bile stones. Gallbladder stones may be asymptomatic in a considerable number of patients with gallstones, and the pathogenesis of symptoms is not understood clearly. In previous scintigraphic studies, motor function parameters of the gallbladder have been found to be different in patients with symptomatic gallbladder stones, however, no definitive data have been published in asymptomatic cholelithiasis.
The authors showed for the first time that, even in the absence of any clinical and laboratory findings, gallbladder motor functions such as filling and emptying time and ejection fraction, were impaired in asymptomatic gallstone patients.
Their study was designed to analyze the scintigraphic parameters of gallbladder motor function (gallbladder ejection fraction, gallbladder visualization time, gallbladder time to peak activity, gallbladder half emptying time, and transit time of bile to duodenum) in patients with asymptomatic cholelithiasis who had been diagnosed incidentally during routine abdominal ultrasonography.
99m-Tc-mebrofenin is a radiopharmaceutical agent for hepatobiliary scintigraphy, Gallbladder ejection fraction describes gallbladder emptying function.
This is a very interesting study. This paper reports on the results of an investigation aimed at assessing the effects of gallbladder stones on gallbladder motility and at assessing the dynamics of bile flow in asymptomatic gallstone disease patients. The authors report that, even in the absence of any clinical and laboratory findings, gallbladder filling and emptying can be impaired in this subgroup of gallstone patients.
| 1. | Gracie WA, Ransohoff DR. The silent stone requiescat in pace. Controversies in surgery II. Philadelphia: Saunders 1983; 361-370. [Cited in This Article: ] |
| 2. | McSherry CK, Glenn F. The incidence and causes of death following surgery for nonmalignant biliary tract disease. Ann Surg. 1980;191:271-275. [Cited in This Article: ] |
| 3. | Ransohoff DF, Gracie WA, Wolfenson LB, Neuhauser D. Prophylactic cholecystectomy or expectant management for silent gallstones. A decision analysis to assess survival. Ann Intern Med. 1983;99:199-204. [Cited in This Article: ] |
| 4. | Thistle JL, Cleary PA, Lachin JM, Tyor MP, Hersh T. The natural history of cholelithiasis: the National Cooperative Gallstone Study. Ann Intern Med. 1984;101:171-175. [Cited in This Article: ] |
| 5. | Meshikhes AW. Asymptomatic gallstones in the laparoscopic era. J R Coll Surg Edinb. 2002;47:742-748. [Cited in This Article: ] |
| 6. | Yaylali OT, Yilmaz M, Kiraç FS, Değirmencioğlu S, Akbulut M. Scintigraphic evaluation of gallbladder motor functions in H pylori positive and negative patients in the stomach with dyspepsia. World J Gastroenterol. 2008;14:1406-1410. [Cited in This Article: ] |
| 7. | Krishnamurthy S, Krishnamurthy GT. Gallbladder ejection fraction: a decade of progress and future promise. J Nucl Med. 1992;33:542-544. [Cited in This Article: ] |
| 8. | Krishnamurthy GT, Bobba VR, McConnell D, Turner F, Mesgarzadeh M, Kingston E. Quantitative biliary dynamics: introduction of a new noninvasive scintigraphic technique. J Nucl Med. 1983;24:217-223. [Cited in This Article: ] |
| 9. | Jazrawi RP. Review article: measurement of gall-bladder motor function in health and disease. Aliment Pharmacol Ther. 2000;14 Suppl 2:27-31. [Cited in This Article: ] |
| 10. | Shaffer EA. Review article: control of gall-bladder motor function. Aliment Pharmacol Ther. 2000;14 Suppl 2:2-8. [Cited in This Article: ] |
| 11. | Ryan J, Cooper M, Loberg M, Harvey E, Sikorski S. Technetium-99m-labeled n-(2,6-dimethylphenylcar-bamoylmethyl) iminodiacetic acid (tc-99m HIDA): a new radiopharmaceutical for hepatobiliary imaging studies. J Nucl Med. 1977;18:997-1004. [Cited in This Article: ] |
| 12. | Chan DC, Chang TM, Chen CJ, Chen TW, Yu JC, Liu YC. Gallbladder contractility and volume characteristics in gallstone dyspepsia. World J Gastroenterol. 2004;10:721-724. [Cited in This Article: ] |
| 13. | Larsen TK, Qvist N. The influence of gallbladder function on the symptomatology in gallstone patients, and the outcome after cholecystectomy or expectancy. Dig Dis Sci. 2007;52:760-763. [Cited in This Article: ] |
| 14. | Fisher RS, Stelzer F, Rock E, Malmud LS. Abnormal gallbladder emptying in patients with gallstones. Dig Dis Sci. 1982;27:1019-1024. [Cited in This Article: ] |
| 15. | Northfield TC, Kupfer RM, Maudgal DP, Zentler-Munro PL, Meller ST, Garvie NW, McCready R. Gall-bladder sensitivity to cholecystokinin in patients with gall stones. Br Med J. 1980;280:143-144. [Cited in This Article: ] |
| 16. | Zhu J, Han TQ, Chen S, Jiang Y, Zhang SD. Gallbladder motor function, plasma cholecystokinin and cholecystokinin receptor of gallbladder in cholesterol stone patients. World J Gastroenterol. 2005;11:1685-1689. [Cited in This Article: ] |
| 17. | Funch-Jensen P, Ebbehøj N. Sphincter of Oddi motility. Scand J Gastroenterol Suppl. 1996;216:46-51. [Cited in This Article: ] |
| 18. | Balon HR, Fink-Bennett DM, Brill DR, Fig LM, Freitas JE, Krishnamurthy GT, Klingensmith WC 3rd, Royal HD. Procedure guideline for hepatobiliary scintigraphy. Society of Nuclear Medicine. J Nucl Med. 1997;38:1654-1657. [Cited in This Article: ] |
| 19. | Pomeranz IS, Shaffer EA. Abnormal gallbladder emptying in a subgroup of patients with gallstones. Gastroenterology. 1985;88:787-791. [Cited in This Article: ] |
| 20. | Kao CH, Wang SJ, Chen GH, Yeh SH. Evaluation of gallbladder function by quantitative radionuclide cholescintigraphy in patients with gallbladder sludge or stones. Nucl Med Commun. 1994;15:742-745. [Cited in This Article: ] |
| 21. | Bouchier IA, Cooperband SR, el-Kodsi BM. Mucous substances and viscosity of normal and pathological human bile. Gastroenterology. 1965;49:343-353. [Cited in This Article: ] |
| 22. | Pitt HA, Roslyn JJ, Kuchenbecker SL, Doty JE, Denbesten L. The role of cystic duct resistance in the pathogenesis of cholesterol gallstones. J Surg Res. 1981;30:508-514. [Cited in This Article: ] |
| 23. | Jazrawi RP, Pazzi P, Petroni ML, Prandini N, Paul C, Adam JA, Gullini S, Northfield TC. Postprandial gallbladder motor function: refilling and turnover of bile in health and in cholelithiasis. Gastroenterology. 1995;109:582-591. [Cited in This Article: ] |
| 24. | Cicala M, Guarino MP, Vavassori P, Alloni R, Emerenziani S, Arullani A, Pallone F. Ultrasonographic assessment of gallbladder bile exchanges in healthy subjects and in gallstone patients. Ultrasound Med Biol. 2001;27:1445-1450. [Cited in This Article: ] |
| 25. | Fridhandler TM, Davison JS, Shaffer EA. Defective gallbladder contractility in the ground squirrel and prairie dog during the early stages of cholesterol gallstone formation. Gastroenterology. 1983;85:830-836. [Cited in This Article: ] |
| 26. | Brand B, Lerche L, Stange EF. Symptomatic or asymptomatic gallstone disease: is the gallbladder motility the clue? Hepatogastroenterology. 2002;49:1208-1212. [Cited in This Article: ] |