Published online Jan 21, 2005. doi: 10.3748/wjg.v11.i3.460
Revised: May 2, 2004
Accepted: June 25, 2004
Published online: January 21, 2005
Primary rectal lymphoma is a rare presentation of gastrointestinal lymphomas. Its clinical presentation is indistinguishable from that of rectal carcinoma. Although surgical resection is often technically feasible, optimal therapy for colorectal lymphoma has not yet been identified. We report a case of primary rectal lymphoma (non-Hodgkin’s large cell lymphoma of type B) with high-grade features that disappeared completely after chemo-radiotherapy. This case underlines that primary treatment with systemic chemotherapy and involved-field radiotherapy can be successful for rectal lymphoma, with surgery reserved for complications and chemotherapy failures.
- Citation: Bilsel Y, Balik E, Yamaner S, Bugra D. Clinical and therapeutic considerations of rectal lymphoma: A case report and literature review. World J Gastroenterol 2005; 11(3): 460-461
- URL: https://www.wjgnet.com/1007-9327/full/v11/i3/460.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i3.460
Lymphoma may occur as a primary lesion or as part of a generalized malignant process involving the gastrointestinal tract. The differentiation of these two forms is very important, as both treatment and prognosis are different. Primary gastrointestinal lymphomas have been described as those in which involvement of the alimentary tract predominates or those with symptoms of gastrointestinal involvement on presentation. More strict guidelines include the absence of palpable peripheral lymphadenopathy at the time of presentation; absence of mediastinal adenopathy on a chest radiograph; a normal peripheral blood smear; involvement at laparatomy of only the the esophagus, stomach, bowel or regional lymph nodes (excluding retroperitoneal lymph nodes); and absence of hepatic and splenic involvement except by direct spread of the disease from a contagious focus[1].
Primary gastrointestinal lymphoma accounts for 5% of all lymphomas. Colorectal involvement accounts for 10-20% of the cases in most studies of gastrointestinal tract lymphoma[2-5]. Primary colorectal lymphoma is an uncommon disorder accounting for 0.05% of all colonic neoplasms and 0.1% of primary rectal tumors[6].
Gastrointestinal lymphomas remain the subject of much debate with regard to therapeutic approaches. The role of surgery in primary lymphoma of the rectum is controversial. Keeping these data in mind we decided to describe the recently observed case of a patient affected by primary lymphoma of the rectum to discuss the treatment modalities with a brief review of the literature.
A 33 year-old male, in May 2001, was admitted to a local hospital with complaints of pain in lower abdominal regions, rectal bleeding, diarrhea, and weight loss. Rectoscopy verified a tumor mass in the rectum, but histology of biopsy specimens revealed no specific findings other than chronic inflammatory cells.
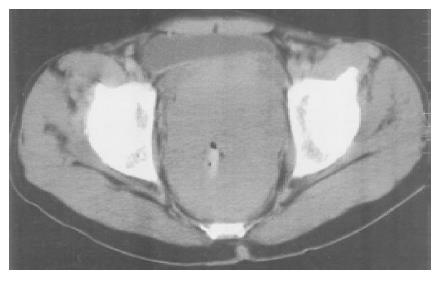
When the patient was transferred to our clinic, he had severe abdominal pain. There was a palpable mass on rectal examination. The mass was smooth, firm to hard, and fixed to the rectal wall. Abdominopelvic CT demonstrated an extensive, bulky rectal tumor (Figure 1). There was no associated intraabdominal adenopathy. A repeat colonoscopy showed enlargement of the lesion. Large biopsy specimens were taken for histological diagnosis. The lesion was diagnosed as non-Hodgkin’s large cell lymphoma of B type, with high-grade features. Results of immunohistochemical staining were CD20 (+), LCA (+), CD5 (-), TdT (-), and cytokeratin (-). KI was more than 90%. As additional investigations did not show any evidence of infiltration to other organs, the disease was staged as clinical stage I rectal lymphoma. However, the lesion was enlarged enormously during an observation period of 10 d. This could suggest that the lesion had a tendency to advance into a more aggressive clinical course.
A transverse loop colostomy was performed to relieve colonic obstruction and pain. After six cycles of modified ProMACE schedule (doxorubicin 30 mg/m2 iv on d 1, cyclophosphamide 600 mg/m2 iv on d 1 and 2, etoposide 120 mg/m2 iv on d 1, 2 and 3, prednisone 50 mg/m2 im on d 1-6, and methotrexate 35 mg/m2 iv on d 7), the lesion completely disappeared. We decided not to resect the rectum. Additionally, the patient was also given an involved-field radiation therapy (4000 cGy in 20 fractions for over 4 wk). A complete remission was achieved and confirmed by abdominal CT scan and colonoscopy with biopsy of the diseased region. Afterwards, the colostomy was closed. There was no recurrence during the 3 years of follow up using endoscopy and biopsy.
Primary lymphoma of the rectum is a rare disorder. These lesions are predominantly non-Hodgkin lymphomas, with colorectal involvement seen in less than 5% of autopsies for Hodgkin disease[6]. Rectal lymphoma usually presents with signs and symptoms suggestive of primary rectal carcinoma. Patient with rectal lymphoma usually seek treatment because of rectal bleeding or an alteration in bowel habits. It has been reported that the majority of patients are symptomatic complaining of abdominal pain, nausea, vomiting, fever, and weight loss[2-6]. Abdominal CT and endoscopy with biopsy are the most useful diagnostic tests. The growth patterns seen in the rectum varied. The growth might be bulky and protuberant with ulceration; it may appear as annular or plaque like thickenings of the bowel wall or manifest as multiple lymphomatous polyposes[7]. The macroscopic appearance bears no relationship to the histologic structure.
When CT revealed a combination of a focally or diffusely infiltrative process of the colon and extensive abdominal and/or pelvic adenopathy, lymphoma should be the primary consideration in the differential diagnosis and must be excluded by endoscopic biopsy. However, if adenopathy was not associated with a primary colorectal lymphoma, it might be difficult radiologically to distinguish this lesion from a primary adenocarcinoma of the colon. This difficulty arises predominantly in the settings of solitary mass lesions. Primary colorectal lymphomas manifested as discrete masses tended to have a greater depth of mural invasion than infiltrative lesions[8].
Colorectal lymphomas commonly cause concentric wall thickening and they often destroy the full thickness of the bowel wall without an associated desmoplastic reaction. Some authors cited a typical wall thickness in colonic lymphoma of 7 to 12 cm from the lumen to the serosa[9].
Two risk factors have been reported to be associated with the development of primary colorectal lymphoma: inflammatory bowel disease and immunosuppression (posttransplant, AIDS, or immune disorder). The aggressive nature of AIDS-related lymphoma could usually result in a disseminated disease at the time of diagnosis[10,11].
Treatment of colorectal lymphomas remains uncertain. Some studies suggested that the primary treatment was to attempt resection when the disease was judged to be resectable because patients with residual diseases had a poor prognosis[12-14]. Given the morbidity following resection of the rectum, the value of surgery for primary lymphoma of the rectum is a subject to be debated.
In some series, radiotherapy or chemotherapy was considered a treatment of choice, because patients with residual diseases after surgery had a poor prognosis, and adjuvant treatment would increase the duration of disease free survival[15,16]. For patients with widespread diseases, those in whom the rectum was secondarily involved, or patients with AIDS, operation would seem inappropriate. These patients may benefit from chemotherapy and radiotherapy.
Radiotherapy alone has not been studied extensively in this disease, although it has been used in a small number of patients usually in combination with cytotoxic chemotherapy. It remains to be seen what role radiotherapy may play in the treatment of this disease.
Diffuse large B cell lymphoma of the large bowel is generally treated with a uniform therapeutic approach: aggressive surgery followed by adjuvant chemotherapy. However, most of the studies included patients with primary gastric or small bowel and large bowel in the same analysis, and also patients at different stages, different histology, and different surgical approaches. Lymphoma of the rectum should be considered as a different clinico-pathological entity with different behaviors, histology and clinical presentation. For this reason, treatment should be defined based on this special clinical condition[17].The therapeutic experience in this selected group of patients is limited, because even in large tertiary referral centers the number of cases is small. The analysis of those retrospective data regarding surgery, radiation therapy, and chemotherapy is also difficult to interpret because of lack of uniformly accepted regimens.
This case showed that a rectal lymphoma could be treated without resection of the rectum. Although it is not possible to make a legitimate conclusion with a single case, with an optimistic approach, we may conclude that the intensity and preferred modality of optimal therapy for rectal lymphoma should be determined by the clinical stage of the disease. Patients with a high tumor bulk, a low-grade histology, and no evidence of local or distant metastasis can be managed by combined chemo-radiotherapy, reserving surgery only for complications and chemotherapy failures.
Assistant Editor Guo SY Edited by Wang XL
| 1. | Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961;49:80-89. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 525] [Cited by in F6Publishing: 459] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 2. | Kashimura A, Murakami T. Malignant lymphoma of large intestine --15-year experience and review of literature. Gastroenterol Jpn. 1976;11:141-147. [PubMed] [Cited in This Article: ] |
| 3. | Lewin KJ, Ranchod M, Dorfman RF. Lymphomas of the gastrointestinal tract: a study of 117 cases presenting with gastrointestinal disease. Cancer. 1978;42:693-707. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |
| 4. | Dragosics B, Bauer P, Radaszkiewicz T. Primary gastrointestinal non-Hodgkin's lymphomas. A retrospective clinicopathologic study of 150 cases. Cancer. 1985;55:1060-1073. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 5. | Henry CA, Berry RE. Primary lymphoma of the large intestine. Am Surg. 1988;54:262-266. [PubMed] [Cited in This Article: ] |
| 6. | Dodd GD. Lymphoma of the hollow abdominal viscera. Radiol Clin North Am. 1990;28:771-783. [PubMed] [Cited in This Article: ] |
| 7. | Ohri SK, Keane PF, Sackier JM, Hutton K, Wood CB. Primary rectal lymphoma and malignant lymphomatous polyposis. Two cases illustrating current methods in diagnosis and management. Dis Colon Rectum. 1989;32:1071-1074. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Wyatt SH, Fishman EK, Hruban RH, Siegelman SS. CT of primary colonic lymphoma. Clin Imaging. 1994;18:131-141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Megibow AJ, Balthazar EJ, Naidich DP, Bosniak MA. Computed tomography of gastrointestinal lymphoma. AJR Am J Roentgenol. 1983;141:541-547. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 58] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Bartolo D, Goepel JR, Parsons MA. Rectal malignant lymphoma in chronic ulcerative colitis. Gut. 1982;23:164-168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Fan CW, Chen JS, Wang JY, Fan HA. Perforated rectal lymphoma in a renal transplant recipient: report of a case. Dis Colon Rectum. 1997;40:1258-1260. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Jinnai D, Iwasa Z, Watanuki T. Malignant lymphoma of the large intestine--operative results in Japan. Jpn J Surg. 1983;13:331-336. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 60] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Zighelboim J, Larson MV. Primary colonic lymphoma. Clinical presentation, histopathologic features, and outcome with combination chemotherapy. J Clin Gastroenterol. 1994;18:291-297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 45] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Fan CW, Changchien CR, Wang JY, Chen JS, Hsu KC, Tang R, Chiang JM. Primary colorectal lymphoma. Dis Colon Rectum. 2000;43:1277-1282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 72] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Bellesi G, Alterini R, Messori A, Bosi A, Bernardi F, di Lollo S, Ferrini PR. Combined surgery and chemotherapy for the treatment of primary gastrointestinal intermediate- or high-grade non-Hodgkin's lymphomas. Br J Cancer. 1989;60:244-248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 43] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Rackner VL, Thirlby RC, Ryan JA. Role of surgery in multimodality therapy for gastrointestinal lymphoma. Am J Surg. 1991;161:570-575. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 64] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Avilés A, Neri N, Huerta-Guzmán J. Large bowel lymphoma: an analysis of prognostic factors and therapy in 53 patients. J Surg Oncol. 2002;80:111-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |