Published online Aug 28, 2021. doi: 10.37126/aige.v2.i4.103
Peer-review started: May 18, 2021
First decision: June 22, 2021
Revised: June 24, 2021
Accepted: August 19, 2021
Article in press: August 19, 2021
Published online: August 28, 2021
Processing time: 110 Days and 23.1 Hours
Pancreaticoduodenectomy (PD) is a complex operation accompanied by significant morbidity rates. Due to this complexity, the transition to minimally invasive PD has lagged behind other abdominal surgical operations. The safety, feasibility, favorable post-operative outcomes of robotic PD have been suggested by multiple studies. Compared to open surgery and other minimally invasive techniques such as laparoscopy, robotic PD offers satisfactory outcomes, with a non-inferior risk of adverse events. Trends of robotic PD have been on rise with centers substantially increasing the number the operation performed. Although promising, findings on robotic PD need to be corroborated in prospective trials.
Core Tip: The robotic Whipple procedure is a safe and technically feasible surgical operation. Robotic pancreaticoduodenectomy has shown favorable outcomes and is currently increasing in widespread implementation. Prospective trials are needed before this relatively new approach can be fully adopted as a standard of care in patients with pancreatic neoplasms.
- Citation: Khachfe HH, Habib JR, Chahrour MA, Nassour I. Robotic pancreaticoduodenectomy: Where do we stand? Artif Intell Gastrointest Endosc 2021; 2(4): 103-109
- URL: https://www.wjgnet.com/2689-7164/full/v2/i4/103.htm
- DOI: https://dx.doi.org/10.37126/aige.v2.i4.103
Pancreaticoduodenectomy (PD) or Whipple surgery, is a complex procedure associated with significant morbidity rates[1]. Due to the complexity of this operation, PD’s move to a more minimally invasive approach has lagged behind other general surgery procedures[2]. Gagner and Pomp[3], pioneered the laparoscopic PD (LPD) back in 1994, but LPD has not successfully transitioned into routine surgical care[3]. This is partly due to the difficulty associated with LPD in terms of expertise needed to perform the operation and the complexity of teaching the approach. In addition, the LEOPARD-2 trial demonstrated that LPD has a higher 90-d mortality as compared to the open PD (OPD). This eventually led to the discontinuation of the trial[4].
Robotic PD (RPD), which was first performed by Giulianotti et al[5], was originally described in 2001. Later in 2003, the same team published a series of 8 robotic-assisted cases[6]. The preliminary results established that RPD is both safe and feasible. Their reported mean operative time was around 8 h (490 min) in this case series.
Following these promising results, an increasing number of surgeons started utilizing the RPD approach. Different than initial reports of LPD, where some showed that LPD does not provide benefit as compared to the open approach, RPD benefits and advantages have been reported with increasing rate since its launch[7,8]. However, the “Miami International Guideline on Minimally Invasive Pancreas Resection” still does not assume minimally invasive PD is equal to OPD due to insufficient data[9].
Robotic surgery is considered a direct advancement of laparoscopy. The most widely utilized surgical system to perform RPD in specific, as well as in other operations, is the DaVinci system developed by Intuitive Surgical Incorporated[10]. The robotic system provides surgeons increased dexterity employing endo-wristed instruction, three-dimensional stereoscopic views of the surgical field, filtering of user tremors, and it provides pancreatic surgeons the capability to perform extremely complex dissections, sutures, knots and reconstructions with unparalleled precision, magnification and accuracy[11,12].
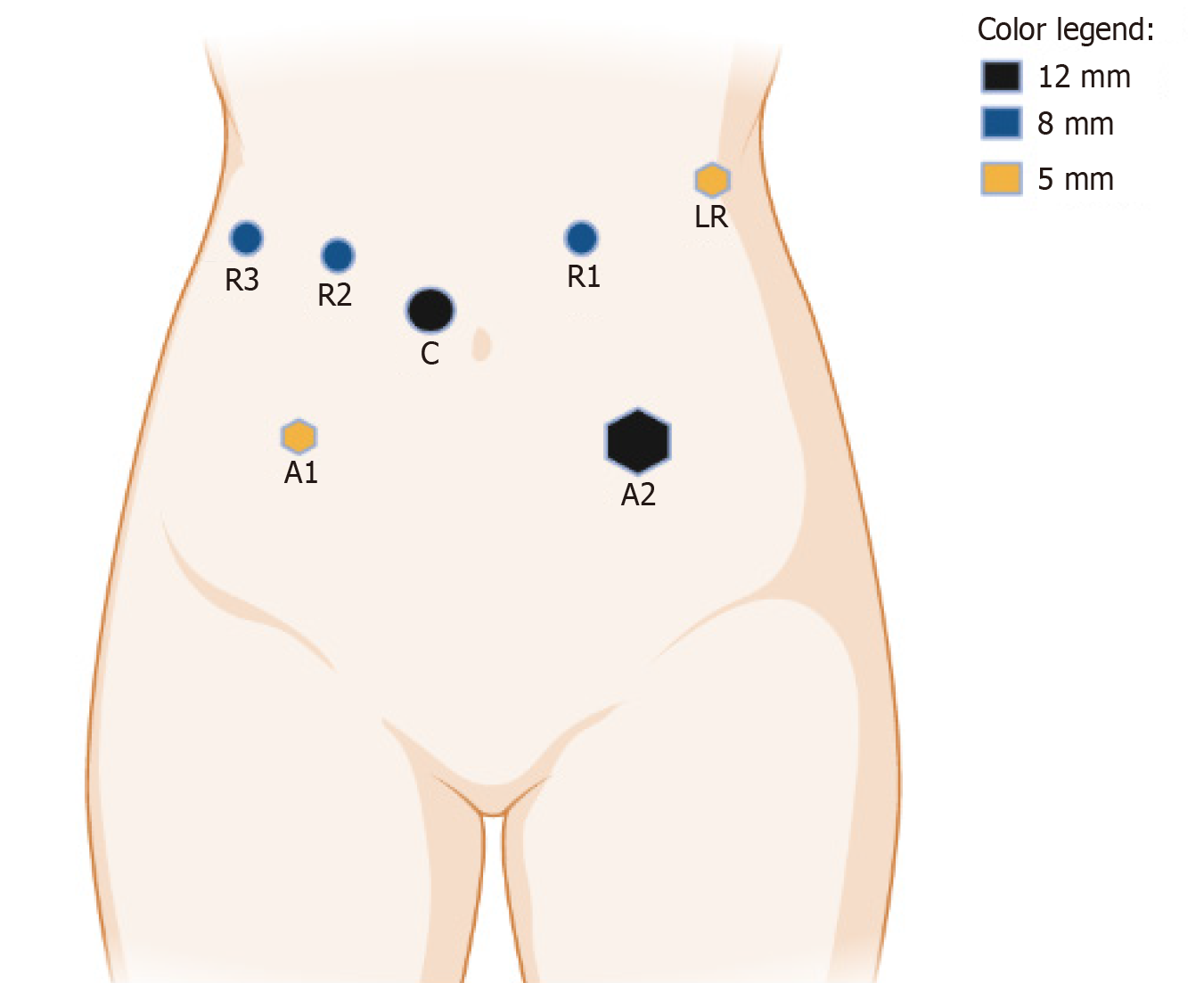
Variations in robotic Whipple techniques exist between pancreatic surgeons. While some groups undergo the operation completely robotically, other choose to use a cross laparoscopic/robotic approach. Giulianotti et al[5] support a performing the operation entirely using the robotic approach, while other groups advocate the “hybrid” approach. The hybrid or cross method entails dissecting first using laparoscopy and then performing the reconstruction part using the robot[13,14]. At the University of Pittsburgh Medical Center, the surgeons employ a robotic exclusive approach, using four robotic ports, two assistant and one retractor port as shown in Figure 1. RPD follows the same steps as Whipple’s 1935 description[15]. The gastrocolic ligament is first dissected to gain access to the lesser sac. Then, the ascending and transverse colon are mobilized. This is followed by a complete Kocher maneuver. Transection of the jejunum and the stomach (in classic Whipple) are then performed using stapling devices. Then, the porta is approached to transect the gastroduodenal artery and the hepatic duct. This is followed by transection of the pancreas at the neck and finally dissecting the uncinate of the mesenteric vessels. The reconstruction phase includes the creation of a pancreaticojejunostomy, followed by hepaticojejunostomy and finally a gastrojejunostomy. Finally, a drain is left behind and the port and extraction sites are closed.
The challenges facing the introduction of RPD are numerous. First, robotic operations are known to still have long operating time as compared to open ones. Second, due to the complexity of the robotic approach, there an increased need of training (higher learning curve) than the open and other minimally invasive techniques (laparoscopic). Third, robotic surgeries carry a high financial burden to patients, covering bodies and hospitals. This helps favor the open or laparoscopic approach for PD by insuring bodies and patients paying out-of-pocket. Fourth, RPDs require high-end infrastructure, which includes larger operating rooms, more technical staff present (in case any issues arise), and robotic certification by faculty and trainees. Finally, there is an increased difficulty in making prospective randomized trials in robotic operations. This issue arises with the decreased apparel/enrollment into robotic trials due to patient preference of open or laparoscopic approaches.
A recent study exploring the trends of the RPD for pancreatic cancers demonstrated an increasing number of RPDs over the past decade. This was accompanied by a greater reach of RPD where it may be found in community centers across the US, after being present only in a few number of academic medical facilities[16]. Robotic procedures increased from 150 operations/year to around 450 operation/year from 2010-2016[16]. This is likely owing to an increase in the number of graduates from fellowship programs that include robotic pancreas surgery as part of their curriculum, as well as greater experience and "retraining" of experienced pancreatic surgeons in the robotic approach[17-20].
Overall, the robotic method appears to enhance short-term outcomes over time. Between 2010 and 2016, there was a substantial rise in the number of lymph nodes harvested (from 18 to 21), as well as a drop in postoperative mortality (from 6.7 percent to 1.8 percent)[16]. Yan et al[21] found that as compared to open PD, RPD had considerably longer operating time, less blood loss, shorter length of stay, and reduced infection rates in a recent meta-analysis comprising 2403 patients (788 robotic and 1615 open). There was no discernible change in lymph node harvesting, reoperation, readmission rate, or death rate[21]. Another meta-analysis by Kamarajah et al[22] found that RPD had substantially lower conversion and transfusion rates than LPD, with 3462 participants (1025 robotic and 2437 Laparoscopic]. RPD had a substantially shorter hospital stay after surgery, but there was no significant difference in postoperative outcomes or R0 resection rates. Zureikat et al[23] demonstrated that RPD was linked with decreased operating time, perioperative blood loss, and postoperative pancreatic fistula development in the largest series of RPD comprising 500 robot-assisted PD. These findings were described early in the group's experience and remained low despite growing complexity of cases. Less frequent conversion to open was also noted. As for long term outcomes, Nassour et al[24] identified 17831 PD from the National Cancer Database, of which 626 were RPDs. The median overall survival did not differ between the robotic (22 mo) and open (21.8 mo) approaches. Table 1 highlights RPD findings from a variety of research. In the hands of skilled surgeons, RPD is a relatively safe procedure with excellent perioperative and postoperative results.
| Ref. | n | OR time (mean in min) | EBL (mean in mL) | Conversion (%) | R0 (%) | LN harvest (mean) | Fistula (%) | Morbidity (%) | Mortality (%) | LOS (mean in days) |
| Giulianotti et al[28], 2010 | 60 | 421 | 394 | 18.3 | 82 | 18 | 31.6 | NR | 3.3 | 22 |
| Narula et al[29], 2010 | 5 | 420 | NR | 37.5 | 100 | 16 | 0 | 0 | 0 | 9.6 |
| Zhou et al[30], 2011 | 8 | 718 | 153 | 0 | 100 | NR | 25 | NR | 0 | 16.4 |
| Lai et al[31], 2012 | 20 | 491.5 | 247 | 5 | 73.3 | 10 | 35 | 50 | 0 | 13.7 |
| Chalikonda et al[32], 2012 | 30 | 476 | 485 | 10 | 100 | 13.2 | 6.6 | 30 | 3 | 9.8 |
| Bao et al[33], 2014 | 28 | 431 | 100 | 14 | 88 | 15 | 29 | NR | 2 | 7.4 |
| Boone et al[34], 2015 | 200 | 483 | 250 | 6.5 | 92 | 22 | 17 | 67.5 | 3.3 | 9 |
| Chen et al[26], 2015 | 60 | 410 | 400 | 1.7 | 97.8 | 13.6 | 13.3 | 35 | 1.7 | 20 |
| Boggi et al[35], 2016 | 83 | 527 | NR | 1.5 | NR | 37 | 33.7 | 73.5 | 3 | 17 |
| Nassour et al[36], 2017 | 193 | 399 | NR | 11.4 | NR | NR | 20.8 | 54.9 | 1 | 8 |
| Jin et al[37], 2020 | 17 | 240 | 100 | 0 | NR | 4 | 59 | 66.4 | NR | 15 |
| Mejia et al[38], 2020 | 102 | 352 | 321 | 12.7 | 73 | 24.2 | 3.9 | 31.3 | 2.9 | 7 |
| Shi et al[39], 2020 | 187 | 279 | 297 | 3.7 | 94 | 16.6 | 10.2 | 35.6 | 2.1 | 22.4 |
| Zureikat et al[23], 2021 | 500 | 415 | 250 | 5.2 | 85 | 28 | 20.2 | 68.8 | 1.8 | 8 |
The reported learning curves for RPD are currently variable among different institutions. The University of Pittsburgh Medical center reported that 80 RPDs would be required to optimize operative time, 40 cases for an optimal pancreatic fistula rate and 20 cases to improved blood loss and conversion[25]. This was due to the that fact the surgeons at the center had no prior training, mentorship, or guidance in the technique as the robotics program was implemented in 2008. According to Chen et al[26], a comparable result can be reached after 40 RPDs. At 40 patients, Zhang et al[27] found a comparable learning curve for RPD. The learning curve may be short if adequate training and guidance is performed in surgical formative years. A formal mastery-based curriculum which integrates complex robotic procedures into practice may help in shortening the learning curve.
The future directions of RPD will likely involve the use of robotics in borderline resectable or locally advanced pancreatic lesion cases i.e. more surgically complex cases. This also includes performing complex vasculature reconstructions using the robotic approach. However, in order to develop these surgical techniques, better infrastructure, increased training, and more prospective randomized clinical trials are required. The first step needed is to prove that RPD is noninferior to the open technique in PD with level 1 evidence. This entails increasing the number of prospective trials in order to perform meta-analyses and systematic reviews. Afterwards, increased funding and training can follow, which will allow for further developments of the RPD technique discussed. Additionally, robotic training will need to be introduced and integrated early into residency programs (possibly using simulation labs) to help with the learning curve of future robotic surgeons.
Current evidence indicates that RPD is a safe and feasible procedure. The robotic approach overcomes many of technical challenges associated with the laparoscopic Whipple procedure. RPD, in the proper hands, can help patients and surgeons with periampullary lesions achieve good results. More prospective clinical trials are still needed to verify previously published retrospective research on RPD.
Manuscript source: Invited manuscript
Specialty type: Surgery
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cioffi U, Sakamoto Y S-Editor: Liu M L-Editor: A P-Editor: Wang LYT
| 1. | Cameron JL, He J. Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg. 2015;220:530-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 439] [Article Influence: 43.9] [Reference Citation Analysis (0)] |
| 2. | van Hilst J, de Rooij T, Klompmaker S, Rawashdeh M, Aleotti F, Al-Sarireh B, Alseidi A, Ateeb Z, Balzano G, Berrevoet F, Björnsson B, Boggi U, Busch OR, Butturini G, Casadei R, Del Chiaro M, Chikhladze S, Cipriani F, van Dam R, Damoli I, van Dieren S, Dokmak S, Edwin B, van Eijck C, Fabre JM, Falconi M, Farges O, Fernández-Cruz L, Forgione A, Frigerio I, Fuks D, Gavazzi F, Gayet B, Giardino A, Groot Koerkamp B, Hackert T, Hassenpflug M, Kabir I, Keck T, Khatkov I, Kusar M, Lombardo C, Marchegiani G, Marshall R, Menon KV, Montorsi M, Orville M, de Pastena M, Pietrabissa A, Poves I, Primrose J, Pugliese R, Ricci C, Roberts K, Røsok B, Sahakyan MA, Sánchez-Cabús S, Sandström P, Scovel L, Solaini L, Soonawalla Z, Souche FR, Sutcliffe RP, Tiberio GA, Tomazic A, Troisi R, Wellner U, White S, Wittel UA, Zerbi A, Bassi C, Besselink MG, Abu Hilal M; European Consortium on Minimally Invasive Pancreatic Surgery (E-MIPS). Minimally Invasive vs Open Distal Pancreatectomy for Ductal Adenocarcinoma (DIPLOMA): A Pan-European Propensity Score Matched Study. Ann Surg. 2019;269:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 196] [Article Influence: 32.7] [Reference Citation Analysis (0)] |
| 3. | Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc. 1994;8:408-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 619] [Cited by in RCA: 658] [Article Influence: 21.2] [Reference Citation Analysis (1)] |
| 4. | van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, Gerhards MF, de Hingh IH, Karsten TM, Lips DJ, Luyer MD, Busch OR, Festen S, Besselink MG; Dutch Pancreatic Cancer Group. Laparoscopic vs open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol. 2019;4:199-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 429] [Cited by in RCA: 407] [Article Influence: 67.8] [Reference Citation Analysis (0)] |
| 5. | Giulianotti PC, Mangano A, Bustos RE, Fernandes E, Masrur MA, Valle V, Gangemi A, Bianco FM. Educational step-by-step surgical video about operative technique in robotic pancreaticoduodenectomy (RPD) at University of Illinois at Chicago (UIC): 17 steps standardized technique-Lessons learned since the first worldwide RPD performed in the year 2001. Surg Endosc. 2020;34:2758-2762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, Caravaglios G. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138:777-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 749] [Cited by in RCA: 771] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 7. | Mesleh MG, Stauffer JA, Asbun HJ. Minimally invasive surgical techniques for pancreatic cancer: ready for prime time? J Hepatobiliary Pancreat Sci. 2013;20:578-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Gagner M, Pomp A. Laparoscopic pancreatic resection: Is it worthwhile? J Gastrointest Surg. 1997;1:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 158] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A, D'Angelica MI, Balduzzi A, Bassi C, Björnsson B, Boggi U, Callery MP, Del Chiaro M, Coimbra FJ, Conrad C, Cook A, Coppola A, Dervenis C, Dokmak S, Edil BH, Edwin B, Giulianotti PC, Han HS, Hansen PD, van der Heijde N, van Hilst J, Hester CA, Hogg ME, Jarufe N, Jeyarajah DR, Keck T, Kim SC, Khatkov IE, Kokudo N, Kooby DA, Korrel M, de Leon FJ, Lluis N, Lof S, Machado MA, Demartines N, Martinie JB, Merchant NB, Molenaar IQ, Moravek C, Mou YP, Nakamura M, Nealon WH, Palanivelu C, Pessaux P, Pitt HA, Polanco PM, Primrose JN, Rawashdeh A, Sanford DE, Senthilnathan P, Shrikhande SV, Stauffer JA, Takaori K, Talamonti MS, Tang CN, Vollmer CM, Wakabayashi G, Walsh RM, Wang SE, Zinner MJ, Wolfgang CL, Zureikat AH, Zwart MJ, Conlon KC, Kendrick ML, Zeh HJ, Hilal MA, Besselink MG; International Study Group on Minimally Invasive Pancreas Surgery (I-MIPS). The Miami International Evidence-based Guidelines on Minimally Invasive Pancreas Resection. Ann Surg. 2020;271:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 319] [Article Influence: 63.8] [Reference Citation Analysis (0)] |
| 10. | Kim K, Hagen ME, Buffington C. Robotics in advanced gastrointestinal surgery: the bariatric experience. Cancer J. 2013;19:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Zeh HJ 3rd, Bartlett DL, Moser AJ. Robotic-assisted major pancreatic resection. Adv Surg. 2011;45:323-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Lanfranco AR, Castellanos AE, Desai JP, Meyers WC. Robotic surgery: a current perspective. Ann Surg. 2004;239:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 761] [Cited by in RCA: 687] [Article Influence: 32.7] [Reference Citation Analysis (0)] |
| 13. | Kim BJ, Prakash L, Narula N, Davis CH, Kim MP, Aloia TA, Vauthey JN, Lee JE, Katz MH, Tzeng CD. Contemporary analysis of complications associated with biliary stents during neoadjuvant therapy for pancreatic adenocarcinoma. HPB (Oxford). 2019;21:662-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Miller-Ocuin JL, Hogg ME, Zureikat AH, Zeh Iii HJ. Robotic Approaches to the Patient with Pancreatic Adenocarcinoma. In: Case-Based Lessons in the Management of Complex Hepato-Pancreato-Biliary Surgery. Pawlik TM, Weber S, Gamblin TC, editors. Cham: Springer International Publishing, 2017: 323-337. |
| 15. | Whipple AO, Parsons WB, Mullins CR. TREATMENT OF CARCINOMA OF THE AMPULLA OF VATER. Ann Surg. 1935;102:763-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 882] [Cited by in RCA: 894] [Article Influence: 49.7] [Reference Citation Analysis (0)] |
| 16. | Hoehn RS, Nassour I, Adam MA, Winters S, Paniccia A, Zureikat AH. National Trends in Robotic Pancreas Surgery. J Gastrointest Surg. 2021;25:983-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 17. | Moekotte AL, Rawashdeh A, Asbun HJ, Coimbra FJ, Edil BH, Jarufe N, Jeyarajah DR, Kendrick ML, Pessaux P, Zeh HJ, Besselink MG, Abu Hilal M, Hogg ME; International Evidence-Based Guidelines on Minimally Invasive Pancreas Resection (IG-MIPR). Safe implementation of minimally invasive pancreas resection: a systematic review. HPB (Oxford). 2020;22:637-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 18. | Tam V, Zenati M, Novak S, Chen Y, Zureikat AH, Zeh HJ 3rd, Hogg ME. Robotic Pancreatoduodenectomy Biotissue Curriculum has Validity and Improves Technical Performance for Surgical Oncology Fellows. J Surg Educ. 2017;74:1057-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 19. | Nota CL, Zwart MJ, Fong Y, Hagendoorn J, Hogg ME, Koerkamp BG, Besselink MG, Molenaar IQ; Dutch Pancreatic Cancer Group. Developing a robotic pancreas program: the Dutch experience. J Vis Surg. 2017;3:106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Mark Knab L, Zenati MS, Khodakov A, Rice M, Al-Abbas A, Bartlett DL, Zureikat AH, Zeh HJ, Hogg ME. Evolution of a Novel Robotic Training Curriculum in a Complex General Surgical Oncology Fellowship. Ann Surg Oncol. 2018;25:3445-3452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 21. | Yan Q, Xu LB, Ren ZF, Liu C. Robotic vs open pancreaticoduodenectomy: a meta-analysis of short-term outcomes. Surg Endosc. 2020;34:501-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 22. | Kamarajah SK, Bundred J, Marc OS, Jiao LR, Manas D, Abu Hilal M, White SA. Robotic vs conventional laparoscopic pancreaticoduodenectomy a systematic review and meta-analysis. Eur J Surg Oncol. 2020;46:6-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 23. | Zureikat AH, Beane JD, Zenati MS, Al Abbas AI, Boone BA, Moser AJ, Bartlett DL, Hogg ME, Zeh HJ 3rd. 500 Minimally Invasive Robotic Pancreatoduodenectomies: One Decade of Optimizing Performance. Ann Surg. 2021;273:966-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 128] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 24. | Nassour I, Winters SB, Hoehn R, Tohme S, Adam MA, Bartlett DL, Lee KK, Paniccia A, Zureikat AH. Long-term oncologic outcomes of robotic and open pancreatectomy in a national cohort of pancreatic adenocarcinoma. J Surg Oncol. 2020;122:234-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 25. | Zureikat AH, Postlewait LM, Liu Y, Gillespie TW, Weber SM, Abbott DE, Ahmad SA, Maithel SK, Hogg ME, Zenati M, Cho CS, Salem A, Xia B, Steve J, Nguyen TK, Keshava HB, Chalikonda S, Walsh RM, Talamonti MS, Stocker SJ, Bentrem DJ, Lumpkin S, Kim HJ, Zeh HJ 3rd, Kooby DA. A Multi-institutional Comparison of Perioperative Outcomes of Robotic and Open Pancreaticoduodenectomy. Ann Surg. 2016;264:640-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 200] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 26. | Chen S, Chen JZ, Zhan Q, Deng XX, Shen BY, Peng CH, Li HW. Robot-assisted laparoscopic vs open pancreaticoduodenectomy: a prospective, matched, mid-term follow-up study. Surg Endosc. 2015;29:3698-3711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 141] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 27. | Zhang T, Zhao ZM, Gao YX, Lau WY, Liu R. The learning curve for a surgeon in robot-assisted laparoscopic pancreaticoduodenectomy: a retrospective study in a high-volume pancreatic center. Surg Endosc. 2019;33:2927-2933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 103] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 28. | Giulianotti PC, Sbrana F, Bianco FM, Elli EF, Shah G, Addeo P, Caravaglios G, Coratti A. Robot-assisted laparoscopic pancreatic surgery: single-surgeon experience. Surg Endosc. 2010;24:1646-1657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 266] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 29. | Narula VK, Mikami DJ, Melvin WS. Robotic and laparoscopic pancreaticoduodenectomy: a hybrid approach. Pancreas. 2010;39:160-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 30. | Zhou NX, Chen JZ, Liu Q, Zhang X, Wang Z, Ren S, Chen XF. Outcomes of pancreatoduodenectomy with robotic surgery vs open surgery. Int J Med Robot. 2011;7:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 31. | Lai EC, Yang GP, Tang CN. Robot-assisted laparoscopic pancreaticoduodenectomy vs open pancreaticoduodenectomy--a comparative study. Int J Surg. 2012;10:475-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 157] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 32. | Chalikonda S, Aguilar-Saavedra JR, Walsh RM. Laparoscopic robotic-assisted pancreaticoduodenectomy: a case-matched comparison with open resection. Surg Endosc. 2012;26:2397-2402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 191] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 33. | Bao PQ, Mazirka PO, Watkins KT. Retrospective comparison of robot-assisted minimally invasive vs open pancreaticoduodenectomy for periampullary neoplasms. J Gastrointest Surg. 2014;18:682-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 34. | Boone BA, Zenati M, Hogg ME, Steve J, Moser AJ, Bartlett DL, Zeh HJ, Zureikat AH. Assessment of quality outcomes for robotic pancreaticoduodenectomy: identification of the learning curve. JAMA Surg. 2015;150:416-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 235] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 35. | Boggi U, Napoli N, Costa F, Kauffmann EF, Menonna F, Iacopi S, Vistoli F, Amorese G. Robotic-Assisted Pancreatic Resections. World J Surg. 2016;40:2497-2506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 36. | Nassour I, Wang SC, Porembka MR, Yopp AC, Choti MA, Augustine MM, Polanco PM, Mansour JC, Minter RM. Robotic Versus Laparoscopic Pancreaticoduodenectomy: a NSQIP Analysis. J Gastrointest Surg. 2017;21:1784-1792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 37. | Jin JB, Qin K, Yang Y, Shi YS, Wu ZC, Deng XX, Chen H, Cheng DF, Shen BY, Peng CH. Robotic pancreatectomy for solid pseudopapillary tumors in the pancreatic head: A propensity score-matched comparison and analysis from a single center. Asian J Surg. 2020;43:354-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 38. | Mejia A, Shah J, Vivian E, Acharya P. Analysis of 102 Fully Robotic Pancreaticoduodenectomies: Clinical and Financial Outcomes. Pancreas. 2020;49:668-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 39. | Shi Y, Jin J, Qiu W, Weng Y, Wang J, Zhao S, Huo Z, Qin K, Wang Y, Chen H, Deng X, Peng C, Shen B. Short-term Outcomes After Robot-Assisted vs Open Pancreaticoduodenectomy After the Learning Curve. JAMA Surg. 2020;155:389-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 85] [Article Influence: 21.3] [Reference Citation Analysis (0)] |