Copyright
©2006 Baishideng Publishing Group Co.
World J Gastroenterol. May 28, 2006; 12(20): 3139-3145
Published online May 28, 2006. doi: 10.3748/wjg.v12.i20.3139
Published online May 28, 2006. doi: 10.3748/wjg.v12.i20.3139
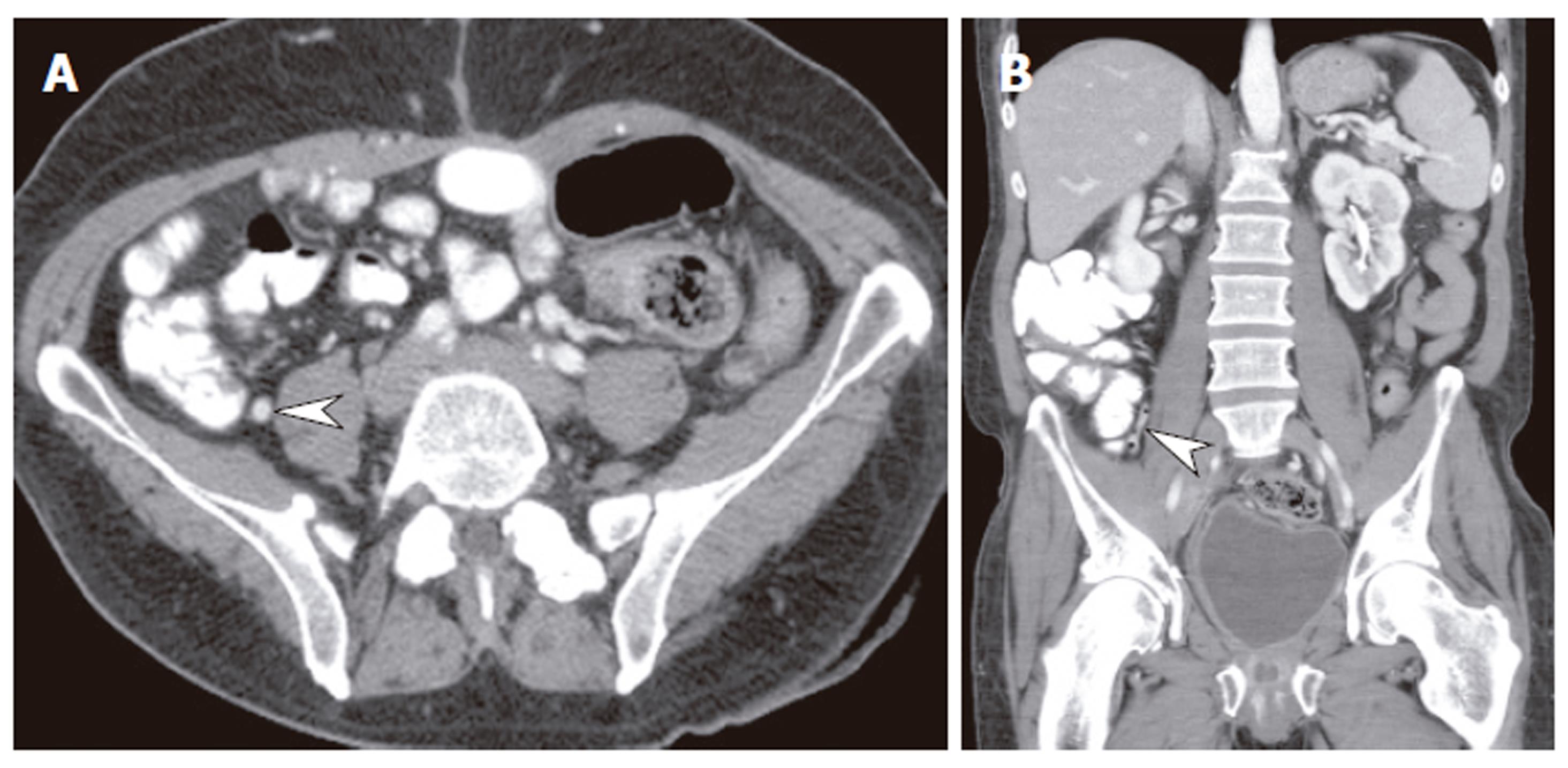
Figure 1 Sixty-three years old man with right lower quadrant abdominal pain.
Note the equivalent resolution of the axial image (A) and coronal reformat (B). In addition it was easier to appreciate the vertically oriented normal appendix (arrowhead) on the coronal reformat.
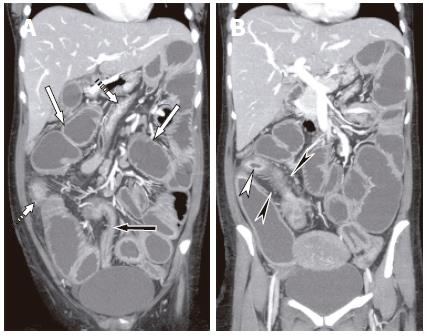
Figure 2 Abdominal pain and fever in 23 years old female.
A, B: Coronal reformats with neutral enteral contrast (water) showed dilated proximal loops of small bowel (white solid arrows), and nondistended colon (dashed arrows). A segment of distal ileum (black arrow, image A) showed stenosis with mucosal enhancement, consistent with inflammatory stricture causing small bowel obstruction. A second noncontiguous segment of terminal ileum showed intense mucosal enhancement (white arrowhead, image B) and comb sign due to mesenteric hypervascularity (black arrowhead, image B). The appearances were consistent with acute Crohn’s disease. The diagnosis of wall enhancement and thickening is made easier by using water as oral contrast. The coronal perspective also allows easier evaluation of length of involved segments.
Figure 3 Three dimensional volume rendered image of small and large bowel in 46 years old female with diarrhea.
There was no evidence of bowel obstruction. The apparent narrowing of ascending colon (arrowhead) was likely to be due to passage of peristalsis, there was no evidence of mass on two dimensional axial and coronal images. Three dimensional images may be more commonly used in the future to help plan surgery.
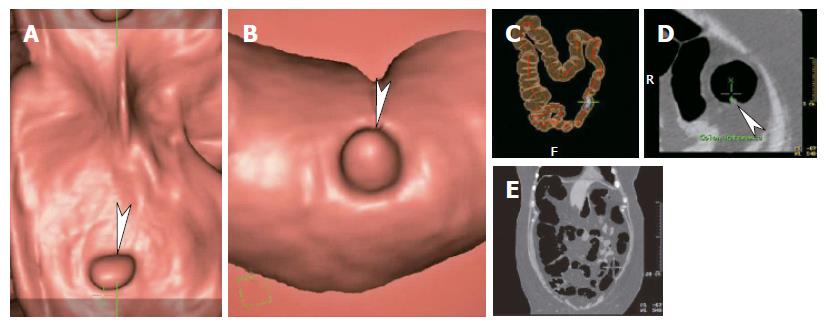
Figure 4 Virtual colonoscopy images in 62 years old female with incomplete optical colonoscopy.
A: Dissection or fillet view; B: Endoluminal fly-through view; C: Transparent localizing view; D: Two dimensional axial view; E: Two dimensional coronal view. At our institution the initial read is the 3 dimensional fillet and endoluminal views in antegrade and retrograde fashion. Sites of concern are correlated with axial or coronal two dimensional views. The entire interpretation including assessment of extracolonic structures takes about 30 min. Note the 6 mm polyp (arrowhead). Its location was confirmed as distal descending colon on image C.
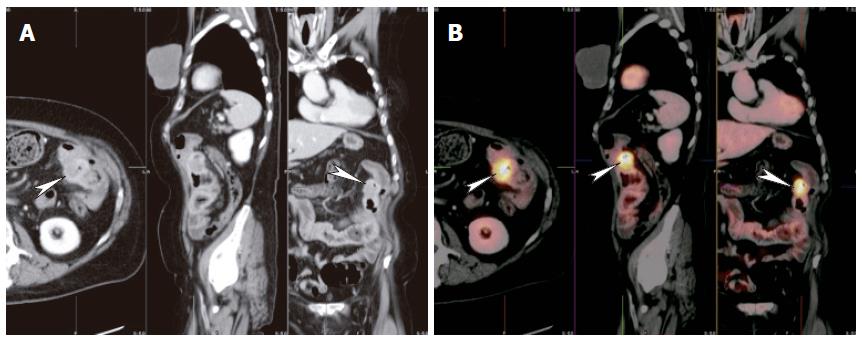
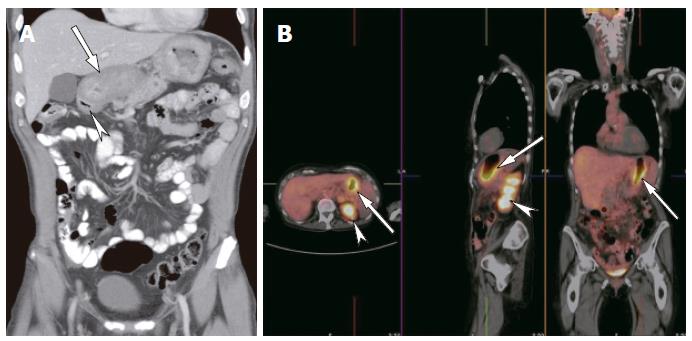
Figure 5 Thirty-nine years old female with prior sigmoid colectomy for cancer, presented with rising CA-125.
A: Axial, coronal and sagittal images of CT raised concern for possible mass adjacent to the splenic flexure (arrowheads); B: Fused images of PET and CT showed hypermetabolic focus (arrowheads) in the mesocolon adjacent to splenic flexure, indicating recurrent tumor. No other sites of tumor were found. While PET is sensitive for recurrent disease it has poor spatial resolution and it would have been difficult to determine if the recurrence was in the colon, mesentery or adjacent spleen. Fusion of PET and CT images allowed accurate anatomical localization.
Figure 6 Sixty-nine years old male with dyspepsia.
A: Coronal reformat showed diffuse thickening of the gastric wall (arrow). The duodenal cap was normal (arrowhead); B: Fused PET-CT images showed hypermetabolic activity of the gastric wall indicating cancer. No other foci of abnormal uptake were identified. Note the normal increased activity in the renal collecting systems (arrowheads) due to excretion of radiopharmaceutical.
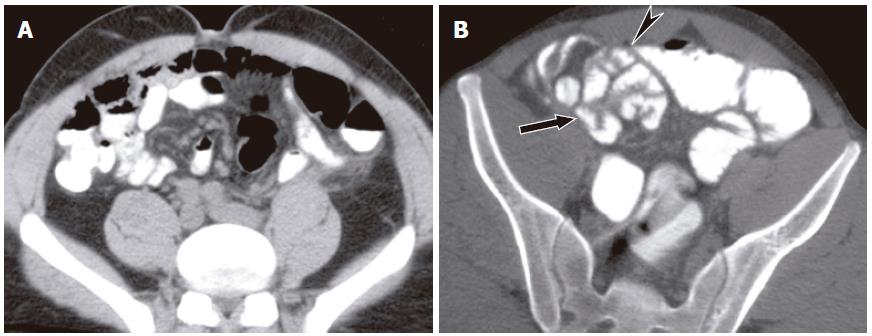
Figure 7 Fifty-four years old with prior hysterectomy presented with abdominal bloating and nausea.
A: Conventional CT did not show distended bowel or transition point and was interpreted as normal; B: CT enteroclysis performed a day later shows distended small bowel loop with beaking (arrowhead) adjacent to anterior parietal peritoneum. Distal small bowel loops were nondistended (arrow). The appearances were of low grade small bowel obstruction due to adhesions.
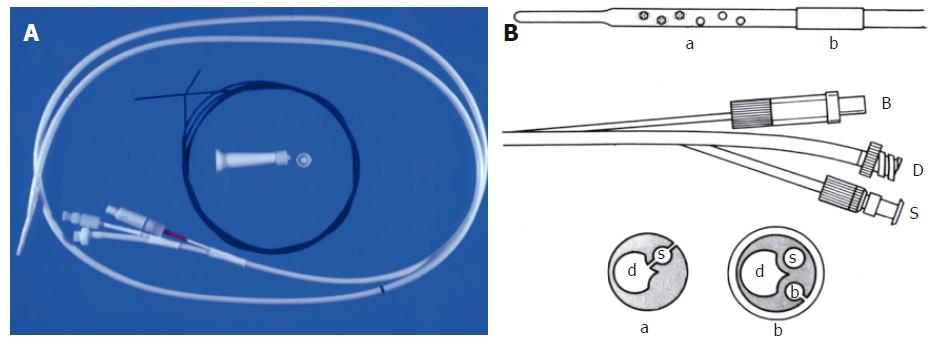
Figure 8 A: Image of MDEC decompression and enteroclysis tube with stiffening wire that helps maneuvering the tube into the proximal jejunum; B: Line diagram of the tube.
B = balloon port, D = drainage port, S = sump port (helps prevent the tube from becoming obstructed by debris). The inset figures show the cross sectional appearances of the tube at positions a and b.
Figure 9 Neutral enteral contrast CT enteroclysis in 27 years old female presented with chronic diarrhea and anemia.
There was a prior history of systemic lupus erythematosis. Coronal reformat showed diffuse smooth small bowel wall (arrow) and fold thickening. Small bowel biopsy showed vasculitis.
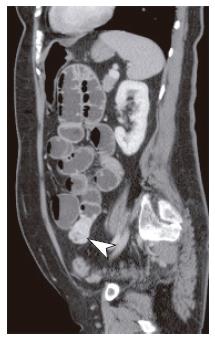
Figure 10 Sagittal reformat of CT enteroclysis in 63 years old female with unexplained gastrointestinal (GI) bleeding showed 3 cm hypervascular submucosal mass (arrow) arising from mid small bowel, proven as a gastrointestinal stromal tumor at surgery.
Prior capsule endocsopy had shown no abnormality, other than jejunal angioectasia.
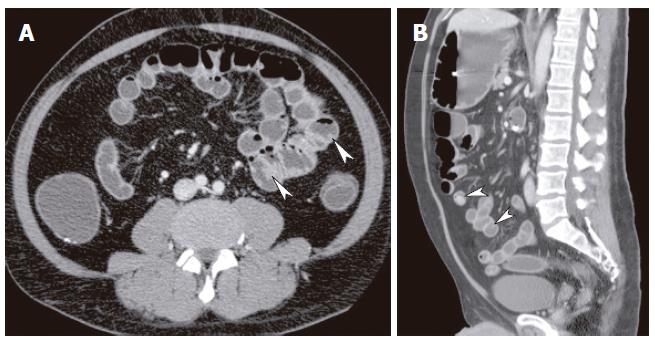
Figure 11 Fifty-two years old male with known Peutz-Jeghers syndrome.
Axial (A) and sagittal (B) images showed multiple polyps of varying sizes in the small bowel (arrowheads). Information regarding the location and sizes of polyps was valuable in performing double balloon endoscopic polypectomy.
Figure 12 Metastatic carcinoid in 59 years old female presenting diarrhea and wheezing.
Coronal reformat of isotropic resolution CT enteroclysis performed with neutral enteral contrast showed 3 cm hypervascular mass in distal ileum (arrowhead) and hypervascular liver metastases (arrow).
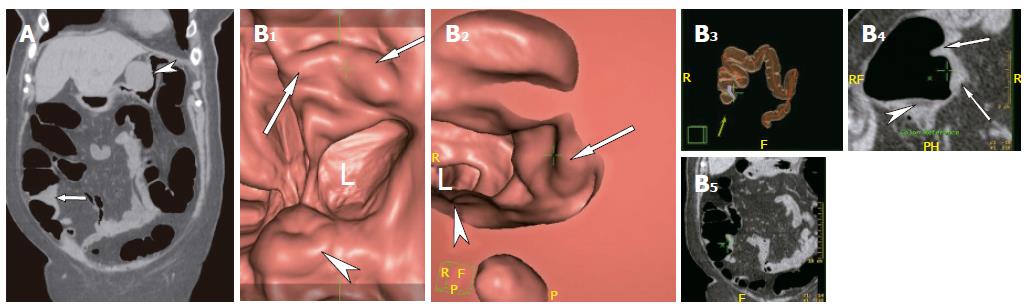
Figure 13 Fifty-eight years old male with incomplete optical colonoscopy.
A: Coronal reformat showed a mass in the medial right colon (arrow) consistent with colonic cancer. A second mass (arrowhead) showed exophytic growth from the stomach and was subsequently proven to be a gastrointestinal stromal tumor; B: Images of virtual colonoscopy showed the mass (arrows) adjacent to the ileocecal valve (arrowheads). L = colonic lumen.
- Citation: Maglinte DD, Sandrasegaran K, Tann M. Advances in alimentary tract imaging. World J Gastroenterol 2006; 12(20): 3139-3145
- URL: https://www.wjgnet.com/1007-9327/full/v12/i20/3139.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i20.3139