Copyright
©2007 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 7, 2007; 13(9): 1313-1332
Published online Mar 7, 2007. doi: 10.3748/wjg.v13.i9.1313
Published online Mar 7, 2007. doi: 10.3748/wjg.v13.i9.1313
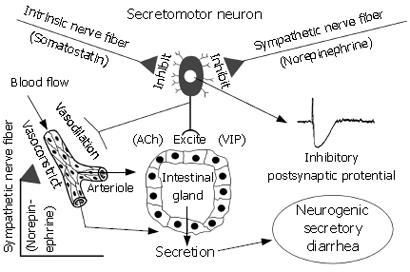
Figure 3 Intestinal secretory glands (i.
e. crypts of Lieberkühn and Brunner’s glands) are innervated by secretomotor neurons in the ENS. Neurotransmitters (e.g. ACh and VIP), which evoke secretion, are released at the neuro-epithelial junctions when secretomotor neurons fire. Axon collaterals to blood vessels simultaneously dilate submucosal vessels to increase blood flow in support of stimulated secretion. Noradrenergic input from the sympathetic nervous system and somatostatinergic input from intrinsic ENS neurons suppress firing of secretomotor neurons and thereby inhibit secretion. Factors that cause hyperactivity of secretomotor neurons enhance secretion and lead to neurogenic secretory diarrhea. In inflammatory states (e.g. ulcerative colitis and Crohn’s disease) the release of inflammatory mediators elevates activity of secretomotor neurons leading to diarrhea. Certain pathogens and enterotoxins (e.g. cholera toxin and Clostridium difficille toxin A) activate secretomotor neurons to produce a diarrheal state. In food allergies, presence of sensitizing food antigens (e.g. shellfish, tree nuts) triggers mast cell degranulation and releases mediators such as histamine, serotonin and prostaglandins, all of which activate secretomotor neurons to evoke diarrhea. When secretomotor neurons are hypoactive, secretion is reduced, the liquidity of the intestinal contents is reduced and a state of constipation can follow. Activating opioid or somatostatinergic receptors (e.g. by opioid analgesics or octreotide) on secretomotor neurons inhibits their excitability and suppresses secretion.
- Citation: Wood JD. Neuropathophysiology of functional gastrointestinal disorders. World J Gastroenterol 2007; 13(9): 1313-1332
- URL: https://www.wjgnet.com/1007-9327/full/v13/i9/1313.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i9.1313