Published online Jan 7, 2008. doi: 10.3748/wjg.14.143
Revised: September 23, 2007
Published online: January 7, 2008
The authors describe a rare case in which blunt abdominal trauma resulted in mesenteric injury with delayed double ischemic ileal stenosis. Abdominal computed tomography demonstrated stenotic ileal loop with mural thickening. At surgery, a double stenotic bowel loop was found adjacent to a healed defect in the mesentery. Histological examination of the two resected segments showed fibrotic and ischemic lesions within the mesentery. Ischemic intestinal stenosis from mesenteric injury should be considered in the differential diagnosis in patients suffering from intestinal occlusion with a history of blunt abdominal trauma.
- Citation: Bougard V, Avisse C, Patey M, Germain D, Levy-Chazal N, Delattre JF. Double ischemic ileal stenosis secondary to mesenteric injury after blunt abdominal trauma. World J Gastroenterol 2008; 14(1): 143-145
- URL: https://www.wjgnet.com/1007-9327/full/v14/i1/143.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.143
In the current treatment of blunt abdominal trauma, conservative management and observation with computed tomography (CT) have become the standard of care for the non-life threatening abdominal lesions. Ischemic intestinal stenosis has been described as a delayed rare complication of mesenteric blunt abdominal trauma. The authors present herein a case of post-traumatic mesenteric injury proved by histological examination, and with double bowel stenosis on CT scan and enteroclysis.
A 35-year-old female was admitted after an automobile accident with sudden deceleration. She drove the car and carried the safety belt. The admission check-up showed a cranial trauma and multiple fractures, in particular of the two inferior limbs. She underwent contrast enhanced abdominal CT which showed moderate fluid in the peritoneal cavity attributed to recent bleeding, but no free air, and no parenchymatous, visceral or vascular lesions. She was transferred to the traumatologic unit for surgical osteosynthesis, after which she underwent revalidation treatment.
Six weeks later, she returned to the emergency department with abdominal pain. Altogether, she suffered from four painful abdominal crises with vomiting, described as acute, periumbilical cramps, spontaneously resoluting, compatible with subocclusion or König syndrome.
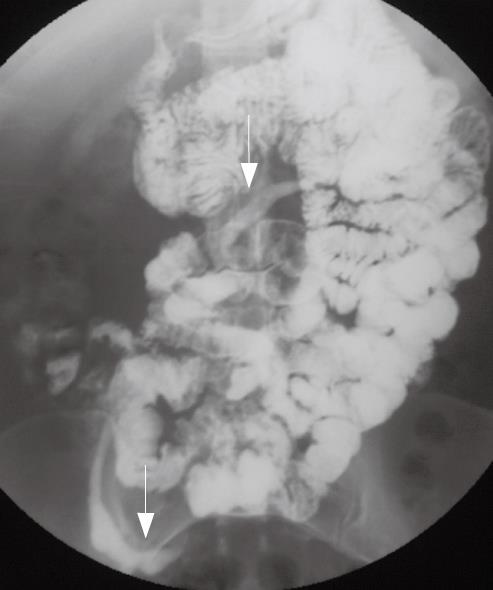
Abdominal CT showed two ileal loops with a thickened wall and narrowed lumen (Figure 1) adjacent to a mesenteric haziness and minimal fluid in the Douglas. There was no sign of absolute obstruction. An enteroclysis confirmed two intestinal stenosis with rigid ileal loops, one proximal and the other distal (Figure 2).
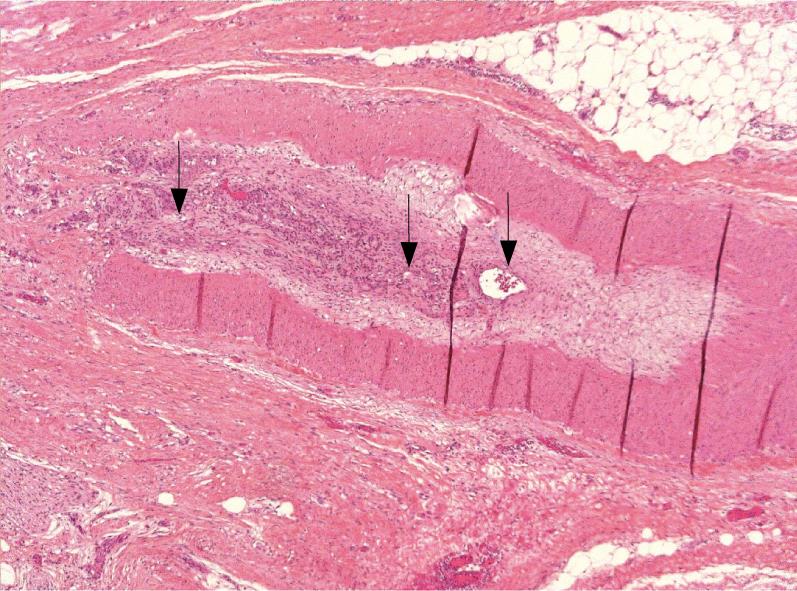
The patient underwent laparotomy. Two ileal lesions were observed, one located at 180 cm from Treitz’s angle, the second one at 60 cm from the Bauhin’s valve. Both were scarred ischemic post-traumatic lesions located in front of a mesenteric injury, with thickened ileal wall and narrowed lumen (Figure 3). The two stenosed ileal segments were resected and a latero-lateral anastomosis was performed. Recovery was uneventful. Pathological examination showed mucosal ulceration of the gut located in front of a mesenteric tear (Figure 4), and degenerative infiltration of the mesenteric small vessels, arterioles and veins (Figure 5).
Some patients with traumatic intestinal lesion such as perforation or hemorrhage from disruption of mesenteric vessels or parenchymatous tears require immediate surgical intervention. Small and large bowel mesenteric injuries are found in approximately 13.5 % of all patients undergoing laparotomy after blunt abdominal trauma[12]. In this setting, small bowel injuries are more frequent than colonic injuries, probably due to the factors, including location and lack of redundancy, which prevents formation of closed loops[3]. Contrast enhanced CT should be performed early in patients with blunt abdominal trauma because most significant bowel and mesenteric injuries, as well as associated injuries to other abdominal viscera, may be reliably identified. The presence of a moderate to large volume of intra-peritoneal fluid without visible solid organ injury can be an important sign of mesenteric or bowel injury[1], similar to this patient.
On the other hand, mesenteric injury may not cause clinical manifestations[4]. Patients with blunt abdominal trauma are often managed without surgical intervention if there is no sign of bowel perforation or hypovolemic shock. As a result, mesenteric injuries might remain undiagnosed after blunt abdominal trauma.
Small bowel obstruction following blunt abdominal trauma is rare. Three possible causes have been suggested: small bowel perforation[5], localized bowel ischemia[14] and mesenteric injury[6]. Mesenteric vascular injury may induce chronic ischemia of the corresponding segment of small bowel, inducing secondary thickening of the bowel wall and intestinal occlusion[16]. Post-traumatic bowel lesions may also be found in the colon, mainly on the left side, specifically the sigmoid colon[7]. The case described herein and its pathological report, further support the mesenteric injury theory of post-traumatic bowel strictures. Most published reports of post-traumatic bowel stenosis described one stricture of the small bowel[8]. The patient reported herein suffered from a double localisation of small bowel lesions, both treated by resection and anastomosis.
Under this particular circumstance, enteroclysis may demonstrate the localization of the stricture, showing a narrowed, rigid loop[910]. Abdominal CT may show a bowel wall thickening and a concentric narrowed intestinal lumen, or signs of small bowel obstruction with changed calibre of loops[1]. Although angiography may further demonstrate mesenteric vessel occlusion and provide additional information concerning mesenteric injury[911], the authors consider that abdominal CT may provide sufficient information to confirm the clinical suspicion of post-traumatic small bowel stricture and to indicate the need for surgical exploration. Laparotomy with resection of the stenosed segment and primary anastomosis is the appropriate treatment. Early recognition and intervention may prevent prolonged morbidity[1012].
In summary, a rare case of intestinal occlusion secondary to double small bowel stricture due to abdominal blunt trauma and mesenteric injury was described. This diagnosis should be considered in all patients presenting with abdominal pain some weeks after blunt abdominal trauma.
| 1. | De Backer AI, De Schepper AM, Vaneerdeweg W, Pelckmans P. Intestinal stenosis from mesenteric injury after blunt abdominal trauma. Eur Radiol. 1999;9:1429-1431. [Cited in This Article: ] |
| 3. | Dauterive AH, Flancbaum L, Cox EF. Blunt intestinal trauma. A modern-day review. Ann Surg. 1985;201:198-203. [Cited in This Article: ] |
| 4. | Marks CG, Nolan DJ, Piris J, Webster CU. Small bowel strictures after blunt abdominal trauma. Br J Surg. 1979;66:663-664. [Cited in This Article: ] |
| 5. | Welch GH, Anderson JR. Small bowel stricture following abdominal trauma. Postgrad Med J. 1985;61:1087-1088. [Cited in This Article: ] |
| 6. | Maharaj D, Perry A, Ramdass M, Naraynsingh V. Late small bowel obstruction after blunt abdominal trauma. Postgrad Med J. 2003;79:57-58. [Cited in This Article: ] |
| 7. | Lublin M, Chauvin S, Kashani M, Ibrahim I, Kahn M. Delayed colonic stricture and obstruction after blunt abdominal trauma: a case report and review of the literature. J Trauma. 2004;57:193-195. [Cited in This Article: ] |
| 8. | Hirota C, Iida M, Aoyagi K, Matsumoto T, Yao T, Fujishima M. Posttraumatic intestinal stenosis: clinical and radiographic features in four patients. Radiology. 1995;194:813-815. [Cited in This Article: ] |
| 9. | Tsushima Y, Yamada S, Aoki J, Endo K. Ischaemic ileal stenosis following blunt abdominal trauma and demonstrated by CT. Br J Radiol. 2001;74:277-279. [Cited in This Article: ] |
| 10. | Lane TM, Williams TG. Small bowel obstruction following blunt abdominal trauma. Injury. 1998;29:484-485. [Cited in This Article: ] |
| 11. | Loberant N, Szvalb S, Herskovits M, Cohen I, Salamon V. Posttraumatic intestinal stenosis: radiographic and sonographic appearance. Eur Radiol. 1997;7:524-526. [Cited in This Article: ] |