Published online Jun 26, 2015. doi: 10.13105/wjma.v3.i3.181
Peer-review started: January 27, 2015
First decision: February 7, 2015
Revised: April 9, 2015
Accepted: April 16, 2015
Article in press: April 20, 2015
Published online: June 26, 2015
Processing time: 156 Days and 0.4 Hours
AIM: To investigate whether an association exists between sleep-associated movement disorders and cardiovascular disease (CVD).
METHODS: Several studies have observed the relationship of sleep-associated movement disorders such as restless legs syndrome (RLS) and periodic limb movements during sleep with CVD, but the results were still contradictory. We performed an extensive literature search on PubMed, Medline and Web of Science published from inception to December 2014. Additional studies were manually searched from bibliographies of retrieved studies. Meta-analyses were conducted with Stata version 12.0 (Stata Corp, College Station, Texas). Pooled odds ratios (ORs) and 95%CIs were calculated to assess the strength of association using the random effects model. Sensitivity and subgroup analyses were performed to explore the underlying sources of heterogeneity. The publication bias was detected using Egger’s test and Begg’s test.
RESULTS: A total of 781 unique citations were indentified from electronic databases and 13 articles in English were finally selected. Among these studies, nine are cohort studies; two are case-control studies; and two are cross-sectional studies. The results showed that the summary OR of CVD associated with sleep-associated movement was 1.51 (95%CI: 1.29-1.77) in a random-effects model. There was significant heterogeneity between individual studies (P for heterogeneity = 0.005, I2 = 57.6%). Further analysis revealed that a large-scale cohort study may account for this heterogeneity. A significant association was also found between RLS and CVD (OR = 1.54, 95%CI: 1.24-1.92). In a fixed-effects model, we determined a significant relationship between sleep-associated movement disorders and coronary artery disease (CAD) (OR = 1.34, 95%CI: 1.16-1.54; P for heterogeneity = 0.210; I2 = 30.0%). Our meta-analysis suggests that sleep-associated movement disorders are associated with prevalence of CVD and CAD.
CONCLUSION: This finding indicates that sleep-associated movement disorders may prove to be predictive of underlying CVD.
Core tip: We conducted a meta-analysis of 13 relevant studies to investigate the association between sleep-associated movement disorders and cardiovascular disease (CVD). The present study suggested that sleep-associated movement disorders are associated with prevalence of CVD. This finding indicates that sleep-associated movement disorders may prove to be predictive of underlying CVD.
- Citation: Fang Z, Liu YW, Zhao LY, Xu Y, Zhang FX. Sleep-associated movement disorders and the risk of cardiovascular disease: A systematic review and meta-analysis. World J Meta-Anal 2015; 3(3): 181-187
- URL: https://www.wjgnet.com/2308-3840/full/v3/i3/181.htm
- DOI: https://dx.doi.org/10.13105/wjma.v3.i3.181
Sleep-associated movement disorders are a group of movement disorders which occur during sleep in relation to episodes of arousal and sleep disorder. They are characterized by the persistence of muscle tone or the emergence of motor activity. Among of them, restless legs syndrome (RLS) and periodic limb movements during sleep (PLMS) are the two most common disorders encountered in adult. RLS affects approximately 5%-10% of the general population and up to 80% of RLS patients may have PLMS[1,2]. RLS and PLMS can result in similar clinical problems due to sleep disruption[3]. Recently, several studies indicate that untreated RLS with PLMS may contribute partly to secondary causes of uncontrolled hypertension and cardiovascular disease (CVD), while some studies demonstrated negative results[4,5]. Therefore, the objective of the present study was to provide a systematic review and meta-analysis of the available evidence on the association between sleep-associated movement disorders and CVD in general populations.
This meta-analysis was based on the guidelines of the Meta-analysis of Observational Studies in Epidemiology Group[6].
We performed a literature search of PubMed, Medline and Web of Science using key words of ‘‘periodic limb movements”, “RLS”, “heart disease’’, “CVD”, “coronary artery disease (CAD)’’ and ‘‘sleep-associated movement disorders” published from inception to December 2014. Additional studies were manually searched from references of related studies or reviews and the language was limited in English. Review articles, abstracts, correspondence, conference proceedings and book chapters were excluded, and only one instance of the study found in multiple journals was included.
Prospective cohort, case-control, and cross-sectional studies based in general populations that assessed the association of sleep-associated movement disorders with CVD were eligible for this systematic review. Exclusion criteria were as follows: (1) duplicated studies; (2) no controls; and (3) no detail risk estimates and 95%CIs. We included only published full-text that assessed sleep-associated movement disorders and CVD, or that provided sufficient data to calculate risk estimates of CVD associated with sleep-associated movement disorders. Unpublished reports, abstracts, comments, reviews, case report or editorials were not considered in this review. CVD in our investigation were defined as CAD, heart failure (HF) and stroke, not including hypertension.
Two reviewers independently extracted eligible data by screening the titles and abstracts of the search results and evaluating the remaining full-text articles. Disagreements were discussed till consensus was achieved. The following data were extracted: the first authors’ name, publication year, country where the study was conducted, study type, RLS or PLMS, number of samples, crude or adjusted risk estimates and 95%CIs. Different study types were divided into prospective cohort, case-control, and cross-sectional studies.
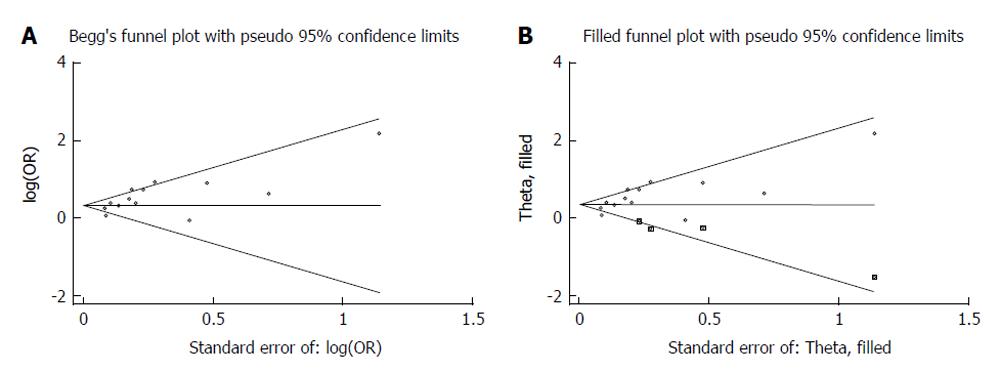
Summary odds ratios (ORs) and 95%CIs were used to measure the association strength between sleep-associated movement disorders and CVD risk. Cochran’s Q statistic and the I2 statistic were used to quantify between-study heterogeneity. The heterogeneity was considered as significant with a conservative P value of 0.10 and a value of I2 exceeding 56%. We pooled ORs, relative risks and hazard ratios (HRs) with the random-effects model when a significant heterogeneity exists, otherwise, with the fixed-effect model[7]. We also performed subgroup analyses to explore the underlying confounding factor. Sensitivity analyses were carried out to test the reliability of results. We checked for funnel plot asymmetry, Begg’s test and Egger’s test to assess potential publication bias, and the significant P value was < 0.05[8,9]. The “trim and fill” procedure was utilized to further evaluate the possible effect of publication bias in the present meta-analysis[7]. All analyses were calculated with Stata version 12.0 (Stata Corp, College Station, Texas).
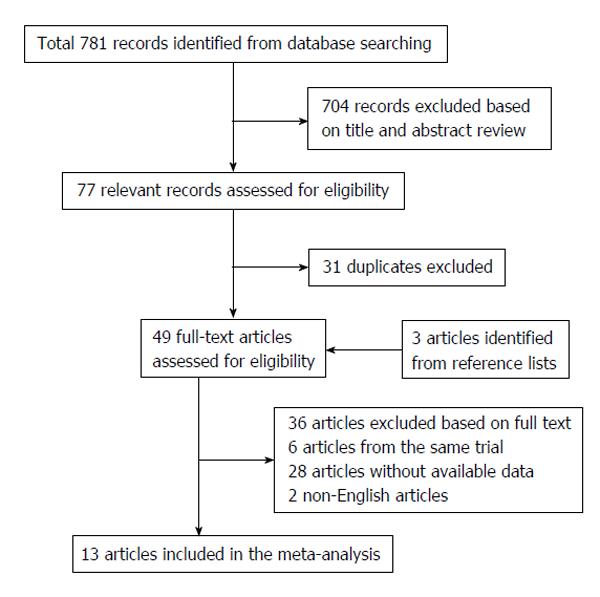
A total of 781 unique citations were identified: 279 from PubMed, 283 from Medline and 219 from Web of Science. The flow of study identification was shown in Figure 1[10-22]. Table 1 shows characteristics of eligible studies and the effect of sleep-associated movement disorders on the risk for CVD and CAD. Among these studies, nine are cohort studies; two are case-control studies; and two are cross-sectional studies. All participants were investigated from either European countries or United States. The sample sources of cases in nine studies were RLS patients and five were PLMS patients, including one study investigating both PLS and PLMS patients. The risk estimates and 95%CIs of most studies were extracted directly from original articles except for those of seven studies were recalculated by merging raw data[12-14,17,19,20,22].
| Ref. | Year | Country | Study type | Total | Source of patients | CVD-OR (95%CI) | CAD-OR (95%CI) |
| Hanly et al[10] | 1996 | Canada | Cohort | 32 | PLMS | 8.73 (0.94-81.49) | - |
| Ulfberg et al[11] | 2001 | Sweden | Case-control | 4000 | RLS | 2.50 (1.40-4.30) | - |
| Ohayon et al[12] | 2002 | 5 European countries | Cross-sectional | 18980 | PLMS/RLS | 1.47 (1.12-1.81) | - |
| Winkelman et al[13] | 2006 | United States | Cohort | 2821 | RLS | 2.07 (1.31-3.27) | |
| Elwood et al[14] | 2006 | United Kingdom | Cohort | 1871 | RLS | 1.38 (1.06-1.81) | 1.24 (0.89-1.74) |
| Winkelman et al[15] | 2008 | United States | Cross-sectional | 3433 | RLS | 2.07 (1.43-3.00) | 2.05 (1.38-3.04) |
| Walters et al[16] | 2010 | United States | Cohort | 267 | RLS | 2.46 (0.97-6.28) | - |
| Koo et al[17] | 2011 | United States | Cohort | 2911 | PLMS | 1.28 (1.08-1.51) | 1.23 (1.01-1.50) |
| Li et al[18] | 2012 | United States | Cohort | 70977 | RLS | 1.46 (0.97-2.18) | 1.46 (0.97-2.18) |
| Winter et al[19] | 2012 | United States | Cohort | 48938 | RLS | 1.06 (0.90-1.26) | - |
| Lindner et al[20] | 2012 | Hungary | Cohort | 150 | PLMS | 1.85 (0.46-7.51) | 1.15 (0.35-3.81) |
| Mirza et al[21] | 2013 | United States | Case-control | 584 | PLMS | 1.62 (1.14-2.30) | - |
| Szentkirályi et al[22] | 2013 | German | Cohort | 4308 | RLS | 0.94 (0.42-2.10) | 0.53 (0.12-2.27) |
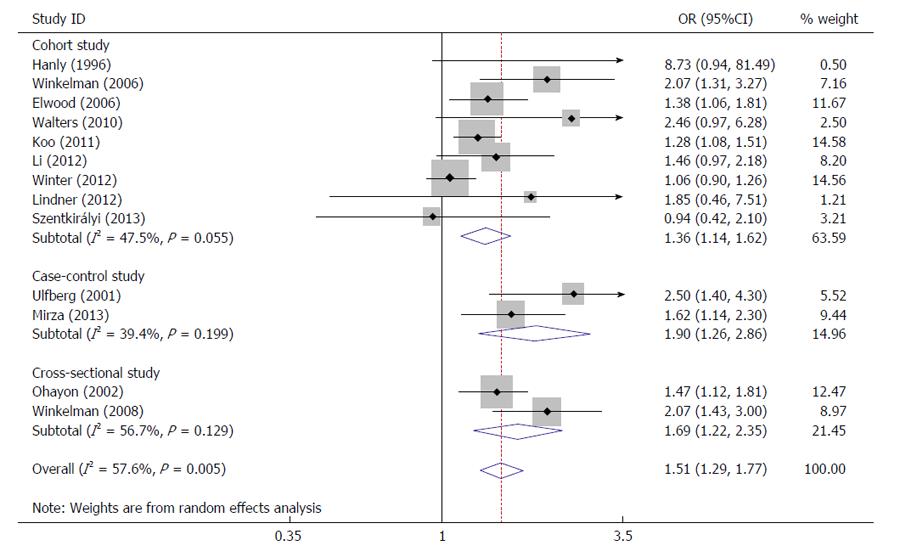
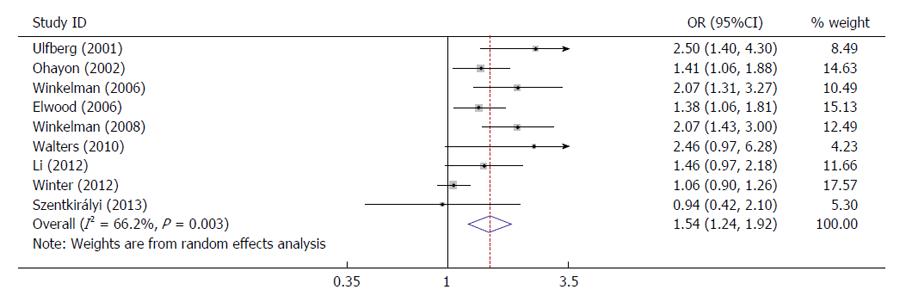
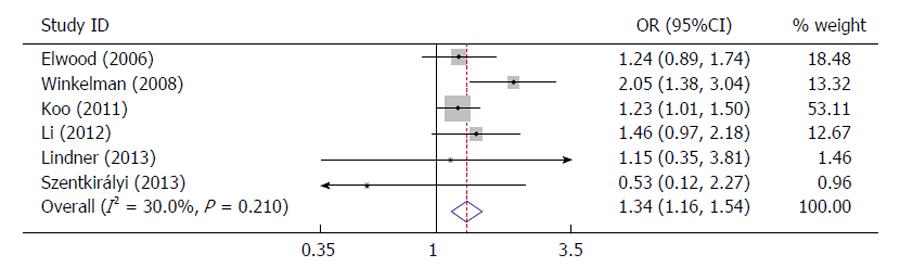
Several studies indicated that sleep-associated movement disorders were associated with a significant increased risk for CVD; while others showed inconsistent findings (Figure 2). In a random-effects model, the summary OR of CVD associated with sleep-associated movement was 1.51 (95%CI: 1.29-1.77), with the evidence of heterogeneity (P for heterogeneity = 0.005, I2 = 57.6%) (Figure 2). In subgroup analysis by study type, the summary OR was 1.36 for nine cohort studies (95%CI: 1.14-1.62; P for heterogeneity = 0.055; I2 = 47.5%) (Figure 2). Figure 3 listed that a significant association was also found between RLS and CVD (OR = 1.54, 95%CI: 1.24-1.92). In a fixed-effects model, we determined a significant association of sleep-associated movement disorders with CAD (OR = 1.34, 95%CI: 1.16-1.54; P for heterogeneity = 0.210; I2 = 30.0%) (Figure 4).
Sensitive analysis was performed by sequentially excluding each study to test the stability of the results in the present meta-analysis. After removing a study performed by Winter et al[19] which allowed the assessment of incident CVD cases, we found no significantly heterogeneity existed between overall studies (P = 0.112, I2 = 34.8%). In addition, there was no significantly influence on the pooled OR of the CVD risk (OR = 1.49, 95%CI: 1.35-1.64). Therefore, the different study design may be a possible origin of heterogeneity. Then we conducted the funnel plot and Egger’s test to assess the publication bias of literatures. Visual assessment of the Begg funnel plot revealed asymmetry (Figure 5A). This indicates the potential publication bias, although the Begg’s test showed no statistically significance (Z = 1.53, P = 0.127). In order to identify and correct for funnel plot asymmetry arising from publication bias, we continued the analysis using the trim and fill method. The other four hypothetical studies were filled to produce a symmetrical funnel plot (Figure 5B). After that, the meta-analysis still showed a statistically significant association between sleep-associated movement disorders and CVD (OR = 1.39, 95%CI: 1.19-1.63).
Plenty of evidences have revealed screening, identification, and treatment of sleep disorders were important among patients with CVD. Several studies showed RLS were associated with hypertension and heart disease, because RLS may contribute to a high cardiovascular burden[1,11,12]. In 2001, Ulfberg et al[11] found an association of RLS with both self-reported hypertension and heart problems in 4000 Swedish men aged 18 to 64 years (hypertension: OR = 1.5, 95%CI: 0.9-2.4; heart problems: OR = 2.5, 95%CI: 1.4-4.3). Ohayon et al[12] reported heart disease made a significant independent contribution to RLS (OR = 1.41, 95%CI: 1.06-1.88). In a cohort study, Elwood et al[14] identified RLS is associated with a significant increase in ischaemic heart disease events among 1871 men in South Wales, United Kingdom during the following 10 years (OR = 1.24, 95%CI: 0.89-1.71). In the Wisconsin Sleep Cohort study of 2006, Winkelman et al[15] observed a dose-related association between RLS symptoms and CVD (Frequent: OR = 1.61, 95%CI: 0.82-3.13; Daily: OR = 2.58, 95%CI: 1.38-4.84). Moreover, Winkelman et al[15] also demonstrated the association of RLS with CVD and CAD in a large cross-sectional observational community-based study of 1559 men and 1874 women (CAD: OR = 2.05, 95%CI = 1.38-3.04; CVD: OR = 2.07, 95%CI: 1.43-3.00) for subjects with RLS compared to those without RLS, and the associations were stronger in those with RLS more frequent or severer symptoms[15]. Li et al[18] performed a large-scale prospective study to examine whether RLS was associated with an increased risk of CAD in women of the Nurses’ Health Study (HR = 1.46, 95%CI: 0.97-2.18). The fact suggests that CVD could be result from the long-term impact of RLS or RLS-associated conditions. Nevertheless, a study from Walters et al[16] showed that there was no statistically difference in the prevalence of CVDs or risk factors between RLS patients and controls, which may be caused by the limited sample size. Another two large prospective cohort studies (Women’s Health Study and Physicians’ Health Study, United States) also did not support that RLS is a marker of increased risk of vascular disease. The discrepancy between these two results and those of previous studies may be explained by the prospective cohort study, which was designed to assess incident CVD cases[19].
Ninety-nine percent of PLMS are related to greater heart rate response, which result in sympathetic activation as a cause of cardiovascular complications[1,23,24]. In 1996, Hanly et al[10] for first time found an association between congestive HF and increased prevalence of PLMS. Furthermore, a cross-sectional study was performed in the five European countries, identifying CVD certainly associated with PLMS (OR = 1.61, 95%CI: 1.09-2.39). A study published in 2011 from Koo et al[17] supported PLMS frequency may be a predictive factor of incident CVD. In a recent study by Mirza et al[23], periodic limb movement index > 35/h were found to confer a high risk for HF (OR = 1.62; 95%CI: 1.14-2.30).
To clarify the controversial results of previous studies regarding the association of sleep-associated movement disorders with CVD, we performed this meta-analysis. Our analysis suggested that sleep-associated movement might play an important role in the development of heart disease, particular in prevalence of CAD. As different study design of the previous works might contribute to discrepancies between previous reports, thus we conducted subgroup analysis by study types which suggested the association was only to be weaker but still significant in cohort studies. In addition, our results also provided a stronger evidence for the significant relationship between RLS and CVD. However, the exact mechanism of the effect of sleep-associated movement disorders on cardiovascular system remains unclear. The most accepted hypothesis is these disorders may result from sustained adrenergic surges caused by sympathetic nervous system activation, which predispose to persistent elevated blood pressure as well as increased left ventricular afterload and heart rate. Another possible explanation is that sleep-associated movement disorders interrupt sleep which raises heart risk[25].
Some limitations of our meta-analysis should be considered. First, the results of the present meta-analysis remain cautious due to heterogeneity across studies. Second, the risk estimate of each study included was not adjusted by the same covariable related to risk of CVD. Third, the asymmetry shape of the funnel plot suggested the possibility of publication bias, even the trim and fill sensitivity analysis has been used to test the stability of the results. Fourth, all sample sources are of European or United States descent, which lead to lacking data from other ethnicity backgrounds.
In conclusion, the current meta-analysis suggests that sleep-associated movement disorders are associated with prevalence of CVD, which may be predictive of CVD. This finding may settle the controversy among previous investigations. However, further well-designed and mechanistic work should undertake to confirm this association.
The burden of cardiovascular disease (CVD) is increasing globally, especially in developing countries such as China. CVD has been the first leading cause of mortality in China. It has been known that unhealthy life style is the most common induced factor of CVD which can also lead to other disease like diabetes, obesity and so on. Therefore, the prevention of CVD, which consumes less, is more important than treatment in developing countries. Sleep-associated movement disorders is a group of symptoms that easily been ignore by the public and some limited studies seem to indicate they may be also the underlying cause of CVD, although this association is not been well established.
Over the recent 2 decades, many studies attempted to understand the associations between sleep-associated movement disorders and CVD. However, it is difficult to obtain an inconsistent conclusion about the association from the previous studies.
From this meta-analysis, sleep-associated movement disorders may increase the risk of CVD by approximately 51%. Significant associations also showed in subgroup analyses of nine cohort studies. And sleep-associated movement disorders may be predictively used in the prevention of coronary artery disease in the future based the current investigation.
Sleep-associated movement disorders appear to be either directly or indirectly associated with the risk of CVD. An exploration of the mechanism for this association may help us decrease the prevalence of CVD.
Sympathetic nervous system is a web of nerves and neurons spreading excitement to each organ of body. Left ventricular afterload is the encountering resistance when the myocardial of left ventricular contracts.
Well written and concise meta-analysis.
P- Reviewer: Lazzeri C, Lin GM S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Schaffernocker T, Ho J, Hayes D. Sleep-associated movement disorders and heart failure. Heart Fail Rev. 2009;14:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lespérance P. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Mov Disord. 1997;12:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 634] [Cited by in RCA: 580] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 3. | Ancoli-Israel S, Kripke DF, Klauber MR, Mason WJ, Fell R, Kaplan O. Periodic limb movements in sleep in community-dwelling elderly. Sleep. 1991;14:496-500. [PubMed] |
| 4. | Ferini-Strambi L, Walters AS, Sica D. The relationship among restless legs syndrome (Willis-Ekbom Disease), hypertension, cardiovascular disease, and cerebrovascular disease. J Neurol. 2014;261:1051-1068. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Walters AS, Rye DB. Review of the relationship of restless legs syndrome and periodic limb movements in sleep to hypertension, heart disease, and stroke. Sleep. 2009;32:589-597. [PubMed] |
| 6. | Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008-2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14425] [Cited by in RCA: 16795] [Article Influence: 671.8] [Reference Citation Analysis (0)] |
| 7. | Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21630] [Cited by in RCA: 25800] [Article Influence: 1121.7] [Reference Citation Analysis (0)] |
| 8. | Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34245] [Cited by in RCA: 40536] [Article Influence: 1447.7] [Reference Citation Analysis (2)] |
| 9. | Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088-1101. [PubMed] |
| 10. | Hanly PJ, Zuberi-Khokhar N. Periodic limb movements during sleep in patients with congestive heart failure. Chest. 1996;109:1497-1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 55] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Ulfberg J, Nyström B, Carter N, Edling C. Prevalence of restless legs syndrome among men aged 18 to 64 years: an association with somatic disease and neuropsychiatric symptoms. Mov Disord. 2001;16:1159-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 267] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 12. | Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res. 2002;53:547-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 489] [Cited by in RCA: 423] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 13. | Winkelman JW, Finn L, Young T. Prevalence and correlates of restless legs syndrome symptoms in the Wisconsin Sleep Cohort. Sleep Med. 2006;7:545-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 201] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 14. | Elwood P, Hack M, Pickering J, Hughes J, Gallacher J. Sleep disturbance, stroke, and heart disease events: evidence from the Caerphilly cohort. J Epidemiol Community Health. 2006;60:69-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 169] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 15. | Winkelman JW, Shahar E, Sharief I, Gottlieb DJ. Association of restless legs syndrome and cardiovascular disease in the Sleep Heart Health Study. Neurology. 2008;70:35-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 293] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 16. | Walters AS, Moussouttas M, Siddiqui F, Silveira DC, Fuentes K, Wang L, Berger K. Prevalence of stroke in Restless Legs Syndrome: Initial Results Point to the Need for More Sophisticated Studies. Open Neurol J. 2010;4:73-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Koo BB, Blackwell T, Ancoli-Israel S, Stone KL, Stefanick ML, Redline S. Association of incident cardiovascular disease with periodic limb movements during sleep in older men: outcomes of sleep disorders in older men (MrOS) study. Circulation. 2011;124:1223-1231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 134] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 18. | Li Y, Walters AS, Chiuve SE, Rimm EB, Winkelman JW, Gao X. Prospective study of restless legs syndrome and coronary heart disease among women. Circulation. 2012;126:1689-1694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 19. | Winter AC, Schürks M, Glynn RJ, Buring JE, Gaziano JM, Berger K, Kurth T. Restless legs syndrome and risk of incident cardiovascular disease in women and men: prospective cohort study. BMJ Open. 2012;2:e000866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 20. | Lindner A, Fornadi K, Lazar AS, Czira ME, Dunai A, Zoller R, Veber O, Szentkiralyi A, Kiss Z, Toronyi E. Periodic limb movements in sleep are associated with stroke and cardiovascular risk factors in patients with renal failure. J Sleep Res. 2012;21:297-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 21. | Mirza M, Shen WK, Sofi A, Jahangir A, Mori N, Tajik AJ, Jahangir A. Frequent periodic leg movement during sleep is associated with left ventricular hypertrophy and adverse cardiovascular outcomes. J Am Soc Echocardiogr. 2013;26:783-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 22. | Szentkirályi A, Völzke H, Hoffmann W, Happe S, Berger K. A time sequence analysis of the relationship between cardiovascular risk factors, vascular diseases and restless legs syndrome in the general population. J Sleep Res. 2013;22:434-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 23. | Sforza E, Nicolas A, Lavigne G, Gosselin A, Petit D, Montplaisir J. EEG and cardiac activation during periodic leg movements in sleep: support for a hierarchy of arousal responses. Neurology. 1999;52:786-791. [PubMed] |
| 24. | Yang CK, Jordan AS, White DP, Winkelman JW. Heart rate response to respiratory events with or without leg movements. Sleep. 2006;29:553-556. [PubMed] |
| 25. | Nannapaneni S, Ramar K. Periodic limb movements during sleep and their effect on the cardiovascular system: is there a final answer? Sleep Med. 2014;15:379-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |