Published online Aug 31, 2019. doi: 10.13105/wjma.v7.i8.399
Peer-review started: April 8, 2019
First decision: August 2, 2019
Revised: August 13, 2019
Accepted: August 20, 2019
Article in press: August 20, 2019
Published online: August 31, 2019
Processing time: 149 Days and 9.2 Hours
Blood glucose control, including hyperglycemia correction, maintaining glucose at optimal level and avoiding hypoglycemia, is a challenge clinicians face every day in intensive care units (ICUs). If managed inadequately, its related mortality can increase. Prior to 2001, no relevant data from randomized, controlled studies assessing glucose control in the ICU were available. In the past 18 years, however, many clinical trials have defined criteria for managing abnormal blood glucose levels, as well as provided suggestions for glycemic monitoring. Point-of-care blood glucose monitors have become the preferred bedside technology to aid in glycemic management. In addition, in some institutions, continuous glucose monitoring is now available. Cost-effectiveness of adequate glycemic control in the ICU must be taken into consideration when addressing this complex issue. Newer types of glycemic monitoring may reduce nursing staff fatigue and shorten times for the treatment of hyperglycemia or hypoglycemia. There are a variety of glycemic care protocols available. However, not all ICU clinicians are aware of them. The following minireview describes some of these concepts.
Core tip: Blood glucose control in the intensive care unit has remained a controversial topic since 2001, with many clinical trials attempting to elucidate which method provides the best option in terms of cost-effectiveness and in providing good clinical outcomes. As technology plays an important role in this matter, this minireview compiles the many features of state-of-the-art glycemic monitoring in the intensive care unit and treatment strategies for blood glucose control.
- Citation: Casillas S, Jauregui E, Surani S, Varon J. Blood glucose control in the intensive care unit: Where is the data? World J Meta-Anal 2019; 7(8): 399-405
- URL: https://www.wjgnet.com/2308-3840/full/v7/i8/399.htm
- DOI: https://dx.doi.org/10.13105/wjma.v7.i8.399
Critically ill patients present a special challenge when dealing with glycemic control, as they require correcting hyperglycemia while avoiding hypoglycemia and keeping blood glucose (BG) at optimal levels. This can have significant repercussions on the prognosis of these patients[1]. In the last 2 decades there have been a series of studies and added recommendations for glycemic control in the intensive care unit (ICU) setting[2-5]. For example, Van den Berghe et al[2,3] conducted a study among patients in the surgical ICU, who were managed with a rigorous glucose control protocol (maintenance of BG between 80-110 mg/dL) versus conventional treatment (infusion of insulin if BG > 215 mg/dL). They showed an increased survival rate and better prognosis, overall decrease in the mortality rate by 34%, as well as by sepsis (46%), polyneuropathy (44%) acute kidney injury (41%), and a significant decrease in blood transfusion requirements (50%)[2]. That particular study elicited some controversies, and additional randomized controlled trials were conducted. In 2009, the Normoglycemia in Intensive Care Evaluation-Survival Using Glucose Algorithm Regulation study (known by its acronym, NICE-SUGAR) revealed an increased mortality rate in those patients that underwent the tight glucose control (TGC) of 81-108 mg/dL, while moderate glucose control target of 140-180 mg/dL was associated with a higher survival rate[6]. This multicenter study emphasized the significant risk of hypoglycemic episodes with TGC due its proximity to the lower limit of the BG levels and other similar studies followed[6-8].
Independent of diabetes mellitus, there are many other clinical scenarios that may cause alterations in BG level among critically ill patients, although diabetics are most susceptible to these alterations[9-11]. Indeed, critically ill patients are usually admitted to the ICU with stress-induced hyperglycemia (50%-85%)[5,12]. For that reason, it is important to identify adequate BG monitoring methods. Continuous BG monitoring would be ideal but can be complex to interpret and treat. Current glucose monitoring devices are rudimentary, and laboratory results may take longer periods of time[13]. In this review, we present some aspects regarding the diagnosis, monitoring and management of glycemia in the ICU and discuss some of the newer technological advances that are at the forefront of continuous care of BG.
Hyperglycemia has been an important issue when dealing with glucose control in critically ill patients. Krinsley et al[9] conducted a retrospective study evaluating 1826 patients admitted to the ICU and reported a significant increase in mortality related to glycemic levels, reaching 42.5% in patients with higher mean glucose levels (> 300 mg/dL). These results are consistent with those from other studies, which also have shown that hyperglycemia is a marker of mortality in the ICU[1,14].
Hypoglycemia, on the other hand, is also an important contributing factor for mortality in critically ill patients. Many trials have tested the effectiveness of TGC and have shown it to be a risk factor for developing hypoglycemia (BG < 40 mg/dL) as well as a powerful marker for mortality; it was also found to be superior to hyperglycemia[6-8,15]. For example, hypoglycemia in intensive insulin therapy (IIT) was found to be 6-fold more common in patients with more liberal glycemic control[2,16].
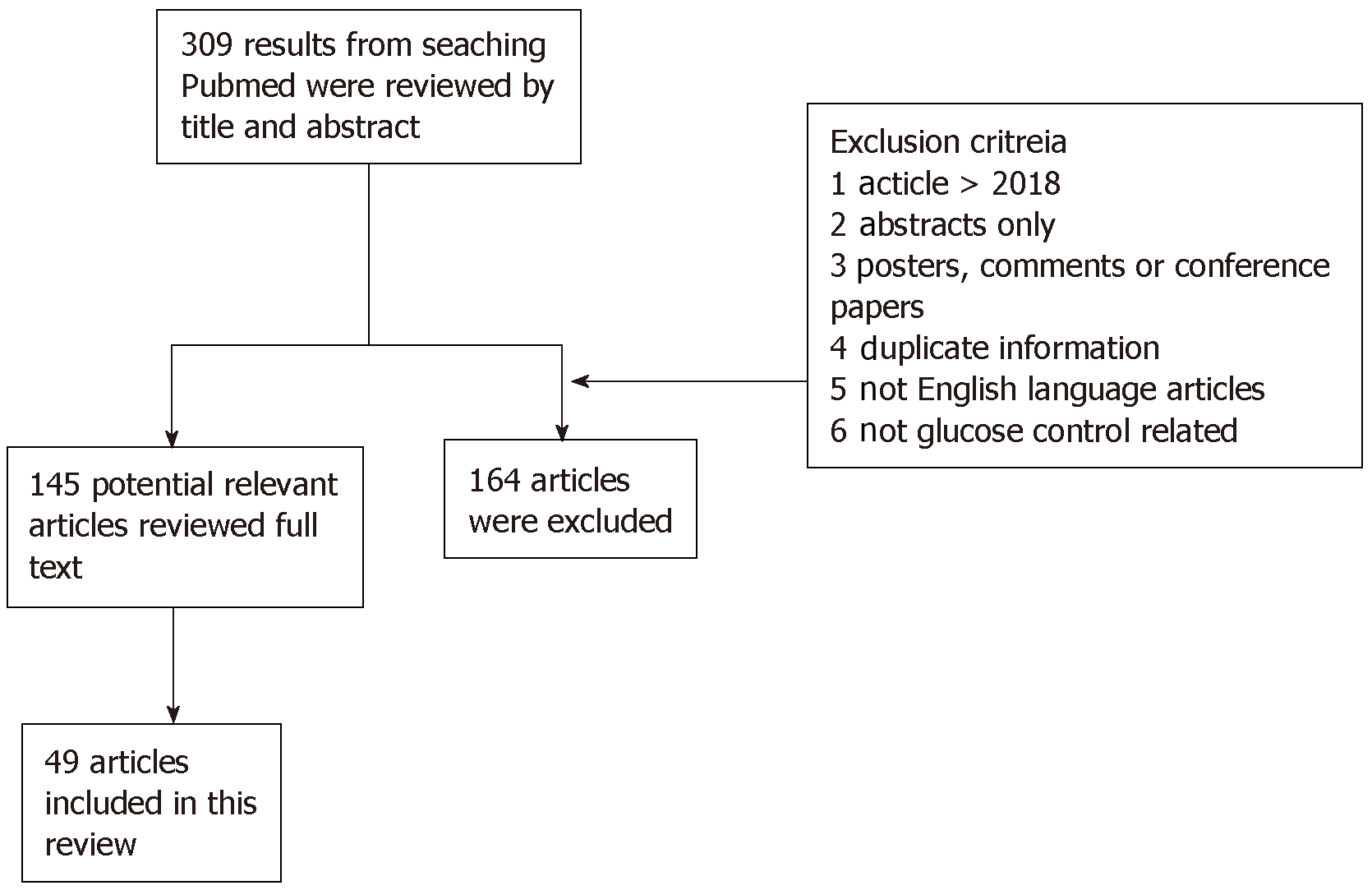
The authors independently searched an electronic database (PubMed™) using MeSH identifiers with the terms “blood glucose” and “intensive care unit” to identify articles published up to December 2018 with relevancy to glycemic care in the ICU. This search yielded 309 articles. Of those articles, after independent manual review, 160 potential articles were identified and reviewed. As the topic of this search was narrowed to the care of the critically ill patients, only 49 articles were included in this review. Abstract-only, posters, duplicate information, comments and conference papers were excluded. All data acquired were discussed later between the authors, and any disagreements were resolved (Figure 1).
Several different guidelines recommend certain parameters for glycemic control, with slight differences between the reference values, but a common denominator is the minimization of TGC. In 2011, the American College of Physicians recommended the use of the moderate range of 140-200 mg/dL and did not recommended TGC of 80-110 mg/dL, in order to avoid hypoglycemia and glucose variability (similar to the conclusive results from NICE-SUGAR)[17]. The following year, the American Diabetes Association recommended a very similar glycemic control, ranging from 140-180 mg/dL[18]. These recommendations are consistent with current critical care guidelines that support the use of insulin infusions in values that exceed 150 mg/dL, with the aim of maintaining a glycemia of 180 mg/dL in an attempt to avoid hypoglycemic episodes[19,20]. The Society of Critical Care Medicine guidelines recommended to keep a BG between 150 mg/dL and 180 mg/dL[19].
Despite these recommendations, some studies have reported results that have different outcomes. For example, the COIITSS study investigators ran a multicenter randomized clinical trial involving 509 adult patients with septic shock, revealing no significant mortality difference in patients with a target BG of 80-110 mg/dL compared to those with a target BG of 150 mg/dL[21].
In many studies, preexisting diabetes mellitus has remained a significant cause for bias in terms of glucose management, as prior studies have shown variability in the response to therapy and different mortality from other patients in the ICU[10]. These diabetic patients can develop resistance to glucose fluctuations and can actually benefit from higher BG ranges, avoiding BG variability and hypoglycemic episodes. Marik et al[22] suggested the necessary target BG ranges based on the hemoglobin A1c (referred to commonly as HbA1c; 160-220 mg/dL in patients with HbA1c > 7%, and 140-200 mg/dL in patients with HbA1c < 7%). Table 1 summarizes some of these guidelines and recommendations for critically ill patients.
| Study | Glycemic range | Ref. | Comments |
| American College of Physicians | 140-200 mg/dL | Qaseem et al[17], 2014 | Recommend use of moderate glucose control to avoid hypoglycemic episodes |
| American Diabetes Association | 140-180 mg/dL | American Diabetes Association[18], 2012 | Intensive insulin therapy in TGC can cause severe hypoglycemia |
| Society of Critical Care Medicine | 150-180 mg/dL | Jacobi et al[19], 2012 | Recommend the use of moderate use of glucose control |
| COIITSS study | 80-110 mg/dL | Annane et al[21], 2010 | No significant mortality in patients with TGC compared to MGC |
| Standards of medical care in diabetes | Nondiabetic HbA1c < 7% 140-200 mg/dL HbA1c > 7% 160-220 mg/dL | Marik et al[22], 2014 | Different approach between diabetics and nondiabetics, due to glucose variability in tolerance |
Prior to 2001, no randomized controlled trials had assessed specific BG targets among critically ill patients. More recently, a variety of studies have focused on management criteria for BG in critically ill patients via glycemic monitoring, use of IV insulin, and computerized processes. Krinsley et al[23], in a study of 1600 critically ill patients managed with insulin therapy, reported a 75% reduction in acute kidney injury, 19% decrease in the number of patients transfused with packed red blood cells, 11% decrease in length of ICU stay, and a drop of 29% in mortality. This study aimed to decrease glucose levels to < 140 mg/dL with IIT. However, in a systematic review and meta-analysis by Marik et al[15] reviewing TGC (80-110 mg/dL) in ICU patients and including seven randomized controlled trials with more than 11000 patients, no reduction was found in 28-d mortality, blood stream infections, or requirement for renal replacement therapy. These investigators concluded that there is no evidence to support the use of IIT in ICU patients. These findings have since been replicated by other studies[3,24]. In one such, continuous insulin infusion via central venous catheter led to hypoglycemia[24].
Other studies have shown less of a risk of hypoglycemia. In 2014, Amrein et al[25] conducted a nurse-driven trial with the Space Glucose Control System™ involving 40 critically ill patients and utilizing a computer-assisted device combined with an infusion pump for glycemic control. The target values were set at 80-150 mg/dL and it was noted that the adherence to the given insulin dose advised by the computer program was 98.2%; only one severe hypoglycemic episode occurred (0.03% of glucose readings)[25]. In a similar study of 210 patients in four different ICUs, monitoring BG was followed by management with a computerized insulin infusion program that had been programmed to a moderate glycemic range of 120-160 mg/dL in surgical ICUs and 140-180 mg/dL in medical ICUs[26]. The mean BG was 147 mg/dL in the surgical ICUs and 171 mg/dL in the medical ICUs. Only 17% had one or more glycemic episodes between 60-79 mg/dL and 9.8% < 70 mg/dL[26].
The Food and Drug Administration (commonly known as the FDA), in 2014, recommended that the use of point-of-care (POC) BG monitors were not suitable for critically ill patients[27]. In addition, the Centers for Medicare and Medicaid Services indicated that “off-label” use of such glucometers in the ICU could be subject to citations and fines during site evaluations[28]. The main reasons for the FDA and Centers for Medicare and Medicaid Services concerns was that ICU patients are unstable and that might cause erroneous BG readings.
In general, POC glucose monitors cost less, require smaller blood samples, and provide almost instant results. For years, they have been the preferred bedside glucose monitoring devices for glycemic management[29]. In a study of a large academic hospital, POC showed significant accuracy[30]. Results from glycemic POC paired to results of central laboratory testing of samples drawn no more than 60 min and passed the FDA’s 98% criteria[30].
New software incorporating current guidelines may be just as beneficial for glycemia control[31]. Some studies have used the Clinical Notification System that relies on specific criteria and notifies nursing staff of imminent hypoglycemia and persistent hyperglycemia, defined as two consecutive readings > 150 mg/dL[32,33]. The sensitivity and specificity of this system are excellent, being 98.1% and 99.1% respectively[32,33].
Continuous BG monitoring is now available[34-36]. In a single-center study comparing the benefits of continuous with intermittent glucose monitoring, a peripheral venous catheter was inserted with the GlucoClear™ probe[35]. These monitors were flushed with heparin, calibrated, and began BG monitoring every 5 min using a glucose oxidase-based method. Target glycemic ranges for this study were between 90-150 mg/dL. The number of patients with BG < 70 mg/dL in continuous versus the intermittent groups was 8/39 (20.5%) and 15/38 (39.5%) respectively. The time spent with BG < 70 mg/dL was calculated with a continuous glucose monitoring device, and resulted in 0.4% + -0.9% versus 1.6%+ -3.4% (P < 0.05) in intermittent glucose monitoring group[35].
In a study by Flower et al[36], utilizing a novel intravascular continuous glucose monitoring with chemical fluorescence sensing mechanism, 92.4% (404/437) were in target glycemic control (108-180 mg/dL), with no values < 72 mg/dL.
There are now subcutaneous continuous glucose monitoring sensors in case intravenous access is not available[37]. In a small cohort of 14 surgical ICU patients, the Sentrino continuous glucose monitoring glucometer (Medtronic, Dublin, Ireland) was used[38]. The study showed that the sensor provided good accuracy, overestimating glycemia by only 1.5 mg/dL[38].
The glycemic control protocols vary among different institutions and according to whether the patient has preexisting diabetes mellitus or not. The effects of IIT, for example, have been more noticeable in nondiabetic critical patients[39,40]. In one study, the mortality rates for nondiabetic patients undergoing IIT was 36.8%, as compared to 40.9% in the control group[39]. In addition, when compared to patients with diabetes, the interventional group mortality was 39.6% versus 36.8% in the diabetic group[39]. In fact, some authors have also suggested that diabetes may be “protective” in the ICU[40].
Mortality is lower for the ICU diabetic population when it comes to hyperglycemia and glucose variability, as compared to nondiabetics. However, hypoglycemia and severe hypoglycemia have an equal mortality rate for both types of patients[10,41]. In a study evaluating both nondiabetic patients and diabetic patients with tight and moderate glycemic control (80-110 mg/dL and 90-140 mg/dL), nondiabetic mortality was 11.9% in the moderate glycemic control group when compared to 8.1% in the TGC group[42]. In contrast, patients with diabetes had a 12.3% mortality with TGC compared to 9.8% for the moderate glycemic control group[42].
Cost analysis in the ICU remains an important topic. In one study, an economic analysis reported a cost-saving of 2638 Euros per patient in the group that was treated with intensive glycemic control[43]. Some have suggested that blood gas analyzers capable of monitoring continuous BG levels are the best option for accuracy and cost-saving, if they are in proximity to the ICU, even when the cost per device is $40000. The single test cost is very similar to a POC meter ($100) and the accuracy is equal to a central laboratory device[44]. It is clear that euglycemia and avoidance of hypoglycemia decreases the length of stay in the hospital (from 29 d to 24 d) and has a lower health-care cost (mean $5847), showing a notable amount of money-saving in 5 d[45].
Another factor to consider when analyzing cost savings is the role of TGC in reducing blood stream infections. Some studies have reported that decreasing 5% of hospital-acquired infections could improve cost savings considerably; in fact, one of these studies showed a cost-saving of $1580 per patient, driven by the decreased length of stay in the ICU[46,47]. Such goals can be achieved by attempting to control BG with avoidance of hypoglycemia.
As noted above, dysregulation of glycemia is a significant factor in the poor prognosis of an ICU patient[48]. There are other contributing factors that can change the glycemic status, such as age (older), underweight condition, and type of feeding that is managed in the ICU, since these are labile and can create fluctuations in a more noticeable way compared with the rest of the patients. Critical care clinicians may not be fully aware of these findings. Indeed, some survey studies have shown that clinicians vary significantly in how they manage glycemic index in the ICU and very few are aware that hypoglycemia is associated with an increased hospital mortality[49]. Educational programs aimed at understanding these important risk factors are needed. The development of professional awareness of current guidelines and introduction of new technologies are the first step for improving patient care outcomes.
We believe that computerized, protocol-driven and continuous BG monitoring will become the standard of care in ICUs across the world.
Manuscript source: Invited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E, E, E
P-Reviewer: Ding JX, Saisho Y, Nakajima K, Hosseinpour-Niazi S S-Editor: Dou Y L-Editor: Filipodia E-Editor: Zhou BX
| 1. | Lu M, Zuo Y, Guo J, Wen X, Kang Y. Continuous glucose monitoring system can improve the quality of glucose control and glucose variability compared with point-of-care measurement in critically ill patients: A randomized controlled trial. Medicine (Baltimore). 2018;97:e12138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7077] [Cited by in RCA: 6184] [Article Influence: 257.7] [Reference Citation Analysis (2)] |
| 3. | Van den Berghe G. What's new in glucose control in the ICU? Intensive Care Med. 2013;39:823-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Preiser JC, Chase JG, Hovorka R, Joseph JI, Krinsley JS, De Block C, Desaive T, Foubert L, Kalfon P, Pielmeier U, Van Herpe T, Wernerman J. Glucose Control in the ICU: A Continuing Story. J Diabetes Sci Technol. 2016;10:1372-1381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 5. | De Block C, Manuel-y-Keenoy B, Rogiers P, Jorens P, Van Gaal L. Glucose control and use of continuous glucose monitoring in the intensive care unit: a critical review. Curr Diabetes Rev. 2008;4:234-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Lleva RR, Thomas P, Bozzo JE, Hendrickson KC, Inzucchi SE. Using the glucometrics website to benchmark ICU glucose control before and after the NICE-SUGAR study. J Diabetes Sci Technol. 2014;8:918-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Bersoux S, Cook CB, Kongable GL, Shu J. RETROSPECTIVE STUDY OF GLYCEMIC CONTROL FOLLOWING TRANSITION FROM THE INTENSIVE CARE UNIT IN A NATIONAL SAMPLE OF U.S. HOSPITALS. Endocr Pract. 2015;21:986-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Dodson CH, Simpson J, Feinstein D. Glycemic control in a medical intensive care setting: revision of an intensive care unit nurse-driven hyperglycemia protocol. Crit Care Nurs Q. 2014;37:170-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471-1478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 834] [Cited by in RCA: 785] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 10. | Krinsley JS, Egi M, Kiss A, Devendra AN, Schuetz P, Maurer PM, Schultz MJ, van Hooijdonk RT, Kiyoshi M, Mackenzie IM, Annane D, Stow P, Nasraway SA, Holewinski S, Holzinger U, Preiser JC, Vincent JL, Bellomo R. Diabetic status and the relation of the three domains of glycemic control to mortality in critically ill patients: an international multicenter cohort study. Crit Care. 2013;17:R37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 212] [Cited by in RCA: 252] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 11. | Jamaludin UK, M Suhaimi F, Abdul Razak NN, Md Ralib A, Mat Nor MB, Pretty CG, Humaidi L. Performance of Stochastic Targeted Blood Glucose Control Protocol by virtual trials in the Malaysian intensive care unit. Comput Methods Programs Biomed. 2018;149-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Fahy BG, Sheehy AM, Coursin DB. Glucose control in the intensive care unit. Crit Care Med. 2009;37:1769-1776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 111] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 13. | Krinsley JS. Glycemic variability: a strong independent predictor of mortality in critically ill patients. Crit Care Med. 2008;36:3008-3013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 527] [Cited by in RCA: 520] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 14. | Godinjak A, Iglica A, Burekovic A, Jusufovic S, Ajanovic A, Tancica I, Kukuljac A. Hyperglycemia in Critically Ill Patients: Management and Prognosis. Med Arch. 2015;69:157-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Marik PE, Preiser JC. Toward understanding tight glycemic control in the ICU: a systematic review and metaanalysis. Chest. 2010;137:544-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 235] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 16. | Kavanagh BP, McCowen KC. Clinical practice. Glycemic control in the ICU. N. Engl J Med. 2010;363:2540-2546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 129] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 17. | Qaseem A, Chou R, Humphrey LL, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Inpatient glycemic control: best practice advice from the Clinical Guidelines Committee of the American College of Physicians. Am J Med Qual. 2014;29:95-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | American Diabetes Association. Executive summary: Standards of medical care in diabetes--2012. Diabetes Care. 2012;35 Suppl 1:S4-S10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 173] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 19. | Jacobi J, Bircher N, Krinsley J, Agus M, Braithwaite SS, Deutschman C, Freire AX, Geehan D, Kohl B, Nasraway SA, Rigby M, Sands K, Schallom L, Taylor B, Umpierrez G, Mazuski J, Schunemann H. Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Crit Care Med. 2012;40:3251-3276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 386] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 20. | Clain J, Ramar K, Surani SR. Glucose control in critical care. World J Diabetes. 2015;6:1082-1091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 42] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | COIITSS Study Investigators. Annane D, Cariou A, Maxime V, Azoulay E, D'honneur G, Timsit JF, Cohen Y, Wolf M, Fartoukh M, Adrie C, Santré C, Bollaert PE, Mathonet A, Amathieu R, Tabah A, Clec'h C, Mayaux J, Lejeune J, Chevret S. Corticosteroid treatment and intensive insulin therapy for septic shock in adults: a randomized controlled trial. JAMA. 2010;303:341-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 204] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 22. | Marik PE, Egi M. Treatment thresholds for hyperglycemia in critically ill patients with and without diabetes. Intensive Care Med. 2014;40:1049-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Krinsley JS. Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc. 2004;79:992-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 910] [Cited by in RCA: 795] [Article Influence: 37.9] [Reference Citation Analysis (0)] |
| 24. | Maury E, Vitry P, Galbois A, Ait-Oufella H, Baudel JL, Guidet B, Offenstadt G. Continuous insulin administration via complex central venous catheter infusion tubing is another risk factor for blood glucose imbalance. A retrospective study. Ann Intensive Care. 2012;2:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Amrein K, Kachel N, Fries H, Hovorka R, Pieber TR, Plank J, Wenger U, Lienhardt B, Maggiorini M. Glucose control in intensive care: usability, efficacy and safety of Space GlucoseControl in two medical European intensive care units. BMC Endocr Disord. 2014;14:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Sandler V, Misiasz MR, Jones J, Baldwin D. Reducing the risk of hypoglycemia associated with intravenous insulin: experience with a computerized insulin infusion program in 4 adult intensive care units. J Diabetes Sci Technol. 2014;8:923-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 27. | Klonoff DC. Point-of-Care Blood Glucose Meter Accuracy in the Hospital. Setting. Diabetes Spectr. 2014;27:174-179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 28. | DuBois JA, Slingerland RJ, Fokkert M, Roman A, Tran NK, Clarke W, Sartori DA, Palmieri TL, Malic A, Lyon ME, Lyon AW. Bedside Glucose Monitoring-Is it Safe? A New, Regulatory-Compliant Risk Assessment Evaluation Protocol in Critically Ill Patient Care Settings. Crit Care Med. 2017;45:567-574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 29. | Seley JJ, Diaz R, Greene R. Blood Glucose Meters in ICUs. Am J Nurs. 2016;116:46-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Zhang R, Isakow W, Kollef MH, Scott MG. Performance of a Modern Glucose Meter in ICU and General Hospital Inpatients: 3 Years of Real-World Paired Meter and Central Laboratory Results. Crit Care Med. 2017;45:1509-1514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Dubois J, Van Herpe T, van Hooijdonk RT, Wouters R, Coart D, Wouters P, Van Assche A, Veraghtert G, De Moor B, Wauters J, Wilmer A, Schultz MJ, Van den Berghe G, Mesotten D. Software-guided versus nurse-directed blood glucose control in critically ill patients: the LOGIC-2 multicenter randomized controlled clinical trial. Crit Care. 2017;21:212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 32. | Colpaert K, Oeyen S, Sijnave B, Peleman R, Benoit D, Decruyenaere J. Influence of smart real-time electronic alerting on glucose control in critically ill patients. J Crit Care. 2015;30:216.e1-216.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Berger MM, Que YA. Bioinformatics assistance of metabolic and nutrition management in the ICU. Curr Opin Clin Nutr Metab Care. 2011;14:202-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Crane BC, Barwell NP, Gopal P, Gopichand M, Higgs T, James TD, Jones CM, Mackenzie A, Mulavisala KP, Paterson W. The Development of a Continuous Intravascular Glucose Monitoring Sensor. J Diabetes Sci Technol. 2015;9:751-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 35. | Preiser JC, Lheureux O, Thooft A, Brimioulle S, Goldstein J, Vincent JL. Near-Continuous Glucose Monitoring Makes Glycemic Control Safer in ICU Patients. Crit Care Med. 2018;46:1224-1229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 36. | Flower OJ, Bird S, Macken L, Hammond N, Yarad E, Bass F, Fisher C, Strasma P, Finfer S. Continuous intra-arterial blood glucose monitoring using quenched fluorescence sensing: a product development study. Crit Care Resusc. 2014;16:54-61. [PubMed] |
| 37. | Yue XY, Zheng Y, Cai YH, Yin NN, Zhou JX. Real-time continuous glucose monitoring shows high accuracy within 6 hours after sensor calibration: a prospective study. PLoS One. 2013;8:e60070. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 38. | Punke MA, Decker C, Wodack K, Reuter DA, Kluge S. Continuous glucose monitoring on the ICU using a subcutaneous sensor. Med Klin Intensivmed. Notfmed. 2015;110:360-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 39. | Krinsley JS, Meyfroidt G, van den Berghe G, Egi M, Bellomo R. The impact of premorbid diabetic status on the relationship between the three domains of glycemic control and mortality in critically ill patients. Curr Opin Clin Nutr Metab Care. 2012;151-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 40. | Krinsley JS, Fisher M. The diabetes paradox: diabetes is not independently associated with mortality in critically ill patients. Hosp Pract (1995). 2012;40:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 41. | Sechterberger MK, Bosman RJ, Oudemans-van Straaten HM, Siegelaar SE, Hermanides J, Hoekstra JB, De Vries JH. The effect of diabetes mellitus on the association between measures of glycaemic control and ICU mortality: a retrospective cohort study. Crit Care. 2013;17:R52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 42. | Lanspa MJ, Hirshberg EL, Phillips GD, Holmen J, Stoddard G, Orme J. Moderate glucose control is associated with increased mortality compared with tight glucose control in critically ill patients without diabetes. Chest. 2013;143:1226-1234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 43. | Van den Berghe G, Wouters PJ, Kesteloot K, Hilleman DE. Analysis of healthcare resource utilization with intensive insulin therapy in critically ill patients. Crit Care Med. 2006;612-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 139] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 44. | Le HT, Harris NS, Estilong AJ, Olson A, Rice MJ. Blood glucose measurement in the intensive care unit: what is the best method? J Diabetes Sci Technol. 2013;7:489-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 45. | Macrae D, Grieve R, Allen E, Sadique Z, Morris K, Pappachan J, Parslow R, Tasker RC, Elbourne D; CHiP Investigators. A randomized trial of hyperglycemic control in pediatric intensive care. N Engl J Med. 2014;370:107-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 154] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 46. | Krinsley JS. Is glycemic control of the critically ill cost-effective? Hosp Pract (1995). 2014;42:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 47. | Krinsley JS, Jones RL. Cost analysis of intensive glycemic control in critically ill adult patients. Chest. 2006;129:644-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 127] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 48. | Liu X, Wang DF, Xiong J. [Prospective observational study exploring the relationship between the levels and variability of blood glucose and the prognosis of critical patients]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2012;24:538-540. [PubMed] [DOI] [Full Text] |
| 49. | Liu X, Wang DF, Liu Y, Tang Y, Xiong J. Attitudes, Knowledge, and Practices Regarding Blood Glucose Control: A Survey of Intensive Care Unit Professionals. Chin Med J (Engl). 2018;131:622-623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |