Published online Nov 1, 2004. doi: 10.3748/wjg.v10.i21.3230
Revised: February 14, 2004
Accepted: February 21, 2004
Published online: November 1, 2004
AIM: To determine and compare the effect of vagus nerve on gallbladder motility in patients with hepatic cirrhosis before and after portal azygous disconnection (PAD).
METHODS: PAD operation (or Hassab’s operation) was performed on 18 patients with portal hypertension, and anterior and posterior vagal trunks were cut. On d 3 before operation and d 10 after operation, 99mTc-EHIDA 185 MBq was administered intravenously to the patients, and scintigraphy was performed at 0.25 min/frame. A standard fat meal was administered 30 min after scintigraphy, and dynamic imaging was performed 60 min after the fat meal. Following appearance of the region of interest (ROI) in gallbladder, the time-activity curve of ROI was established. The following seven parameters were used: Radioactivity at 30 min after injection of 99mTc-EHIDA (RC 30min), bile emptying fraction (EF), bile emptying period (EP), emptying rate (ER), latent period (LP), latent period radiocounting increment (LI), and latent period radiocounting increment rate (LR).
RESULTS: The RC 30 min decreased significantly after operation, compared with that before operation (2 693.6 ± 2 406.9 vs 5 606.8 ± 2 625.4, P < 0.05). The radiocounting of gallbladder increased gradually during LP. LP after operation was significantly longer than that before operation (13.36 ± 5.92 vs 2.24 ± 1.48, P < 0.01). LI and LR after operation were significantly higher than those before operation (2 861.62 ± 028.3 vs 331.21 ± 421.02, and 113.42 ± 49.52 vs 7.57 ± 10.75, respectively, both P < 0.01). EP after operation was significantly shorter than that before operation (18.5 ± 6.3 vs 24.1 ± 6.4, P < 0.05). EF and ER after operation were significantly lower than those before operation (13.1 ± 5.4 vs 32.3 ± 16.3, and 0.7 ± 0.3 vs 1.4 ± 0.8, respectively, both P < 0.01).
CONCLUSION: PAD operation is a good clinical model in studying the effect of vagus on gallbladder motility. The gallbladder tension after PAD operation decreases significantly during the interdigestive phase. The latent period of gallbladder contraction prolongs and the motility weakens apparently after a standard fat meal. Human vagus influences the gallbladder motility, and cutting of the nerve inhibits the gallbladder motility.
- Citation: Jin HX, Wu SD, Zhang XF, Chen XY, Zhang GX. Gallbladder motility in patients with hepatic cirrhosis before and after portal azygous disconnection. World J Gastroenterol 2004; 10(21): 3230-3233
- URL: https://www.wjgnet.com/1007-9327/full/v10/i21/3230.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i21.3230
Cholecystolithiasis results from multi-factors[1-5], of which gallbladder motor disfunction is an important factor[5,6]. Gallbladder motility is regulated by nerve system and body fluid[7], especially the vagus[8-10]. Because of the complicated interfering factor and its difficulty in control, there were few clinical studies on the gallbladder motility. In this study, vagus nerve effect on gallbladder motility was studied in patients with liver cirrhosis.
Eighteen patients with portal hypertension (10 males and 8 females) with an average age of 50 years were included in this study. They had hypersplenotrophy and certain degree of hypersplenia. The esophagogastric varication was confirmed with gastroscope. No biliary abnormalities were found with ultrasonography. Hepatic function was classified as Child A level. Splenectomy (Hassab’s operation) was performed, anterior and posterior trunks of vagus were cut off after inferior segment of esophagus was liberated. Aerofluxus was observed 48-96 h after operation. Hepatic function was recovered to Child A level 10 d postoperation.
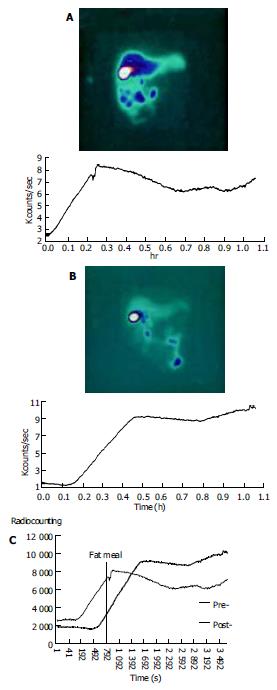
With empty stomach on d 3 preoperation and d 10 postoperation, respectively, 99mTc-labeled diethyl acetyl acid anilide iminodiacetic acid scintigraphy (99mTc-EHIDA) 185 MBq was administered intravenously. American SPECT of GE Company was adopted to perform scintigraphy, 0.25 min/frame. Standard fat meals (ENSURE 250 mL standard solution containing caloric 1046.0 KJ, protein 14%, fattiness 31.5%, carbohydrate 54.5%) was provided for patients after 30 min of continuous displaying. The region of interest (ROI) in gallbladder and the time-activity curve of ROI were established (Figures 1A, B). Then, 7 parameters were used to analyze. the radiocounting of 99mTc-EHIDA injected 30 min later (RC 30 min), emptying fraction (EF, %), emptying period (EP min), emptying rate (ER, %/min): EF/EP, latent period (LP, min): The time from having fat meal to the initiation of contraction of gallbladder, latent period radiocounting increment (LI), latent period radiocounting increment rate (LR, %): The increased amount of radioactivity during LP/the initial radioactivity of LP × 100. The results were expressed as mean ± SD. SPSS11.0 software was used for analysis.
Each of the paired pre- and post-operative parameters was proved in normal distribution by normality test (Table 1).
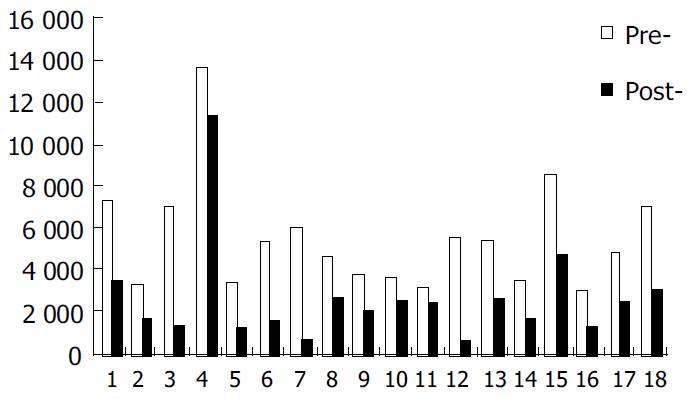
Serum 99mTc-EHIDA in blood was rapidly taken by liver, egested to biliary system, stored and concentrated in gallbladder. Thirty min after injecting 99mTc-EHIDA, the radioactivity in gallbladder could reflect the bile quantity entered to gallbladder during interdigestive phase. The RC 30 min postoperation decreased obviously than that preoperation (2693.6 ± 2406.9 vs 5606.8 ± 2625.4, P < 0.05) (Figure 2).
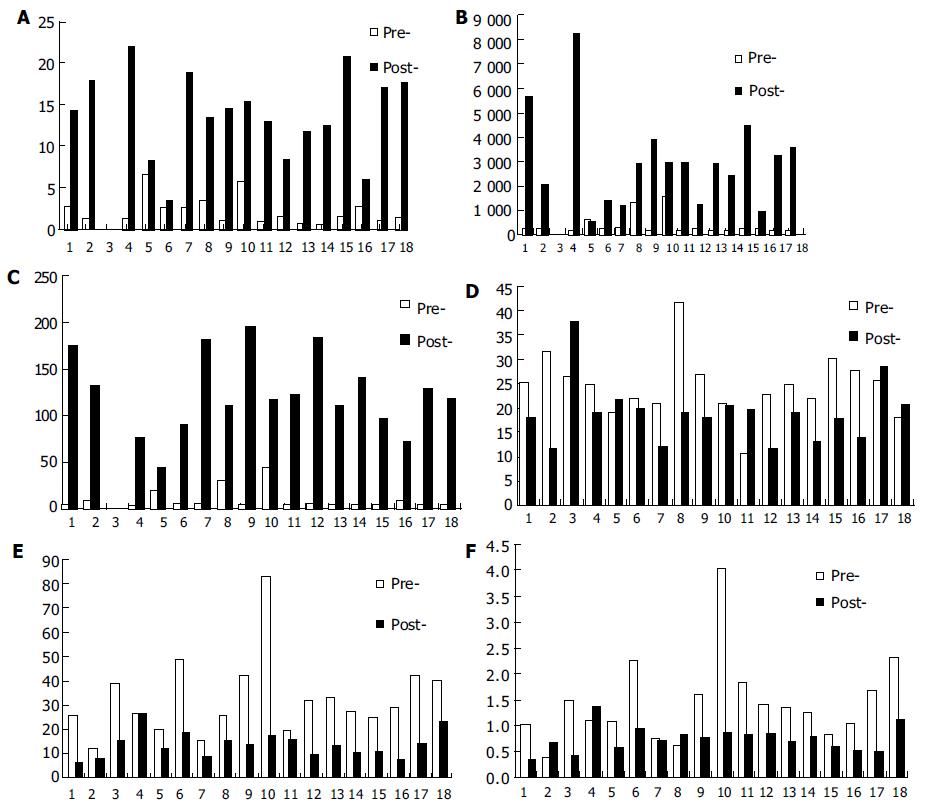
LP in cirrhosis patients was very short preoperation, and LP prolonged significantly postoperation (13.36 ± 5.92 vs 2.24 ± 1.48, P < 0.01). The radioactivity in gallbladder in LP increased gradually. LI and LR increased significantly postoperation (2861.6 ± 2028.3 vs 331.21 ± 421.02, 113.42 ± 49.52 vs 7.57 ± 10.75, P < 0.01) (Figures 3A, B, C). EP in cirrhotic patients was shorter postoperation than that preoperation, EF and ER decreased significantly (13.1 ± 5.4 vs 32.3 ± 16.3, 0.7 ± 0.3 vs 1.4 ± 0.8, P < 0.01) (Figures 3D, E, F).
The Portal azygous disconnection (PAD) is a clinical research model to study the function of human vagus. Most studies on vagus function in gallbladder motility were limited to animal experiments[9-13]. Some scholars studied the gallbladder motility after gastrectomy and speculated that human vagus had an important effect on gallbladder motility[14-16]. In PAD anterior and posterior trunks of vagus were cut, while the integrality of alimentary canal was maintained. Therefore, PAD could eliminate many disturbing factors. Although the basic liver function of patients could disturb the research, we reduced the disturbance to the lowest degree by adjusting liver function of every patient to Child A level, and auto-control method was used on same patient pre- and post-operation.
Radioactive nuclide 99mTc-EHIDA can be specifically taken by liver cells, then egested with bile and discharged through biliary system to intestinal tract. Dynamic flowing of bile can be displayed accurately by SPECT scintigraphy with a clear picture and a high resolution. It has little radiation damage to the patients, and is a good way to study the motility of gallbladder and biliary system
Gallbladder motility is regulated by nerve system and body fluid factors. Gallbladder emptying after ingestion is affected by multiple factors. Vagus cholinergic fibers could cause gallbladder empty after ingestion, sham feeding could result in gallbladder emptying to 25%-56%, and this function could be inhibited by cutting vagus or injection of atropine.
Acetylcholine and other parasympathomimetic drugs could enhance the gallbladder tension and motility. Stimulating the vagus of dogs with electric current caused contraction of gallbladder, and gallbladder contracted slowly after both sides of the vagus were completely cut[10]. In our study, vagus in patients with liver cirrhosis was cut off in PAD to study its effect on gallbladder motility. 99mTc-EHIDA scintigraphy was used. Gallbladder motility was compared between pre- and post-PAD. We found that EP was shortened post-PAD (P < 0.05), EF and ER were significantly reduced, and the motility of gallbladder was obviously weak after meal. Our study showed that human vagus had an important regulatory effect on gallbladder motility after meal.
Vagus is an important factor for maintaining gallbladder tension during interdigestive phase[11,13,22], the gallbladder volume could increase two times if both sides of vagus were completely cut[10]. Gallbladder was a weak in situation during interdigestive phase, and appeared rhythmic contraction and relaxation[11]. Tenuity bile was continuously excreted by liver exchanges with condensed bile stored in gallbladder[23-25]. Our study showed that RC 30 min post-operation was significantly decreased when fasting. The reason might be that cutting the vagus reduced the gallbladder tension during interdigestive phase, and then affected the exchange of bile.
Cholecystolithiasis patients did not contract at once after meal, but had a long latent period[26]. In this study, LP post-operation after fat meal was prolonged (P < 0.01). The gallbladder lost the contractive stimulation in cephalic phase after vagus was cut. The result in our study was similar to that previously described[27] (LI 2861.6 ± 2028.3, LR 113.42% ± 49.52%). We conclude that bile containing nuclides entering into gallbladder more rapidly results from the heightened pressure of biliary tract. The motility of Oddi’s sphincter is adjusted by vagus[11], and the bile excreted by liver is mainly adjusted by body fluid[28-31]. Fat meal may increase the bile excreted by liver through humoral regulation, and amputation of the vagus can weaken the contraction of Oddi’s sphincter cephalic phase, so the pressure of biliary tract increases. Further study is required for clarifying the mechanism in detail.
Edited by Ren SY and Wang XL Proofread by Xu FM
| 1. | Vítek L, Carey MC. Enterohepatic cycling of bilirubin as a cause of 'black' pigment gallstones in adult life. Eur J Clin Invest. 2003;33:799-810. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 61] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Wang DQ, Carey MC. Susceptibility to murine cholesterol gallstone formation is not affected by partial disruption of the HDL receptor SR-BI. Biochim Biophys Acta. 2002;1583:141-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Chuang CZ, Martin LF, LeGardeur BY, Lopez A. Physical activity, biliary lipids, and gallstones in obese subjects. Am J Gastroenterol. 2001;96:1860-1865. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Behar J. Clinical aspects of gallbladder motor function and dysfunction. Curr Gastroenterol Rep. 1999;1:91-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Rubin M, Pakula R, Konikoff FM. Microstructural analysis of bile: relevance to cholesterol gallstone pathogenesis. Histol Histopathol. 2000;15:761-770. [PubMed] [Cited in This Article: ] |
| 6. | Shi JS, Ma JY, Zhu LH, Pan BR, Wang ZR, Ma LS. Studies on gallstone in China. World J Gastroenterol. 2001;7:593-596. [PubMed] [Cited in This Article: ] |
| 7. | Wang J, Luo J, Yu X. [Study on biliary motility in cirrhotic patients with portal hypertension]. Zhonghua Ganzangbing Zazhi. 2000;8:35-36. [PubMed] [Cited in This Article: ] |
| 8. | Shaffer EA. Review article: control of gall-bladder motor function. Aliment Pharmacol Ther. 2000;14 Suppl 2:2-8. [PubMed] [Cited in This Article: ] |
| 9. | Axelsson HG. Effects of gallstone-promoting diet and vagotomy on the mouse gallbladder epithelium. Hepatogastroenterology. 1999;46:2149-2152. [PubMed] [Cited in This Article: ] |
| 10. | Muramatsu S, Sonobe K, Tohara K, Tanaka T, Mizumoto A, Ibuki R, Suzuki H, Itoh Z. Effect of truncal vagotomy on gallbladder bile kinetics in conscious dogs. Neurogastroenterol Motil. 1999;11:357-364. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Liu CY, Liu JZ, Li ZY, Liu KJ. [The vagus nerve coordinates the motion of gallbladder and sphincter of Oddi in the interdigestive period in rabbits]. Zhongguo Yingyongshenglixue Zazhi. 2000;16:347-349. [PubMed] [Cited in This Article: ] |
| 12. | Tsukamoto M, Enjoji A, Ura K, Kanematsu T. Preserved extrinsic neural connection between gallbladder and residual stomach is essential to prevent dysmotility of gallbladder after distal gastrectomy. Neurogastroenterol Motil. 2000;12:23-31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Xie YF, Liu CY, Liu JZ. Nucleus raphe obscurus participates in regulation of gallbladder motility through vagus and sympathetic nerves in rabbits. Chin J Physiol. 2002;45:101-107. [PubMed] [Cited in This Article: ] |
| 14. | Kinoshita H, Imayama H, Hashino K, Aoyagi S. Study of cholelithiasis after gastrectomy. Kurume Med J. 2000;47:105-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Hagiwara A, Imanishi T, Sakakura C, Otsuji E, Kitamura K, Itoi H, Yamagishi H. Subtotal gastrectomy for cancer located in the greater curvature of the middle stomach with prevention of the left gastric artery. Am J Surg. 2002;183:692-696. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Vassilakis JS, Pechlivanides G, Fountos A, Zoras OJ, Xynos E. Roux-en-Y gastroenterostomy severely disturbs emptying of the gallbladder. J Am Coll Surg. 1994;179:313-317. [PubMed] [Cited in This Article: ] |
| 17. | Madácsy L, Velosy B, Szepes A, Szilvássy Z, Pávics L, Csernay L, Lonovics J. Effect of nitric oxide on gallbladder motility in patients with acalculous biliary pain: a cholescintigraphic study. Dig Dis Sci. 2002;47:1975-1981. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Chen SD, Tsai SC, Shiau YC, Ho YJ, Kao CH. Evidence of gallbladder function changes in hepatoma after transcatheter arterial embolization by quantitative Tc-99m DISIDA cholescintigraphy. Hepatogastroenterology. 2001;48:393-396. [Cited in This Article: ] |
| 19. | Kao CH, Hsieh JF, Tsai SC, Ho YJ, Chen SD. Evidence of impaired gallbladder function in patients with liver cirrhosis by quantitative radionuclide cholescintigraphy. Am J Gastroenterol. 2000;95:1301-1304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Robertson MD, Mason AO, Frayn KN. Timing of vagal stimulation affects postprandial lipid metabolism in humans. Am J Clin Nutr. 2002;76:71-77. [PubMed] [Cited in This Article: ] |
| 21. | Fisher RS, Rock E, Malmud LS. Gallbladder emptying response to sham feeding in humans. Gastroenterology. 1986;90:1854-1857. [PubMed] [Cited in This Article: ] |
| 22. | Parkman HP, Pagano AP, Ryan JP. Investigation of endogenous neurotransmitters of guinea pig gallbladder using nicotinic agonist stimulation. Dig Dis Sci. 1998;43:2237-2243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Woods CM, Mawe GM, Shaffer EA, Toouli J, T P Saccone G. Effects of bioactive agents on biliary motor function. Curr Gastroenterol Rep. 2003;5:154-159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | von Kiedrowski R, Huijghebaert S, Raedsch R. Mechanisms of cisapride affecting gallbladder motility. Dig Dis Sci. 2001;46:939-944. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Luiking YC, Akkermans LM, Peeters TL, Cnossen PJ, Nieuwenhuijs VB, Vanberge -Henegouwen GP. Effects of motilin on human interdigestive gastrointestinal and gallbladder motility, and involvement of 5HT3 receptors. Neurogastroenterol Motil. 2002;14:151-159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Xynos E, Pechlivanides G, Zoras OJ, Chrysos E, Tzovaras G, Fountos A, Vassilakis JS. Reproducibility of gallbladder emptying scintigraphic studies. J Nucl Med. 1994;35:835-839. [PubMed] [Cited in This Article: ] |
| 27. | Pazzi P, Petroni ML, Prandini N, Adam JA, Gullini S, Northfield TC, Jazrawi RP. Postprandial refilling and turnover: specific gallbladder motor function defects in patients with gallstone recurrence. Eur J Gastroenterol Hepatol. 2000;12:787-794. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Trauner M, Boyer JL. Bile salt transporters: molecular characterization, function, and regulation. Physiol Rev. 2003;83:633-671. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 737] [Cited by in F6Publishing: 655] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 29. | García F, Kierbel A, Larocca MC, Gradilone SA, Splinter P, LaRusso NF, Marinelli RA. The water channel aquaporin-8 is mainly intracellular in rat hepatocytes, and its plasma membrane insertion is stimulated by cyclic AMP. J Biol Chem. 2001;276:12147-12152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 159] [Cited by in F6Publishing: 162] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 30. | St-Pierre MV, Kullak-Ublick GA, Hagenbuch B, Meier PJ. Transport of bile acids in hepatic and non-hepatic tissues. J Exp Biol. 2001;204:1673-1686. [PubMed] [Cited in This Article: ] |
| 31. | Hooiveld GJ, van Montfoort JE, Meijer DK, Müller M. Function and regulation of ATP-binding cassette transport proteins involved in hepatobiliary transport. Eur J Pharm Sci. 2001;12:525-543. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |