Published online Oct 28, 2020. doi: 10.13105/wjma.v8.i5.400
Peer-review started: May 27, 2020
First decision: September 14, 2020
Revised: October 9, 2020
Accepted: October 27, 2020
Article in press: October 27, 2020
Published online: October 28, 2020
Processing time: 154 Days and 5.7 Hours
Type 2 diabetes mellitus (T2DM) causes both macrovascular and microvascular complications. However, currently, selection of glycemic measures and their thresholds to diagnose T2DM, and efficacy outcomes in evaluation of anti-diabetic drugs is predominantly informed by the relation of T2DM to microvascular complications. We can be severely mistaken on T2DM by neglecting macrovascular complications which are generally more severe, if they also occur more commonly than microvascular complications.
To compare the incidence of major cardiovascular events (MACEs) and severe microvascular complications (SMICs) in T2DM patients.
MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials were searched from inception to September 2017. Cohort studies or trials of T2DM patients aged 18 years or older that reported incidence of both MACEs and SMICs were included. MACEs were defined as nonfatal myocardial infarction and stroke, and cardiovascular death, while SMICs included serious retinopathy, nephropathy and diabetic disorder. The relative risk (RR) was estimated as the incidence of MACEs divided by that of SMICs in same patients and combined with meta-analysis in a random-effect model.
Twelve studies with a total of 16 cohorts and 387376 patients were included, and the combined RR was 2.02 (95%CI: 1.46–2.79). The higher incidence of MACEs remained in various subgroup and sensitivity analyses.
Patients with T2DM are much more likely to develop MACEs than SMICs. By taking more serious consequences and relatively higher incidence into consideration, macrovascular complications deserve more emphasis in developing the diagnostic criteria of T2DM and in evaluating the efficacy of anti-diabetic drugs.
Core Tip: Microvascular complications currently predominate the definition and treatment evaluation of type 2 diabetes mellitus (T2DM). We can be severely mistaken by neglecting macrovascular complications which are generally more severe, if they also occur more commonly than microvascular complications. This systematic review and meta-analysis shows that major cardiovascular events are twice as common as severe microvascular complications in T2DM patients, suggesting that macrovascular complications should be emphasized over microvascular complications in developing the diagnostic criteria of T2DM and in evaluating the efficacy of anti-diabetic drugs.
- Citation: Zhu YY, Yang ZY, Li P, Huang XY, Zhang XH, Ji LN, Tang JL. Comparing the incidence of major cardiovascular events and severe microvascular complications in patients with type 2 diabetes mellitus: A systematic review and meta-analysis . World J Meta-Anal 2020; 8(5): 400-410
- URL: https://www.wjgnet.com/2308-3840/full/v8/i5/400.htm
- DOI: https://dx.doi.org/10.13105/wjma.v8.i5.400
Since 1980, the number of patients with diabetes mellitus has nearly quadrupled to 422 million in 2014 worldwide[1]. Type 2 diabetes mellitus (T2DM), accounting for over 90% of all diabetes cases, can cause both macrovascular (mainly cardiovascular disease) and microvascular (e.g., retinopathy, neuropathy, diabetic foot) complications[2,3]. Hyperglycemia causes microvascular complications by activating the protein kinase C, resulting in abnormal microvasculature characterized by endothelial dysfunction, smooth muscle cell proliferation, increased vascular permeability and angiogenesis[4,5]. In addition, oxidative stress, advanced glycation end products and chronic low-grade inflammation also play important roles in the pathogenesis[6-8]. Microvascular complications are not limited to those occurring in the retina, kidneys, and nerves, but may also affect other organs[9]. For example, diabetes mellitus can cause coronary microvascular dysfunction, which reduces the coronary flow serve and leads to the failure of a normal functioning microvasculature[10].
Despite the potential damage to multiple organs caused by microvascular complications, they are generally less serious than macrovascular complications in terms of the number of deaths, health care cost and decreased quality of life they cause in T2DM patients[11-13]. However, for some historical reasons, macrovascular complications have been less considered in developing the definition of T2DM (e.g., which glycemic measures and which diagnostic thresholds to use) which is largely dominated by concerns about microvascular complications, in particular retinopathy[14-17].
Moreover, the efficacy of anti-diabetic drugs is also evaluated according to their effects on microvascular complications[18]. Macrovascular complications, if included, are often considered as safety indicators or adverse effects of anti-diabetic drugs[19,20]. However, it is indeed observed that some glucose-lowering drugs which can reduce the risk of microvascular complications increase the risk of macrovascular complications in T2DM patients[21,22]. Consequently, trials based only on microvascular complications could mistakenly endorse drugs that can reduce microvascular complications at the cost of increasing macrovascular complications.
If severe macrovascular complications occur as commonly as or more commonly than severe microvascular complications (SMICs) in patients with T2DM, the diagnostic criteria, evaluation of anti-diabetic drugs and practice guidelines may have to be reviewed by considering more about macrovascular complications. We thus conducted this systematic review and meta-analysis to compare the incidence of major cardiovascular events (MACEs) and SMICs in T2DM patients.
This systematic review and meta-analysis summarized direct comparisons of the incidence of MACEs with that of SMICs in the same patients with T2DM in cohort studies or clinical trials. The PRISMA guidelines were followed in this review[23]. This review has not been registered.
We searched MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials from inception to September 2017, with no language restriction. Terms for cardiovascular disease, microvascular disease, T2DM, and study design (cohort and trials) were used to identify potentially relevant studies. Detailed search strategies are included in Supplementary Tables 1 and 2. We also manually reviewed the reference lists of eligible articles and important reviews on the topic to look for additional studies.
After initial scan of titles and abstracts of cohort studies and trials, full-texts of potentially included studies were further reviewed for their eligibility. A study was deemed eligible if its sample size was > 1000, included patients with T2DM aged ≥ 18 years, and reported absolute number of cases or incidence for both MACEs and SMICs. Although one thousand is an arbitrary cutoff, studies with fewer than 1000 participants would have too few microvascular events to allow for reliable estimation of the incidence of SMICs and add little to the included studies. These studies were thus excluded. We also excluded studies conducted in special subgroups of diabetic patients, such as those wholly with cancer or cardiovascular disease and those receiving dialysis at baseline.
In this systematic review, no matter for the MACEs and SMICs, we included the mainly serious types of macrovascular and microvascular complications respectively. MACEs were generally defined as nonfatal myocardial infarction and stroke, and cardiovascular death. SMICs, for which there was no standardized definition, were defined as serious retinopathy, nephropathy, and foot disorder. The reason for choosing these complications as SMICs was that they represented three serious types of microvascular complications, which have the equal severity with MACEs. Serious retinopathy included severe loss of vision, blindness, or laser therapy for retinopathy[24-26]. Serious nephropathy included renal failure, dialysis, end-stage renal disease or renal death[27]. Serious foot disorder included limb amputation or death from peripheral artery disease[3]. Noticeably, by taking retinopathy which requires laser therapy and amputation as SMICs, we slightly over-estimated the incidence of SMICs, which could lead to a more conservative estimate of the risk of MACEs relative to SMICs.
It takes a long time to have all these complications occur in T2DM patients and some studies may have no event for some complications, particularly for severe microvascular ones. Thus, we also included studies that lacked data on only one type of event just to ensure having enough eligible studies in this review.
Study selection was completed independently by three researchers (Zhu YY, Li P, Huang XY). The disagreements were settled by discussions with a more experienced reviewer (Yang ZY).
The following data were extracted from each eligible study: Bibliographic information (e.g., first author, publication year, study location), baseline characteristics (e.g., number of participants, mean age, sex, and diabetes duration), length of follow-up and outcomes including information on definition of MACEs and SMICs, number of people at risk, number or cumulative incidence of each outcome event).
For multiple reports of the same study, we extracted data from the report with relatively longer follow-up and more complete information. For clinical trials, data in the intervention and control groups were extracted separately and considered as two separate cohorts in the data analysis.
Data extraction was completed by three researchers (Zhu YY, Li P, Huang XY). This process was double-checked by another reviewer (Yang ZY). The disagreements were settled by discussion.
Methodological quality of included studies was assessed by Zhu YY, using a 5-item scale adapted from the Institute of Health Economics and the Newcastle–Ottawa Quality Assessment Scale (Supplementary Table 3)[28,29]. The scale evaluated each study based on the population (1 items), outcome measurement (1 item), results (2 item), competing interests and source of support (1 item). For each assessed study, 1 point was assigned to each item if the criterion was met, and a score of 3.5 or more suggests high quality.
In each study, the incidence was estimated as the number of MACEs and SMICs divided by the number of participants at risk respectively. Because some studies reported different numbers of people at risk for different types of SMICs or MACEs, the smallest number of people at risk for SMICs was used as denominator, and the largest was used for MACEs in order to avoid over-estimation of the macrovascular over microvascular complication ratio. In occasions where data on a particular type of MACEs or SMICs was missing, the average incidence estimated from all other studies was used to make it up in the analyses.
In each study, the relative risk (RR) was the ratio of the incidence of MACEs over that of SMICs. The random effect model was used in meta-analysis to estimate the overall RR and its 95%CI. Heterogeneity was evaluated using Cochran’s Q test and I2 statistics[30]. Heterogeneity was judged present if the P value ≤ 0.10 for Cochran’s Q or an I2 statistic ≥ 50%. Begg’s funnel plot and Egger’s test were used to test the potential publication bias[31]. Previous studies have found age, follow-up time, and diabetes duration are associated with macrovascular and microvascular events in patients with T2DM[32]. Besides, different types of study (cohort vs trial) were included in our review. In theory, the drugs tested in trials may affect the incidence of complications, thus affecting the risk ratio (although the result of subgroup analysis showed no significant difference). Therefore, subgroup analyses were conducted according to study design, age at baseline, follow-up period, duration of diabetes to investigate the potential sources of heterogeneity. We planned to do the multivariate meta-regression analysis incorporating all factors mentioned above, but did not actually do it because of the limited number of eligible studies (< 10 times the numbers of factors) as recommended by Cochrane Handbook.
Sensitivity analyses were conducted by excluding studies with missing data on a particular type of SMICs, by excluding those including laser photocoagulation therapy as serious retinopathy, and by combining the data in intervention and control groups from a trial into one cohort rather than taking them as two. A two-tailed significance level of 0.05 was used for all the statistical tests, except for Q tests of heterogeneity for which 0.10 was used. Analyses were performed using RevMan 5.3 and STATA 14. The statistical methods of this study were reviewed by Dr. Jean H. Kim from the Chinese University of Hong Kong.
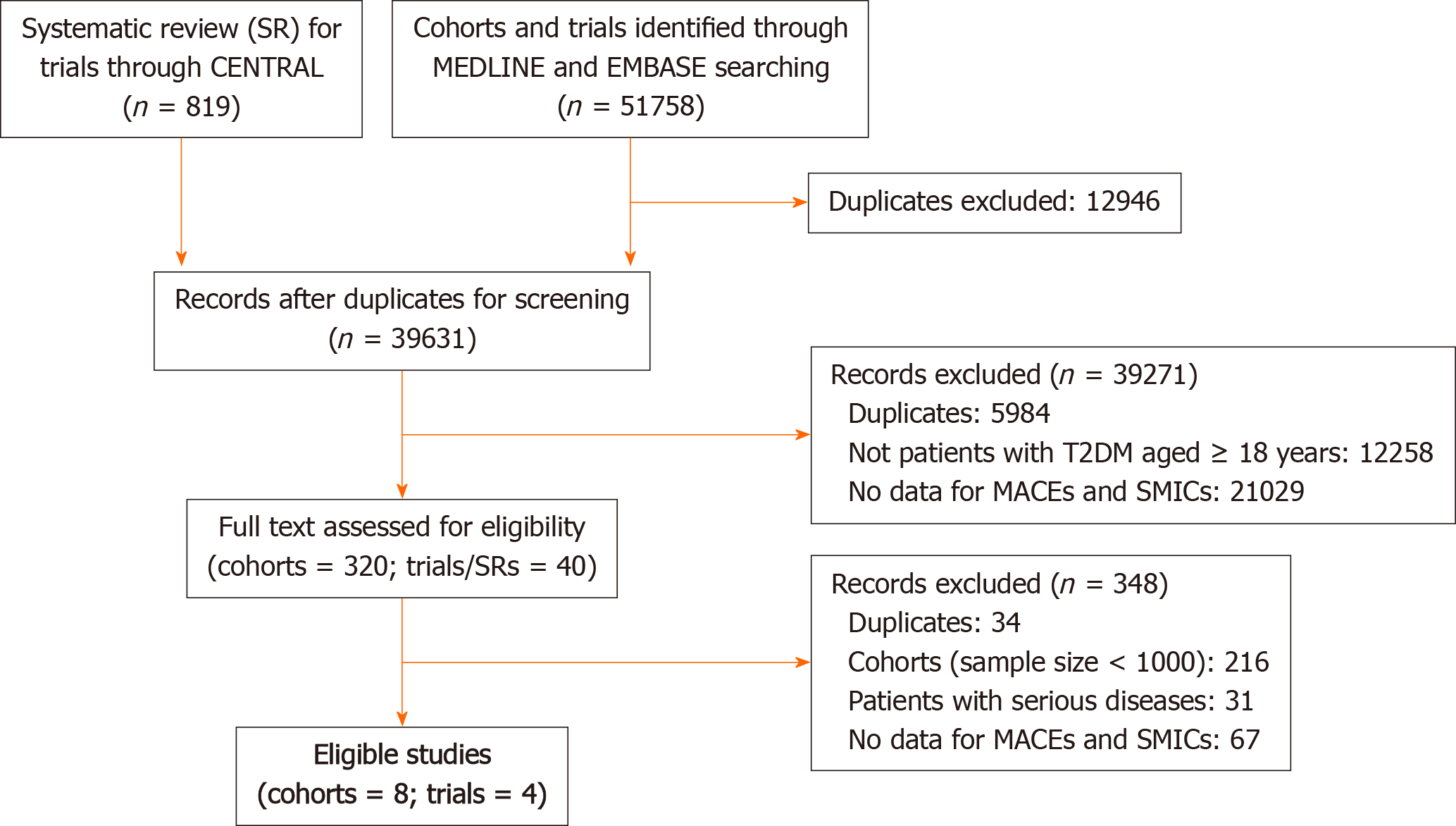
We identified a total of 52577 references from the electronic databases. Figure 1 shows the flow chart of selection process. Finally, 12 studies (eight cohort studies[33-40] and four clinical trials[41-45]) were eligible for this review. The incidence of MACEs and that of SMICs in the ACCORD study were extracted from two different papers[42,43].
The characteristics of the included studies are summarized in Table 1. Among four clinical trials, three (ACCORD[43], ADVANCE[45], and VADT[41]) were conducted to assess the effect of the intensive glucose lowering treatment (vs standard treatment) and Marre et al[44] study for the effect of ramipril (vs placebo) on macrovascular and microvascular complications. Totally, 387376 patients with T2DM (50% males) were included in this review. The patients had a mean age of 61 (range: 51-74) years old, mean duration of diabetes of 6 (range: 0-11.5) years, and mean HbA1c level of 8.4% (range: 7.5%-10.2%). The patients were followed up for a mean duration of 6.6 (range: 1.6-19) years. The details about definitions and numbers of MACEs and SMICs reported in each eligible study are shown in Supplementary Tables 4 and 5 separately. In the 12 eligible studies, two studies (ACCORD[43] and ADVANCE[45]) did not report data on serious diabetic foot and one (Kanaya et al[38]) on serious retinopathy. No missing data were found on MACEs.
| Characteristics | ACCORD[42,43] | ADVANCE[45] | Bethel et al[33], 2007 | Cheng et al[35], 2015 | Gordon et al[36], 2017 | Hansen et al[34], 2013 | Johnson et al[37], 2013 | Kanaya et al[38], 2011 | Leal et al[39], 2013 | Marre et al[44], 2004 | Martin et al[40], 2007 | VADT[41] |
| Study design | Trial | Trial | Cohort | Cohort | Cohort | Cohort | Cohort | Cohort | Cohort | Trial | Cohort | Trial |
| Treatment | Intensive vs Standard | Intensive vs Standard | / | / | / | / | / | / | / | Ramipril vs Placebo | Intensive vs Standard | |
| Country/Territory | USA | Multiple | USA | Taiwan | UK | Denmark | USA | USA | UK | Multiple | German | USA |
| No. of Participants | 10251 | 11140 | 33772 | 226310 | 10484 | 1381 | 15951 | 64211 | 4031 | 4912 | 3142 | 1791 |
| Female (%) | 39 | 42 | 58 | 51 | 46 | 47 | 59 | 47 | 43 | 30 | 51 | 3 |
| Age (yr) | 62 | 66 | 74 | 59 | 73 | 65 | 51 | 60 | 62 | 65 | 63 | 60 |
| BMI (kg/m2) | 32 | 28 | - | 25.8 | 31 | - | - | - | 29 | - | 30 | 31 |
| Diabetes duration (yr) | 10 | 7 | 0 | 5.6 | 6.0 | 0 | - | 9.8 | 11 | 9.8 | 0 | 11.5 |
| Length of follow-up (yr) | 3.5 | 5 | 10 | 6.7 | 2.4 | 19 | 1.6 | 7.2 | 8.41 | 3.9 | 6.5 | 5.6 |
| Current smoking (%) | 14 | 14 | - | - | 14 | 35 | 26 | 12 | 20 | 15 | - | 17 |
| Drinking alcohol (%) | - | - | - | - | - | - | - | - | - | 46 | - | - |
| FPG (mmol/L) | 9.7 | 8.5 | - | - | - | 13.7 | - | - | - | 9.8 | 9.2 | 11.4 |
| HbA1c (%) | 8.3 | 7.5 | - | 8.5 | 8.25 | 10.2 | - | - | 8.2 | 7.8 | 7.6 | 9.4 |
| SBP (mmHg) | 136 | 145 | - | 134 | 136 | 148 | - | - | 139 | 145 | 149 | 132 |
| DBP (mmHg) | 75 | 81 | - | 80 | 75 | 85 | - | - | - | 82 | 87 | 76 |
| Prevalence of MaC (%)1 | 35 | 32 | 0.88 | 0 | 12.5 | - | 15 | - | 6.4 | 10.2 | 22.4 | 40 |
| Prevalence of MiC (%)1 | 39 | 10 | 0.78 | 0 | 13.5 | 33 | 17 | 14 | 3.6 | 73.8 | - | 8 |
Among the 12 eligible studies, participants from five studies (Bethel et al[33], Cheng et al[35], Hansen et al[34], Kanaya et al[38], and Martin et al[40]) were considered representative of the general patients with T2DM. Except Cheng et al[35]’s study, all studies did not exclude those with known macrovascular or microvascular complications at baseline. The studies’ scores ranging from two to five. As a result, six studies[33-35,38,41,43] were considered methodologically as high quality (≥ 3.5). Detailed results are shown in Supplementary Table 6.
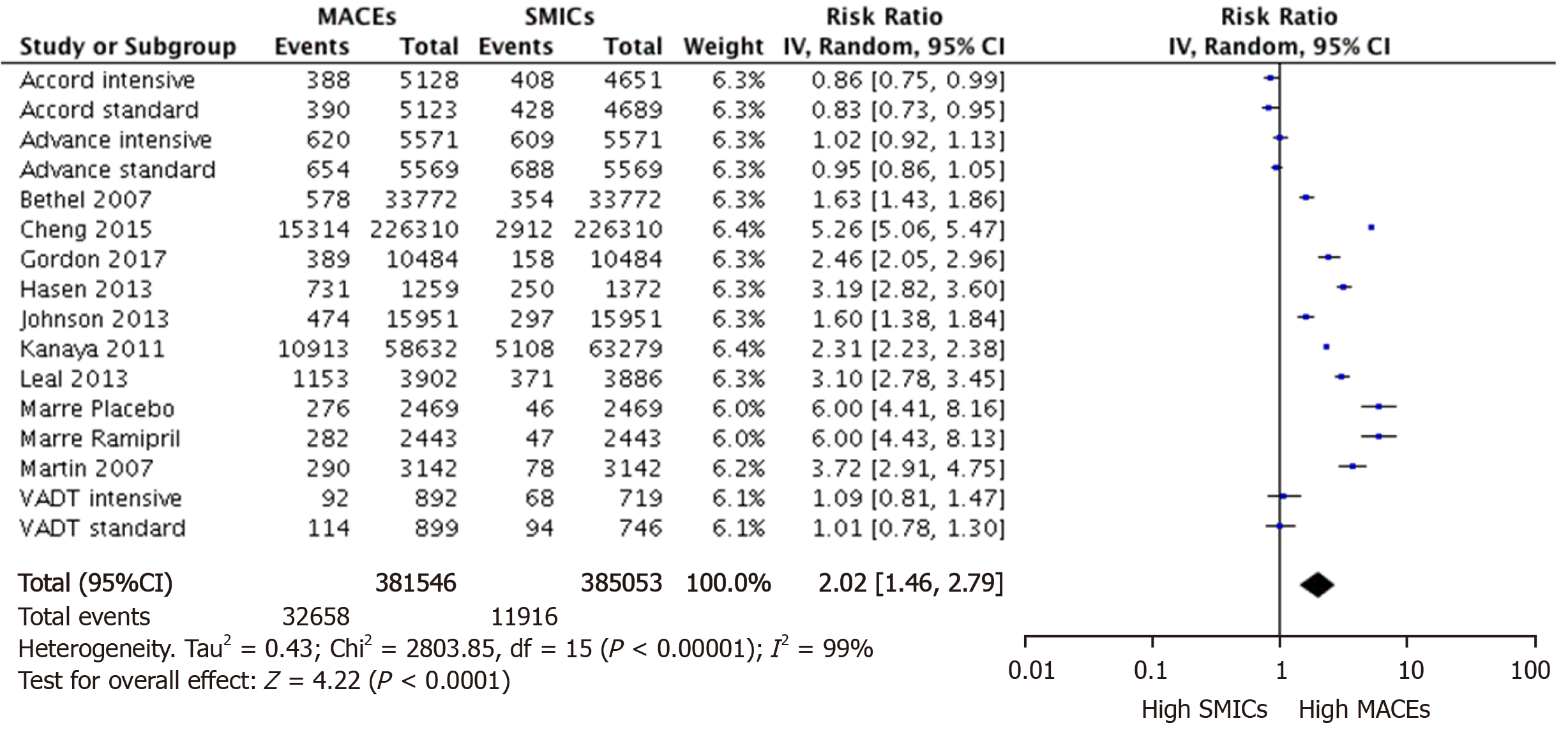
Incidence data from the intervention and control arms of clinical trials were considered as two separate cohorts in the data analysis. Therefore, 16 cohorts (eight cohort studies plus eight cohorts from four clinical trials) were finally included in the meta-analyses. Figure 2 summarizes the incidence of MACEs relative to that of SMICs in patients with T2DM in each cohort. The pooled RR for all 16 cohorts is 2.02 (95%CI: 1.46–2.79). Substantial heterogeneity was found (I2 = 99%). The funnel plot (Supplementary Figure 1) was visually and statistically symmetrical (Egger’s test
| Subgroup | Relative risk | 95%CI | I2 (%) | P difference |
| Age (yr) | 0 | 0.45 | ||
| < 65 | 1.83 | 1.17-2.84 | ||
| ≥ 65 | 2.34 | 1.46-3.75 | ||
| Study design | 80.3 | 0.02 | ||
| Cohort | 2.67 | 1.84-3.87 | ||
| Trial | 1.48 | 1.04-2.11 | ||
| Length of follow-up (yr) | 3.1 | 0.31 | ||
| ≤ 5 | 1.74 | 1.19-2.53 | ||
| > 5 | 2.30 | 1.56-3.39 | ||
| Diabetes duration (yr) | 0 | 0.75 | ||
| ≤ 9 | 2.19 | 1.46-2.87 | ||
| > 9 | 1.93 | 1.27-2.91 |
The RRs became even larger in all sensitivity analyses. After excluding five cohorts from three studies (Kanaya et al[38], ACCORD[43], and ADVANCE[45]) that had missing data on a particular type of SMICs, the combined RR was even larger and remained statistically significant (RR = 2.66, 95%CI: 1.85-3.81). As anticipated, the RR was also increased considerably (RR = 2.26, 95%CI: 1.67-3.06) after excluding six cohorts from four studies (Cheng et al[35], Hansen et al[34], VADT[41], and ADVANCE[45]) that included laser photocoagulation as severe retinopathy. Besides, combining the intervention and control cohorts in each trial[41-45] into one cohort also made the combined RR larger (RR = 2.22, 95%CI: 1.53-3.24).
We identified 16 eligible cohorts and the combined result showed that in patients with T2DM, MACEs occurred twice as commonly as SMICs. Qualitatively, the conclusion remained consistent regardless of age, study design, length of follow-up, and duration of diabetes.
Quantitatively, the relative risk differed considerably according to study design. The summarized RR was much lower in the clinical trials than in cohort studies. This may be partly attributed to the use of a much broader definition of SMICs by including laser photocoagulation as serious retinopathy in the two of these four trials (VADT[41] and ADVANCE[45]). T2DM patients with mild-to-moderate retinopathy are recommended laser photocoagulation therapy to relieve the symptoms and delay or prevent vision loss, suggesting majority of patients taking laser therapy in these trials did not have severe retinopathy[46]. In addition, the number of T2DM patients receiving laser therapy in the same trials is 2-3 times more than that in those who developed severe vision loss or blindness[33,39,47]. Therefore, including laser photocoagulation as serious retinopathy in these two trials may partly explain why trials are more likely to report a lower RR.
Meanwhile, clinical trials, like ACCORD and ADVANCE, usually set the follow-up frequency as every 1 or 2 months, while patients in cohort studies were visited every 1 or 2 years, or even longer. Thus, another possible reason for the difference between cohort studies and clinical trials is the intensive follow-up and rigorous examination in clinical trials which may detect more SMICs outcomes in clinical trials than in cohort studies. Noticeably, even though its summarized RR is relatively smaller, the conclusion remains consistent in clinical trials that MACEs occur more often than SMICs in T2DM patients.
Previous meta-analysis has shown that the risk of MACEs was more than doubled in diabetic patients than in non-diabetic people[48]. Meanwhile, our meta-analysis showed that the incidence of MACEs was two times that of SMICs in diabetic patients. Based on these information, it can be inferred that in a given population the absolute number of MACEs attributable to diabetes is greater than that of SMICs, even if the attributable risk for SMICs is 100%. The difference would be bigger if deaths caused by MACEs were compared with those by SMICs.
Therefore, the findings of this study have important implications regarding T2DM by taking the severity and frequency of complications into consideration. First, macrovascular complications should be given a greater weight than microvascular complications in developing or modifying the diagnostic criteria for T2DM. For example, is the relation between blood glycemic measures and the risk of macrovascular complications similar to that for microvascular complications? Do they suggest the same cutoff values for diagnosing diabetes? Further investigations are thus entailed to address these questions.
Second, our findings also suggest that macrovascular complications should be also considered in the evaluation of the efficacy of anti-diabetic drugs in patients with T2DM. Currently, microvascular complications are frequently used in quantifying the effect of glucose-lowering drugs, while macrovascular complications that are more common as shown in this study and more severe than microvascular complications are sometimes not considered. There is even evidence that some anti-diabetic drugs can reduce the risk of microvascular complications but at the same time show no effect or even increase the risk of macrovascular complications[18,21,22]. Our study suggests that it is time to review the current practice in the evaluation of glucose-lowering drugs in which macrovascular complications should be used as the primary outcome for quantifying the benefit of the drugs.
There are some limitations in this systematic review. First, participants in trials and some cohort studies may not fully represent the general population of those with T2DM. But we have not found any good reasons that more representative populations would have a smaller difference between the two types of vascular complications. Second, a fraction of T2DM patients in this review already have microvascular or macrovascular complications at baseline and could not be excluded in analysis, which may bias the comparison but is unlikely to qualitatively reverse the risk ratio between these two types of complications[49,50].
Patients with T2DM are much more likely to develop MACEs than SMICs. This suggests by taking more serious consequences and higher incidence into consideration, macrovascular complications deserve more emphasis in developing the diagnostic criteria of type 2 diabetes mellitus and in evaluating the efficacy of anti-diabetic drugs.
Type 2 diabetes mellitus (T2DM) causes both macrovascular and microvascular complications. However, currently, selection of glycemic measures and their thresholds to diagnose T2DM, and efficacy outcomes in evaluation of anti-diabetic drugs is predominantly informed by the relation of T2DM to microvascular complications.
We can be severely mistaken by neglecting macrovascular complications in developing the diagnostic criteria of T2DM and in evaluating the efficacy of anti-diabetic drugs if they also occur more commonly than microvascular complications.
This study aimed to compare the incidence of major cardiovascular events (MACEs) and severe microvascular complications (SMICs) in the same T2DM patients.
The systematic review and meta-analysis with a random-effect model were conducted to combine the relative risk (RR) estimated as the incidence of MACEs divided by that of SMICs in the same T2DM patients of eligible cohort studies or trials.
Twelve studies with a total of 16 cohorts and 387376 patients were included, and the combined RR was 2.02 (95%CI: 1.46–2.79). The higher incidence of MACEs remained in various subgroup and sensitivity analyses.
Patients with T2DM are much more likely to develop MACEs than SMICs.
With their severity and incidence taken into consideration, macrovascular complications deserve more emphasis in developing the diagnostic criteria of T2DM and in evaluating the efficacy of anti-diabetic drugs.
Manuscript source: Unsolicited manuscript
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Manenti A, Schuurman H S-Editor: Wang JL L-Editor: A P-Editor: Li JH
| 1. | World Health Organization. Global report on diabetes. Available from: https://www.who.int/diabetes/publications/grd-2016/en/. |
| 2. | Cade WT. Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther. 2008;88:1322-1335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 733] [Cited by in RCA: 640] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 3. | Volmer-Thole M, Lobmann R. Neuropathy and Diabetic Foot Syndrome. Int J Mol Sci. 2016;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 216] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 4. | Simran, Grewal AK, Arora S, Singh TG. Role of protein kinase C in diabetic complications. J Pharm Tech Res Manag. 2019;7:87-95. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Park S, Kang HJ, Jeon JH, Kim MJ, Lee IK. Recent advances in the pathogenesis of microvascular complications in diabetes. Arch Pharm Res. 2019;42:252-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 6. | Calderon GD, Juarez OH, Hernandez GE, Punzo SM, De la Cruz ZD. Oxidative stress and diabetic retinopathy: development and treatment. Eye (Lond). 2017;31:1122-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 176] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 7. | Domingueti CP, Dusse LM, Carvalho Md, de Sousa LP, Gomes KB, Fernandes AP. Diabetes mellitus: The linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J Diabetes Complications. 2016;30:738-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 455] [Article Influence: 50.6] [Reference Citation Analysis (0)] |
| 8. | Rhee SY, Kim YS. The Role of Advanced Glycation End Products in Diabetic Vascular Complications. Diabetes Metab J. 2018. [PubMed] |
| 9. | Mauricio D, Alonso N, Gratacòs M. Chronic Diabetes Complications: The Need to Move beyond Classical Concepts. Trends Endocrinol Metab. 2020;31:287-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 90] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 10. | Kibel A, Selthofer-Relatic K, Drenjancevic I, Bacun T, Bosnjak I, Kibel D, Gros M. Coronary microvascular dysfunction in diabetes mellitus. J Int Med Res. 2017;45:1901-1929. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 11. | Collier A, Meney C, Hair M, Cameron L, Boyle JG. Cancer has overtaken cardiovascular disease as the commonest cause of death in Scottish type 2 diabetes patients: A population-based study (The Ayrshire Diabetes Follow-up Cohort study). J Diabetes Investig. 2020;11:55-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Pham TB, Nguyen TT, Truong HT, Trinh CH, Du HNT, Ngo TT, Nguyen LH. Effects of Diabetic Complications on Health-Related Quality of Life Impairment in Vietnamese Patients with Type 2 Diabetes. J Diabetes Res. 2020;2020:4360804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 13. | Zhuo X, Zhang P, Hoerger TJ. Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am J Prev Med. 2013;45:253-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 172] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 14. | Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 115] [Reference Citation Analysis (0)] |
| 15. | Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26 Suppl 1:S5-S20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1635] [Cited by in RCA: 2108] [Article Influence: 95.8] [Reference Citation Analysis (0)] |
| 16. | International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32:1327-1334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2247] [Cited by in RCA: 2209] [Article Influence: 138.1] [Reference Citation Analysis (1)] |
| 17. | World Health Organization. Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus: Abbreviated Report of a WHO Consultation. Geneva: World Health Organization, 2011. [PubMed] |
| 18. | Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M, Lafont S, Bergeonneau C, Kassaï B, Erpeldinger S, Wright JM, Gueyffier F, Cornu C. Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ. 2011;343:d4169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 524] [Cited by in RCA: 502] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 19. | Smith RJ, Goldfine AB, Hiatt WR. Evaluating the Cardiovascular Safety of New Medications for Type 2 Diabetes: Time to Reassess? Diabetes Care. 2016;39:738-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 20. | Xu J, Rajaratnam R. Cardiovascular safety of non-insulin pharmacotherapy for type 2 diabetes. Cardiovasc Diabetol. 2017;16:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 21. | Li L, Li S, Deng K, Liu J, Vandvik PO, Zhao P, Zhang L, Shen J, Bala MM, Sohani ZN, Wong E, Busse JW, Ebrahim S, Malaga G, Rios LP, Wang Y, Chen Q, Guyatt GH, Sun X. Dipeptidyl peptidase-4 inhibitors and risk of heart failure in type 2 diabetes: systematic review and meta-analysis of randomised and observational studies. BMJ. 2016;352:i610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 184] [Cited by in RCA: 175] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 22. | Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB, Cavender MA, Udell JA, Desai NR, Mosenzon O, McGuire DK, Ray KK, Leiter LA, Raz I; SAVOR-TIMI 53 Steering Committee and Investigators. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317-1326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2804] [Cited by in RCA: 2580] [Article Influence: 215.0] [Reference Citation Analysis (0)] |
| 23. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13930] [Cited by in RCA: 13335] [Article Influence: 833.4] [Reference Citation Analysis (0)] |
| 24. | Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B; American College of Cardiology; American Heart Association Task Force on Practice Guidelines; American College of Chest Physicians; International Society for Heart and Lung Transplantation; Heart Rhythm Society. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112:e154-e235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1366] [Cited by in RCA: 1530] [Article Influence: 76.5] [Reference Citation Analysis (0)] |
| 25. | Mistry H, Auguste P, Lois N, Waugh N. Diabetic retinopathy and the use of laser photocoagulation: is it cost-effective to treat early? BMJ Open Ophthalmol. 2017;2:e000021. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Ringborg A, Yin DD, Martinell M, Stålhammar J, Lindgren P. The impact of acute myocardial infarction and stroke on health care costs in patients with type 2 diabetes in Sweden. Eur J Cardiovasc Prev Rehabil. 2009;16:576-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Mogensen CE, Christensen CK, Vittinghus E. The stages in diabetic renal disease. With emphasis on the stage of incipient diabetic nephropathy. Diabetes. 1983;32 Suppl 2:64-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 557] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 28. | Moga C, Guo B, Schopflocher D, Harstall C. Development of a quality appraisal tool for case series studies using a modified Delphi technique. Edmonton: Institute of Health Economics, 2012. |
| 29. | Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. |
| 30. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46435] [Article Influence: 2110.7] [Reference Citation Analysis (3)] |
| 31. | Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34245] [Cited by in RCA: 40440] [Article Influence: 1444.3] [Reference Citation Analysis (2)] |
| 32. | Zoungas S, Woodward M, Li Q, Cooper ME, Hamet P, Harrap S, Heller S, Marre M, Patel A, Poulter N, Williams B, Chalmers J; ADVANCE Collaborative group. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia. 2014;57:2465-2474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 332] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 33. | Bethel MA, Sloan FA, Belsky D, Feinglos MN. Longitudinal incidence and prevalence of adverse outcomes of diabetes mellitus in elderly patients. Arch Intern Med. 2007;167:921-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 100] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 34. | Hansen LJ, Siersma V, Beck-Nielsen H, de Fine Olivarius N. Structured personal care of type 2 diabetes: a 19 year follow-up of the study Diabetes Care in General Practice (DCGP). Diabetologia. 2013;56:1243-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Cheng LJ, Chen JH, Lin MY, Chen LC, Lao CH, Luh H, Hwang SJ. A competing risk analysis of sequential complication development in Asian type 2 diabetes mellitus patients. Sci Rep. 2015;5:15687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 36. | Gordon J, McEwan P, Evans M, Puelles J, Sinclair A. Managing glycaemia in older people with type 2 diabetes: A retrospective, primary care-based cohort study, with economic assessment of patient outcomes. Diabetes Obes Metab. 2017;19:644-653. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 37. | Johnson BL, Blackhurst DW, Latham BB, Cull DL, Bour ES, Oliver TL, Williams B, Taylor SM, Scott JD. Bariatric surgery is associated with a reduction in major macrovascular and microvascular complications in moderately to severely obese patients with type 2 diabetes mellitus. J Am Coll Surg. 2013;216:545-56; discussion 556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 38. | Kanaya AM, Adler N, Moffet HH, Liu J, Schillinger D, Adams A, Ahmed AT, Karter AJ. Heterogeneity of diabetes outcomes among asians and pacific islanders in the US: the diabetes study of northern california (DISTANCE). Diabetes Care. 2011;34:930-937. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 39. | Leal J, Hayes AJ, Gray AM, Holman RR, Clarke PM. Temporal validation of the UKPDS outcomes model using 10-year posttrial monitoring data. Diabetes Care. 2013;36:1541-1546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 40. | Martin S, Schramm W, Schneider B, Neeser K, Weber C, Lodwig V, Heinemann L, Scherbaum WA, Kolb H. Epidemiology of complications and total treatment costs from diagnosis of Type 2 diabetes in Germany (ROSSO 4). Exp Clin Endocrinol Diabetes. 2007;115:495-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 41. | Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD; VADT Investigators. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3445] [Cited by in RCA: 3323] [Article Influence: 207.7] [Reference Citation Analysis (0)] |
| 42. | Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545-2559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6292] [Cited by in RCA: 5608] [Article Influence: 329.9] [Reference Citation Analysis (0)] |
| 43. | Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, Cuddihy R, Cushman WC, Genuth S, Grimm RH Jr, Hamilton BP, Hoogwerf B, Karl D, Katz L, Krikorian A, O'Connor P, Pop-Busui R, Schubart U, Simmons D, Taylor H, Thomas A, Weiss D, Hramiak I; ACCORD trial group. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376:419-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1099] [Cited by in RCA: 995] [Article Influence: 66.3] [Reference Citation Analysis (0)] |
| 44. | Marre M, Lievre M, Chatellier G, Mann JF, Passa P, Ménard J; DIABHYCAR Study Investigators. Effects of low dose ramipril on cardiovascular and renal outcomes in patients with type 2 diabetes and raised excretion of urinary albumin: randomised, double blind, placebo controlled trial (the DIABHYCAR study). BMJ. 2004;328:495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 190] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 45. | ADVANCE Collaborative Group, Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560-2572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4759] [Cited by in RCA: 4888] [Article Influence: 287.5] [Reference Citation Analysis (0)] |
| 46. | Solomon SD, Chew E, Duh EJ, Sobrin L, Sun JK, VanderBeek BL, Wykoff CC, Gardner TW. Diabetic Retinopathy: A Position Statement by the American Diabetes Association. Diabetes Care. 2017;40:412-418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 445] [Cited by in RCA: 596] [Article Influence: 74.5] [Reference Citation Analysis (0)] |
| 47. | Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:766-785. [PubMed] |
| 48. | Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ. 2006;332:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1073] [Cited by in RCA: 1053] [Article Influence: 55.4] [Reference Citation Analysis (0)] |
| 49. | Giorda CB, Avogaro A, Maggini M, Lombardo F, Mannucci E, Turco S, Alegiani SS, Raschetti R, Velussi M, Ferrannini E; Diabetes and Informatics Study Group. Recurrence of cardiovascular events in patients with type 2 diabetes: epidemiology and risk factors. Diabetes Care. 2008;31:2154-2159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 50. | Packham DK, Alves TP, Dwyer JP, Atkins R, de Zeeuw D, Cooper M, Shahinfar S, Lewis JB, Lambers Heerspink HJ. Relative incidence of ESRD vs cardiovascular mortality in proteinuric type 2 diabetes and nephropathy: results from the DIAMETRIC (Diabetes Mellitus Treatment for Renal Insufficiency Consortium) database. Am J Kidney Dis. 2012;59:75-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 141] [Article Influence: 10.1] [Reference Citation Analysis (0)] |