Published online May 14, 2005. doi: 10.3748/wjg.v11.i18.2691
Revised: April 29, 2004
Accepted: July 22, 2004
Published online: May 14, 2005
Human colonic motility is a relatively difficult topic to investigate. However, the refinement of manometric techniques in recent years enabled us to study both the proximal and distal segments of the viscus. The present paper reviews our knowledge about normal aspects of colorectal motility in man and the abnormalities found in slow transit constipation (STC), one of the most frequent and difficult to treat subtypes of constipation. An internet-based search strategy of the Medline and Science Citation Index was performed using the keywords colon, colonic, colorectal, constipation, slow transit, motility, rectal, rectum in various combinations with the Boolean operators AND, OR and NOT. Only articles related to human studies were used, and manual cross-referencing was also performed. Most of colonic motor activity is represented by single nonpropagated contractions, rarely organized in bursts; this activity is maximal during the day, especially after waking and following meals. In addition, a specialized propagated activity with propulsive features is detectable, represented by high- and low-amplitude propagated contractions. In the severe form of constipation represented by the slow transit type, the above motor activity is completely deranged. In fact, both basal segmental activity (especially in response to meals) and propagated activity (especially that of high amplitude) are usually decreased, and this may represent a physiologic marker of this disorder. Human colonic motor activity is quite a complex issue, still only partly understood and investigated, due to anatomic and physiological difficulties. In recent years, however, some more data have been obtained, even in proximal segments. These data have helped in elucidating, although only in part, some pathophysiological mechanisms of chronic constipation, and especially of the STC subtype.
- Citation: Bassotti G, Roberto G, Castellani D, Sediari L, Morelli A. Normal aspects of colorectal motility and abnormalities in slow transit constipation. World J Gastroenterol 2005; 11(18): 2691-2696
- URL: https://www.wjgnet.com/1007-9327/full/v11/i18/2691.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i18.2691
The main physiological properties of the human colon (absorption, propulsion of contents, storage and expulsion of feces) require unique motor activities, different from those of the upper gut[1], apt to propel distally intraluminal contents, to mix them in a continuous manner, and to store and eventually expel the residuals[2]. Since colonic contents, unlike those in the upper gut, employ hours or days to pass through the viscus, prolonged observations (24 h or more) are needed to assess the various aspects of colonic motility[3].
Several techniques have been proposed to evaluate the motor behavior of the large bowel for prolonged periods of time[4-6], the more diffuse being colonic manometry as both a research and (especially in the pediatric area) diagnostic tool[7,8]. The more frequently employed technique consists of positioning a manometric catheter within the colon by the aid of a colonoscope; the catheter is then connected to a recording apparatus to detect intraluminal pressures throughout the day, and to evaluate the effects of meals, sleep, awakening, etc.[9]. More recently, the classic water-perfused catheters were compared to solid state ones[10] that allow prolonged ambulatory recordings of colonic motility[11,12] and even an automated computer analysis of recordings[13].
An internet-based search strategy of the Medline and Science Citation Index was performed using the keywords colon, colonic, colorectal, constipation, slow transit, motility, rectal, rectum in various combinations with the Boolean operators AND, OR and NOT. Only articles related to human studies were used, and manual cross-referencing was also performed. Articles published in English between January 1965 and March 2004 were selected; however, a search in non-English languages and in journals published before 1965 was also performed in our library. Letters and abstracts were quoted only when the full papers were not available.
Manometric investigations have shown that colonic motility may be grossly classified into two main types, and that these mostly agree with previous radiological observations[14]. We have recently proposed a simple classification of colonic contractile patterns, based on our experience with 24-h recor-dings in healthy humans[9,15]. Colonic motility may therefore be divided into segmental activity (single contractions; bursts of contractions: rhythmic, arrhythmic) and propagated activity (low-amplitude propagated contractions (LAPC); high-amplitude propagated contractions (HAPC)).
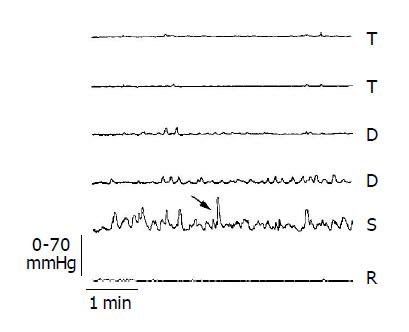
This kind of contractile activity constitutes mostly of the overall colonic motility, and it is usually represented by waves with amplitude ranging from 5 to 50 mmHg; occasionally, contractions of higher amplitude may be observed (Figure 1). Segmental contractions may appear singly or grouped (bursts); although the bursts appear usually as an arrhythmic array of waves, in a small percentage of time (<6% of the overall contractile daily activity) they may assume a rhythmic frequency. This rhythmic frequency is mostly comprised in the 3 cycle/min range, and it is preferentially observed in the distal (descending and sigmoid colon)[16]. The purpose of the segmental contractile activity is to propel distally the fecal matter by means of an aborally directed pressure gradient that moves slowly the contents toward the rectum[17,18]. This activity also allows an optimal absorption of water, electrolytes, short-chain fatty acids, and bacterial metabolites.
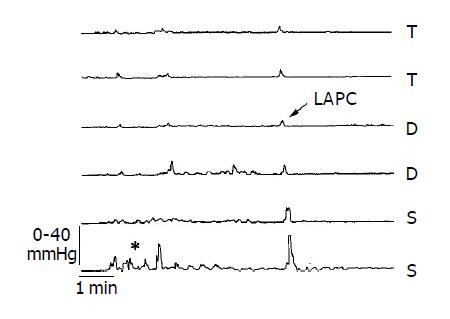
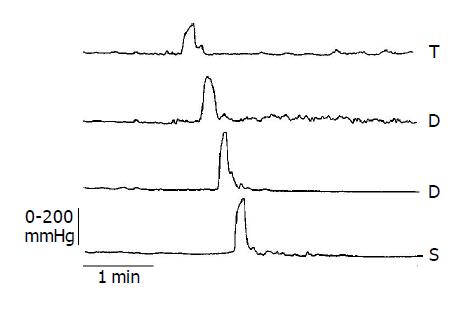
To date, objective criteria (also employing automated analysis) to distinguish the various types of propagated contractions do not exist[19]. We have classified the propagated events, on the basis of their amplitude, as LAPC and HAPC. The former (Figure 2) that feature an amplitude of less than 50 mmHg and are relatively frequent (on average, more than 100 events/d) have a probable main function of transporting fluid contents within the colon[20,21]; LAPC have also been associated with distension of the viscus[22] and passage of flatus[23]. The other kind of propagated activity, represented by contractions averaging more than 100 mmHg amplitude (Figure 3) and occurring infrequently (on average, about 6 events/d), was firstly described in man by radiologists at the beginning of the last century[24], and was subsequently demonstrated to correspond to the radiological concept of “mass movements”, able to shift large quantities of contents for a long tract within the colon[25,26]. More recently, HAPC have been better characterized by manometric means[27,28], and their important role in the defec-atory mechanisms established. These powerful contractions, in fact, are strongly associated with the defecation itself, and precede the expulsion of stools, so that they are considered one of the driving events of this important physiologic act[29,30].
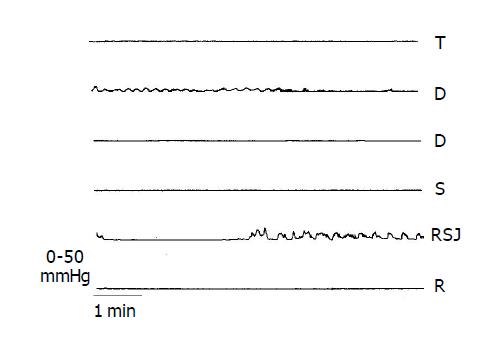
Unlike the upper gut, the human colon seems not to be organized in accordance to regular motor patterns that follow a cyclic timing. However, in recent years periodic motor phenomena have been documented in the rectum (“rectal motor complex”, RMC)[31] and in the more distal colonic segments (“periodic colonic motor activity”) (Figure 4)[32]. The physiological significance of these phenomena is still under investigation, although for the RMC a continence-preserving mechanism (especially when sleeping) has been hypothesized[33]. No cyclic or periodic motor activity has been documented in the anal canal[34].
More information is available concerning the fluctuations of colonic motor activity around-the-clock: in fact, prolonged manometric and electromyographic recordings have convincingly shown that a circadian trend is recognizable, with a maximum of activity during the daylight hours, after awakening in the morning, and after meals[4,5]. Conversely, sleep causes a profound inhibition of colonic motility, and seems to represent a major determinant of its diurnal variations[35,36]. These variations in colonic motility are paralleled by a similar trend that may be observed in the tonic activity of the viscus’ wall when measured by means of a barostat[37].
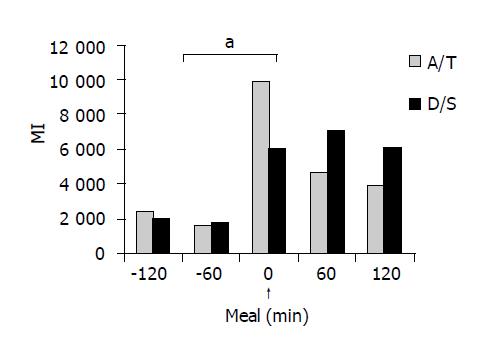
The ingestion of food is a major physiological stimulus for colonic motor activity[38], and it is represented by an increase (of at least 2-h duration) in the overall motility following the first mouthful of food (Figure 5)[39]; this response, mostly represented by segmental contractions, is also accompanied by an increased smooth muscle tone[40]. The colonic motor response to eating is driven by a dual component, cerebral and gastric, in that it may be evoked by both sham feeding and gastric distension[41]. Meal composition influences colonic motor response: in fact, although carbohydrate meals are able to elicit motor activity, the effects are short lived when compared with fat meals[42].
Constipation is a frequent clinical symptom, and its diagnostic criteria have been recently revised in the Rome II classification[43] as the presence in the last year, for at least 12 wk (which need not to be consecutive) and in more than ¼ of defecations, of two or more of the following: straining, lumpy or hard stools, sensation of incomplete evacuation, sensation of anorectal obstruction/blockade, manual maneuvers (digital evacuation, support of the pelvic floor, etc.) to facilitate defecation, and/or less than three defecations per week. Loose stool are not present and there are insufficient criteria for irritable bowel syndrome.
Two major pathophysiologic subtypes of constipation may be identified, with a third being the coexistence of both in the same patient[44]. The most frequent subtype is represented by the pelvic floor dysfunction (also known as “outlet obstruction”, “obstructed defecation”, “dyschezia”, “anismus”, “pelvic floor dyssynergia”), which features normal or slightly slowed colonic transit with residual storage in the rectum or rectosigmoid area[45]. The main pathophysiologic mechanism is due to an inability to evacuate adequately contents from the rectum, and it will not be discussed further, since it has been recently reviewed extensively elsewhere[46]. The other subtype of constipation is the so-called slow transit constipation (STC), a clinical syndrome usually affecting women and characterized by often intractable constipation and heavily delayed colonic transit[47]; this condition is usually attributed to disordered colonic motor function[48]. In the last years, STC had been the subject of several investigations, aimed at evaluating the motility abnormalities of the large bowel as responsible for the patients’ complaints. These pathophysiological aspects of STC will be discussed below. We feel that many of the available data are quite significant because (and differently than those available for other subtypes of constipation or other functional diseases of the large bowel) they have often been obtained in relatively homogenous cohorts of patients.
Although the etiology of STC remains elusive, there is ample evidence that motility of the large bowel is profoundly deranged in this condition, and this derangement may be observed for almost all the physiologic variables described above.
Most of the few studies available were limited to the anorectal-sigmoid area (thereby justifying in part the heterogeneity of findings). These studies showed either overall reduced rectosigmoid motility[49] and impaired response to intrarectal bisacodyl[50], or normal or increased rectosigmoid motor activity[51]. More recently, investigations on more proximal segments of the colon have demonstrated that in these patients the segmental contractile response to cholinergic stimulation is heavily impaired[52] and that the regular contractile frequency activity is reduced to about half (i.e., <3%) of that recorded in normal subjects[53].
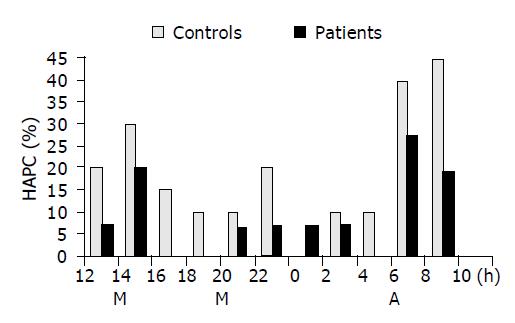
Data on LAPC in STC are still scarce; we have recently shown that this activity may be preserved in such patients, thereby acting as a sort of alternative mechanism able to vicariate, at least in part, the severely impaired main propulsive force (see below)[54]. Conversely, there are several observations showing that HAPC activity is usually deranged, up to complete absence of such events, in severely constipated patients, and especially in those with STC[55-59]; this impairment consists of both a decreased average daily number of HAPC (Figure 6) and decreased amplitude and duration. The latter finding is consistent with the report that HAPC amplitude is a major factor for the propulsion of colonic contents to the rectum[18]. In extreme cases, such an activity is completely absent, and it is also accompanied by almost complete disappearance of the segmental contractile activity: these are the patients with true “colonic inertia”, in whom no medical therapy is successful, and surgical intervention is often the only choice[60,61].
Concerning RMC and periodic colonic motor activity, there is evidence that this kind of activity may be abnormal in STC, with a decreased periodicity and reduced frequency[59,62,63]. A recent investigation, however, reported that these patients may display excessive and un-coordinated RMC activity that, added to the reduced propulsive activity discussed above, may further delay the flow of colonic contents into the rectum[64]. Looking at the daily motor activity, a study showed an overall decrease of colonic contractile activity[65], although the day-night cycle seemed to be maintained, suggesting that normal circadian trend may be preserved, as also shown by a normal contractile response following sudden awakening from sleep[66].
Some of the main physiological reflexes appear to be deranged in STC. In fact, an abnormal motor response to eating seems to be a constant feature in these patients, as shown by both electromyographic and manometric studies consistently demonstrating an overall scarce response to meal ingestion[67-69]. This response is also characterized by a significant impairment of both segmental and propagated activity that follows the meals with respect to that observed in healthy controls[70,71].
Human colonic motor activity is quite a complex issue, still only partly understood and investigated, due to anatomic and physiological difficulties. In recent years, however, some more data have been obtained, even in proximal segments. These data have helped in elucidating, although only in part, some pathophysiological mechanisms of chronic consti-pation, and especially of the STC subtype. Unfortunately, the heterogeneity of the populations under study (that however are probably best selected with respect to other subtypes of constipation) accounts for certain discrepancies in the interpretation of the pathophysiological results. In addition, we are still lacking the “why”, i.e. we need more knowledge about the basic abnormalities of this disorder (nerve and/or smooth muscle involvement), which are still elusive and controversial[72-75], in order to gain a more oriented therapeutic approach to this disease process.
We are warmly indebted to Michela Milanini, MD, for the invaluable help with the illustrations.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Sarna SK. Physiology and pathophysiology of colonic motor activity (1). Dig Dis Sci. 1991;36:827-862. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 151] [Cited by in F6Publishing: 129] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Bassotti G, Germani U, Morelli A. Human colonic motility: physiological aspects. Int J Colorectal Dis. 1995;10:173-180. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 35] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | O'Brien MD, Phillips SF. Colonic motility in health and disease. Gastroenterol Clin North Am. 1996;25:147-162. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Frexinos J, Bueno L, Fioramonti J. Diurnal changes in myoelectric spiking activity of the human colon. Gastroenterology. 1985;88:1104-1110. [PubMed] [Cited in This Article: ] |
| 5. | Narducci F, Bassotti G, Gaburri M, Morelli A. Twenty four hour manometric recording of colonic motor activity in healthy man. Gut. 1987;28:17-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 294] [Cited by in F6Publishing: 252] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 6. | Scott SM. Manometric techniques for the evaluation of colonic motor activity: current status. Neurogastroenterol Motil. 2003;15:483-513. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 83] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Bassotti G, Germani U, Calcara C, Morelli A. Twenty-four hour manometric recording of colonic motility. A technique with both research and clinical identities. Techn Coloproctol. 1996;4:142-144. [Cited in This Article: ] |
| 8. | Rudolph CD, Winter HS. NASPGN guidelines for training in pediatric gastroenterology. NASPGN Executive Council, NASPGN Training and Education Committee. J Pediatr Gastroenterol Nutr. 1999;29 Suppl 1:S1-S26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Bassotti G, Crowell MD. Colon and rectum: normal function and clinical disorder. Manometry. In Schuster MM, Crowell MD, Koch KL, eds. Schuster Atlas of Gastrointestinal Motility in health and disease. 2nd ed. Hamilton BC Decker Inc. 2002;241-252. [Cited in This Article: ] |
| 10. | Crowell MD, Bassotti G, Cheskin LJ, Schuster MM, Whitehead WE. Method for prolonged ambulatory monitoring of high-amplitude propagated contractions from colon. Am J Physiol. 1991;261:G263-G268. [PubMed] [Cited in This Article: ] |
| 11. | Herbst F, Kamm MA, Morris GP, Britton K, Woloszko J, Nicholls RJ. Gastrointestinal transit and prolonged ambulatory colonic motility in health and faecal incontinence. Gut. 1997;41:381-389. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 109] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Rao SS, Sadeghi P, Beaty J, Kavlock R, Ackerson K. Ambulatory 24-h colonic manometry in healthy humans. Am J Physiol Gastrointest Liver Physiol. 2001;280:G629-G639. [PubMed] [Cited in This Article: ] |
| 13. | De Schryver AM, Samsom M, Akkermans LM, Clemens CH, Smout AJ. Fully automated analysis of colonic manometry recordings. Neurogastroenterol Motil. 2002;14:697-703. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Ritchie JA. Colonic motor activity and bowel function. I. Normal movement of contents. Gut. 1968;9:442-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 86] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Bassotti G, Iantorno G, Fiorella S, Bustos-Fernandez L, Bilder CR. Colonic motility in man: features in normal subjects and in patients with chronic idiopathic constipation. Am J Gastroenterol. 1999;94:1760-1770. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 85] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Bassotti G, Bucaneve G, Pelli MA, Morelli A. Contractile frequency patterns of the human colon. J Gastrointest Mot. 1990;2:73-78. [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | García-Olmo D, García-Picazo D, Lopez-Fando J. Correlation between pressure changes and solid transport in the human left colon. Int J Colorectal Dis. 1994;9:87-91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Cook IJ, Furukawa Y, Panagopoulos V, Collins PJ, Dent J. Relationships between spatial patterns of colonic pressure and individual movements of content. Am J Physiol Gastrointest Liver Physiol. 2000;278:G329-G341. [PubMed] [Cited in This Article: ] |
| 19. | De Schryver AM, Samsom M, Smout AJ. In search of objective manometric criteria for colonic high-amplitude propagated pressure waves. Neurogastroenterol Motil. 2002;14:375-381. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Chauve A, Devroede G, Bastin E. Intraluminal pressures during perfusion of the human colon in situ. Gastroenterology. 1976;70:336-340. [PubMed] [Cited in This Article: ] |
| 21. | Gattuso JM, Kamm MA, Myers C, Saunders B, Roy A. Effect of different infusion regimens on colonic motility and efficacy of colostomy irrigation. Br J Surg. 1996;83:1459-1462. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Bassotti G, Gaburri M, Imbimbo BP, Morelli A, Whitehead WE. Distension-stimulated propagated contractions in human colon. Dig Dis Sci. 1994;39:1955-1960. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 43] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Bassotti G, Germani U, Morelli A. Flatus-related colorectal and anal motor events. Dig Dis Sci. 1996;41:335-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Hertz AF. The passage of food along the human alimentary canal. Guy's Hosp Rep. 1907;61:389-427. [Cited in This Article: ] |
| 25. | Torsoli A, Ramorino ML, Ammaturo MV, Capurso L, Paoluzi P, Anzini F. Mass movements and intracolonic pressures. Am J Dig Dis. 1971;16:693-696. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 41] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Ritchie JA, Truelove SC, Ardan GM, Tuckey MS. Propulsion and retropulsion of normal colonic contents. Am J Dig Dis. 1971;16:697-704. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Bassotti G, Gaburri M. Manometric investigation of high-amplitude propagated contractile activity of the human colon. Am J Physiol. 1988;255:G660-G664. [PubMed] [Cited in This Article: ] |
| 28. | Bassotti G, Betti C, Fusaro C, Morelli A. Colonic high-amplitude propagated contractions (mass movements): repeated 24-h studies in healthy volunteers. J Gastrointest Mot. 1992;4:187-191. [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Kamm MA, van der Sijp JR, Lennard-Jones JE. Colorectal and anal motility during defaecation. Lancet. 1992;339:820. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 45] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 30. | Bampton PA, Dinning PG, Kennedy ML, Lubowski DZ, deCarle D, Cook IJ. Spatial and temporal organization of pressure patterns throughout the unprepared colon during spontaneous defecation. Am J Gastroenterol. 2000;95:1027-1035. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 135] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 31. | Orkin BA, Hanson RB, Kelly KA. The rectal motor complex. J Gastrointest Mot. 1989;1:5-8. [DOI] [Cited in This Article: ] |
| 32. | Hagger R, Kumar D, Benson M, Grundy A. Periodic colonic motor activity identified by 24-h pancolonic ambulatory manometry in humans. Neurogastroenterol Motil. 2002;14:271-278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 33. | Rao SS, Welcher K. Periodic rectal motor activity: the intrinsic colonic gatekeeper? Am J Gastroenterol. 1996;91:890-897. [PubMed] [Cited in This Article: ] |
| 34. | Orkin BA, Hanson RB, Kelly KA, Phillips SF, Dent J. Human anal motility while fasting, after feeding, and during sleep. Gastroenterology. 1991;100:1016-1023. [PubMed] [Cited in This Article: ] |
| 35. | Furukawa Y, Cook IJ, Panagopoulos V, McEvoy RD, Sharp DJ, Simula M. Relationship between sleep patterns and human colonic motor patterns. Gastroenterology. 1994;107:1372-1381. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 90] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Roarty TP, Suratt PM, Hellmann P, McCallum RW. Colonic motor activity in women during sleep. Sleep. 1998;21:285-288. [PubMed] [Cited in This Article: ] |
| 37. | Steadman CJ, Phillips SF, Camilleri M, Haddad AC, Hanson RB. Variation of muscle tone in the human colon. Gastroenterology. 1991;101:373-381. [PubMed] [Cited in This Article: ] |
| 38. | Christensen J. The response of the colon to eating. Am J Clin Nutr. 1985;42:1025-1032. [PubMed] [Cited in This Article: ] |
| 39. | Bassotti G, Imbimbo BP, Gaburri M, Daniotti S, Morelli A. Transverse and sigmoid colon motility in healthy humans: effects of eating and of cimetropium bromide. Digestion. 1987;37:59-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 33] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | Steadman CJ, Phillips SF, Camilleri M, Talley NJ, Haddad A, Hanson R. Control of muscle tone in the human colon. Gut. 1992;33:541-546. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 62] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 41. | Wiley J, Tatum D, Keinath R, Chung OY. Participation of gastric mechanoreceptors and intestinal chemoreceptors in the gastrocolonic response. Gastroenterology. 1988;94:1144-1149. [PubMed] [Cited in This Article: ] |
| 42. | Rao SS, Kavelock R, Beaty J, Ackerson K, Stumbo P. Effects of fat and carbohydrate meals on colonic motor response. Gut. 2000;46:205-211. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 88] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 43. | Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45 Suppl 2:II43-II47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 622] [Cited by in F6Publishing: 817] [Article Influence: 32.7] [Reference Citation Analysis (0)] |
| 44. | Locke GR, Pemberton JH, Phillips SF. AGA technical review on constipation. American Gastroenterological Association. Gastroenterology. 2000;119:1766-1778. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 216] [Cited by in F6Publishing: 235] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 45. | Sagar PM, Pemberton JH. Anorectal and pelvic floor function. Relevance of continence, incontinence, and constipation. Gastroenterol Clin North Am. 1996;25:163-182. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 46. | Bassotti G, Chistolini F, Sietchiping-Nzepa F, de Roberto G, Morelli A, Chiarioni G. Biofeedback for pelvic floor dysfunction in constipation. BMJ. 2004;328:393-396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 47. | Knowles CH, Martin JE. Slow transit constipation: a model of human gut dysmotility. Review of possible aetiologies. Neurogastroenterol Motil. 2000;12:181-196. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 91] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 48. | Bharucha AE, Phillips SF. Slow transit constipation. Gastroenterol Clin North Am. 2001;30:77-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 49. | Waldron D, Bowes KL, Kingma YJ, Cote KR. Colonic and anorectal motility in young women with severe idiopathic constipation. Gastroenterology. 1988;95:1388-1394. [PubMed] [Cited in This Article: ] |
| 50. | Preston DM, Lennard-Jones JE. Pelvic motility and response to intraluminal bisacodyl in slow-transit constipation. Dig Dis Sci. 1985;30:289-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 88] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 51. | Ferrara A, Pemberton JH, Grotz RL, Hanson RB. Prolonged ambulatory recording of anorectal motility in patients with slow-transit constipation. Am J Surg. 1994;167:73-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 52. | Bassotti G, Chiarioni G, Imbimbo BP, Betti C, Bonfante F, Vantini I, Morelli A, Whitehead WE. Impaired colonic motor response to cholinergic stimulation in patients with severe chronic idiopathic (slow transit type) constipation. Dig Dis Sci. 1993;38:1040-1045. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 68] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 53. | Bassotti G, Chistolini F, Battaglia E, Chiarioni G, Nzepa FS, Dughera L, deRoberto G, Emanuelli G, Morelli A. Are colonic regular contractile frequency patterns in slow transit constipation a relevant pathophysiological phenomenon? Dig Liver Dis. 2003;35:552-556. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 54. | Bassotti G, Chistolini F, Nzepa FS, Morelli A. Colonic propulsive impairment in intractable slow-transit constipation. Arch Surg. 2003;138:1302-1304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 55. | Kamm MA, van der Sijp JR, Lennard-Jones JE. Observations on the characteristics of stimulated defaecation in severe idiopathic constipation. Int J Colorectal Dis. 1992;7:197-201. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 50] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 56. | Bassotti G, Chiarioni G, Vantini I, Betti C, Fusaro C, Pelli MA, Morelli A. Anorectal manometric abnormalities and colonic propulsive impairment in patients with severe chronic idiopathic constipation. Dig Dis Sci. 1994;39:1558-1564. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 78] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 57. | Bassotti G, Chiarioni G, Germani U, Battaglia E, Vantini I, Morelli A. Endoluminal instillation of bisacodyl in patients with severe (slow transit type) constipation is useful to test residual colonic propulsive activity. Digestion. 1999;60:69-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 58. | Björnsson ES, Chey WD, Hooper F, Woods ML, Owyang C, Hasler WL. Impaired gastrocolonic response and peristaltic reflex in slow-transit constipation: role of 5-HT(3) pathways. Am J Physiol Gastrointest Liver Physiol. 2002;283:G400-G407. [PubMed] [Cited in This Article: ] |
| 59. | Hagger R, Kumar D, Benson M, Grundy A. Colonic motor activity in slow-transit idiopathic constipation as identified by 24-h pancolonic ambulatory manometry. Neurogastroenterol Motil. 2003;15:515-522. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 60. | Bassotti G, Betti C, Pelli MA, Morelli A. Extensive investigation on colonic motility with pharmacological testing is useful for selecting surgical options in patients with inertia colica. Am J Gastroenterol. 1992;87:143-147. [PubMed] [Cited in This Article: ] |
| 61. | Shafik A, Shafik AA, El-Sibai O, Mostafa RM. Electric activity of the colon in subjects with constipation due to total colonic inertia: an electrophysiologic study. Arch Surg. 2003;138:1007-1011; discussion 1011. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 62. | Waldron DJ, Kumar D, Hallan RI, Wingate DL, Williams NS. Evidence for motor neuropathy and reduced filling of the rectum in chronic intractable constipation. Gut. 1990;31:1284-1288. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 63. | Bassotti G, Betti C, Pelli MA, Morelli A. Prolonged (24-hour) manometric recording of rectal contractile activity in patients with slow transient constipation. Digestion. 1991;49:72-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 64. | Rao SS, Sadeghi P, Batterson K, Beaty J. Altered periodic rectal motor activity: a mechanism for slow transit constipation. Neurogastroenterol Motil. 2001;13:591-598. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 65. | Bassotti G, Gaburri M, Imbimbo BP, Rossi L, Farroni F, Pelli MA, Morelli A. Colonic mass movements in idiopathic chronic constipation. Gut. 1988;29:1173-1179. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 190] [Cited by in F6Publishing: 199] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 66. | Bassotti G, Germani U, Fiorella S, Roselli P, Brunori P, Whitehead WE. Intact colonic motor response to sudden awakening from sleep in patients with chronic idiopathic (slow-transit) constipation. Dis Colon Rectum. 1998;41:1550-1555; discussion 1555-1556. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 67. | Schang JC, Devroede G, Duguay C, Hémond M, Hébert M. Constipation caused by colonic inertia and distal obstruction: electromyographic study. Gastroenterol Clin Biol. 1985;9:480-485. [PubMed] [Cited in This Article: ] |
| 68. | Bazzocchi G, Ellis J, Villanueva-Meyer J, Jing J, Reddy SN, Mena I, Snape WJ. Postprandial colonic transit and motor activity in chronic constipation. Gastroenterology. 1990;98:686-693. [PubMed] [Cited in This Article: ] |
| 69. | Bassotti G, Morelli A, Whitehead WE. Abnormal rectosigmoid myoelectric response to eating in patients with severe idiopathic constipation (slow-transit type). Dis Colon Rectum. 1992;35:753-756. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 70. | Bassotti G, Imbimbo BP, Betti C, Dozzini G, Morelli A. Impaired colonic motor response to eating in patients with slow-transit constipation. Am J Gastroenterol. 1992;87:504-508. [PubMed] [Cited in This Article: ] |
| 71. | De Schryver AM, Samsom M, Smout AI. Effects of a meal and bisacodyl on colonic motility in healthy volunteers and patients with slow-transit constipation. Dig Dis Sci. 2003;48:1206-1212. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 71] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 72. | Knowles CH, Nickols CD, Scott SM, Bennett NI, de Oliveira RB, Chimelli L, Feakins R, Williams NS, Martin JE. Smooth muscle inclusion bodies in slow transit constipation. J Pathol. 2001;193:390-397. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 73. | Wedel T, Roblick UJ, Ott V, Eggers R, Schiedeck TH, Krammer HJ, Bruch HP. Oligoneuronal hypoganglionosis in patients with idiopathic slow-transit constipation. Dis Colon Rectum. 2002;45:54-62. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 79] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 74. | Tomita R, Fujisaki S, Ikeda T, Fukuzawa M. Role of nitric oxide in the colon of patients with slow-transit constipation. Dis Colon Rectum. 2002;45:593-600. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 75. | Lyford GL, He CL, Soffer E, Hull TL, Strong SA, Senagore AJ, Burgart LJ, Young-Fadok T, Szurszewski JH, Farrugia G. Pan-colonic decrease in interstitial cells of Cajal in patients with slow transit constipation. Gut. 2002;51:496-501. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 203] [Article Influence: 9.2] [Reference Citation Analysis (0)] |