Copyright
©2007 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 7, 2007; 13(9): 1313-1332
Published online Mar 7, 2007. doi: 10.3748/wjg.v13.i9.1313
Published online Mar 7, 2007. doi: 10.3748/wjg.v13.i9.1313
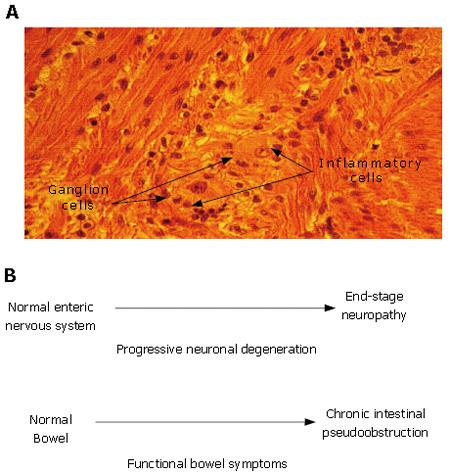
Figure 2 Enteric neuropathy underlies the pathophysiology in a subset of patients with functional gastrointestinal disorders.
A: Idiopathic myenteric ganglionitis. Histology of the myenteric plexus in a full-thickness small intestinal biopsy taken during exploratory laparotomy for intestinal obstruction. A diagnosis of neuropathic pseudoobstruction was made on the basis of neuronal degeneration associated with an inflammatory infiltrate localized to the myenteric plexus. The patient had a multiple year history of complaints suggestive of IBS. Histological section and patient history courtesy of Dr. Claudio Fiocchi, The Cleveland Clinic, Cleveland, Ohio; B: Enteric neuronal degeneration and associated symptoms progress in parallel (e.g. symptoms of IBS). Most individuals start postnatal life with a normal ENS and normally functioning bowel. Neuronal degeneration mediated by autoimmune attack directed to the ENS (e.g. paraneoplastic syndrome, Chagas disease, idiopathic inflammatory neuropathy) can progress to a stage where ENS function is lost. Functional bowel symptoms appear and worsen as neurons are progressively lost from the ENS microcircuits required for integrated function of the whole organ. Chronic intestinal pseudoobstruction of the neuropathic form occurs when the loss of neurons progresses to a stage where the neuronal circuits for propulsive motility are no longer functional.
- Citation: Wood JD. Neuropathophysiology of functional gastrointestinal disorders. World J Gastroenterol 2007; 13(9): 1313-1332
- URL: https://www.wjgnet.com/1007-9327/full/v13/i9/1313.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i9.1313