Published online Feb 26, 2015. doi: 10.13105/wjma.v3.i1.61
Peer-review started: October 18, 2014
First decision: December 3, 2014
Revised: December 8, 2014
Accepted: December 18, 2014
Article in press: December 19, 2014
Published online: February 26, 2015
Processing time: 94 Days and 22.8 Hours
AIM: To investigate clinical efficacy of displaced intra-articular calcaneal fracture (DIACF) following operation and nonoperation.
METHODS: Literature search was performed of PubMed and Cochrane Library by two independent authors to identify randomized controlled trials (RCTs) comparing operative vs nonoperative treatment of DIACF from inception to December 31st, 2013. RCT quality was evaluated by the modified Jadad scale. Dichotomous variables were pooled using risk ratios by review manager 5.3 software. Fixed-effects or random-effects models were adopted with P > 0.05 or P≤ 0.05 for heterogeneity tests, respectively.
RESULTS: Eight RCTs comprising 767 cases met inclusion criteria. Results revealed that more surgically treated patients could resume pre-injury job (P = 0.006). No statistical differences were found between the two groups in residual pain (P = 0.33), shoe fitting problems (P = 0.07), limited walking distance (P = 0.56) or secondary late arthrodesis (P = 0.38). However, operative treatment was associated with a higher complication rate (P = 0.003). Subgroup analyses of specific complications revealed that except for a higher risk of superficial wound problems (P < 0.0001) in operative group, the two groups had similar complication rate in deep wound infection (P = 0.34), compartment syndrome (P = 0.46), thromboembolism (P = 0.32), reflex sympathetic dystrophy (P = 0.51) or traumatic arthritis secondary to DIACF (P = 0.43).
CONCLUSION: Current evidence demonstrates that compared with operative treatment, conservative treatment of DIACF lead to similar clinical outcomes regarding residual pain, shoe fitting, walking distance and secondary subtalar arthrodesis but a significantly lower complication rate.
Core tip: This updated meta-analysis regarding the optimal treatment of displaced intra-articular calcaneal fracture suggests that operative and nonoperative treatment have similar clinical outcomes in residual pain, shoe fitting, walking distance and secondary subtalar arthrodesis. However, operative treatment has a higher complication risk than nonoperative treatment.
-
Citation: Jiang N, Song HJ, Xie GP, Wang L, Liang CX, Qin CH, Yu B. Operative
vs nonoperative treatment of displaced intra-articular calcaneal fracture: A meta-analysis of randomized controlled trials. World J Meta-Anal 2015; 3(1): 61-71 - URL: https://www.wjgnet.com/2308-3840/full/v3/i1/61.htm
- DOI: https://dx.doi.org/10.13105/wjma.v3.i1.61
Calcaneal fracture is the most frequent tarsal fracture in the human body[1,2] and approximately 75% are intra-articular[3,4]. Since they are mostly caused by high energy trauma[4,5], the great violence delivered to the foot usually causes displaced intra-articular calcaneal fracture (DIACF).
DIACF can be treated by operation as well as by nonoperation. However, conclusions by randomized controlled trials (RCTs) comparing clinical efficacy of the two methods were conflicting. In the year 1993, Parmar et al[6] showed no significant differences regarding outcomes between operation and nonoperation. However, subsequently in 1996, Thordarson et al[7] revealed a markedly superior functional score following operative treatment. In 2002, Buckley et al[8] found the two methods had equivalent functional outcomes without stratification of the groups but that operation was superior to nonoperation only after exclusion of the data from patients who were receiving Workers’ Compensation. In 2007, Ibrahim et al[9] reported similar clinical efficacy between the two strategies after 15-year follow-up.
Likewise, conflicting conclusions also existed in published meta-analyses. In a systematic review of three RCTs in 2000, Bridgman et al[10] found slightly better benefits following operative treatment, in consistent with a meta-analysis[11] published in the same year. However, both of them recommended further investigation because they believed the evidence was not strong enough to support operative treatment. In 2005, Bajammal et al[3] indicated there was no sufficient evidence to support with certainty that operation was better than nonoperation. This was also concluded by an updated systematic review[12] in 2009. In our meta-analysis[13] of RCTs and controlled clinical trials (CCTs) in 2012, we found that the data favored operative treatment of DIACF. However, in Jan, 2013, a systematic review[14] of four RCTs and quasi-RCTs up to 2011 concluded that operation and nonoperation could achieve similar clinical efficacy while it admitted insufficiency of the evidence.
In fact, although it is still problematic whether operative or nonoperative treatment is better for DIACF, the problem is clinically significant and warrants further study. It is also one of our chief concerns after we published our preliminary finding on this topic.
To our knowledge, there have been two more RCTs[15,16] comparing operative vs nonoperative treatment of DIACF since the year 2011. In addition, we believe the inclusion of four CCTs[17-20] in our previous meta-analysis[13] might have caused a bias which could have made our conclusions less reliable. Therefore, we decided to make a new meta-analysis of only and all retrieved RCTs until the most recently comparing clinical efficacy of operative and nonoperative treatment of DIACF.
No ethics approval was acquired.
This study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement[21,22].
All RCTs comparing operative vs nonoperative treatment of DIACF were searched in electronic databases of PubMed and Cochrane library by two authors independently. A structured search was performed using the following search string: (displaced intra-articular) AND [(calcaneal fractures) OR (fractures of the calcaneus)] AND (operative OR operation OR surgical OR surgery OR conservative OR conservation). There was no restriction to publication language. The search time was set from inception to 31st December, 2013. We also consulted the references of published systematic reviews[10-12,14].
Only RCTs and quasi-RCTs that reporting operation vs nonoperation for DIACF were taken for inclusion. CCTs, cohort studies and case reports were excluded. In addition, studies that did not report the primary outcomes were also excluded.
Two independent authors viewed all titles of searched articles. Further review of article abstract was performed in those whose titles were relevant to the topic. If information from the abstract was inadequate, a full article was referred to. Disagreement on eligibility of included studies was resolved by the third author.
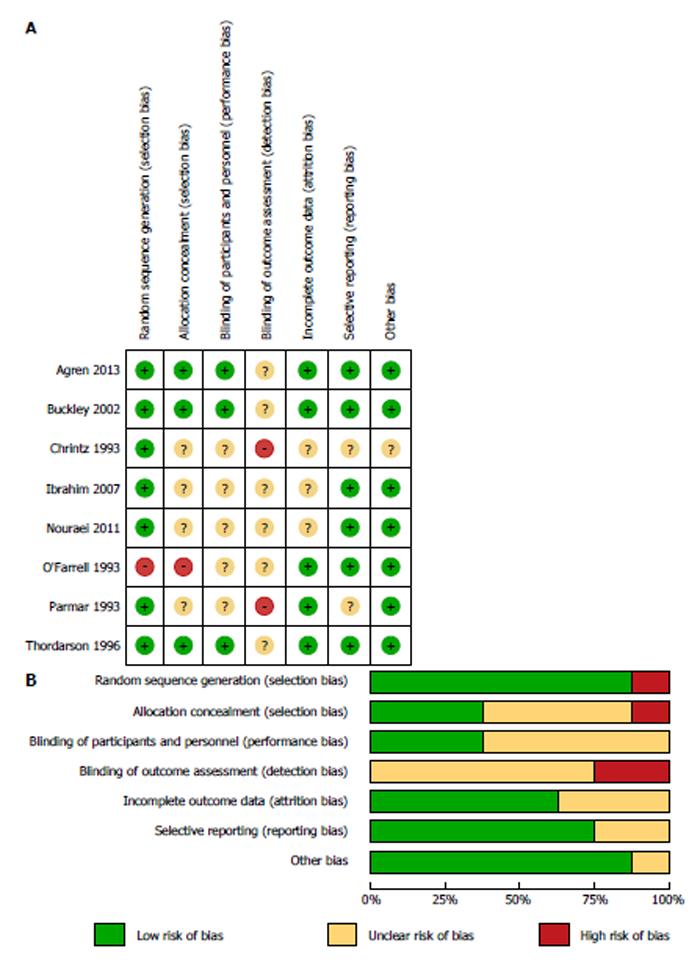
Risk-of-bias was assessed using the Cochrane Collaboration guidelines with seven items: generation of random sequence, allocation concealment, participants and personnel blinding, outcome assessment blinding, incomplete outcome data, selective reporting, and other bias graded by high, low or unclear bias risk[23].
In current study, the modified Jadad scale[24] was used to calculate the methodological scores of eligible studies. The scale includes eight items (Table 1) with scores range from 0 (lowest quality) to 8 (highest quality). The cut-off value between high quality and low quality was score 4. Scores higher than 4 mean high-quality trials while scores lower than 4 indicate low-quality trials. The methodological evaluation was performed by two independent reviewers and discrepancy was solved by discussion.
| Item assessed | Response | Score |
| Was the study described as randomized? | Yes | 1 |
| No | 0 | |
| Was the method of randomization appropriate? | Yes | 1 |
| No | -1 | |
| Not described | 0 | |
| Was the study described as blinded?1 | Yes | 1 |
| No | 0 | |
| Was the method of blinding appropriate? | Yes | 1 |
| No | -1 | |
| Not described | 0 | |
| Was there a description of withdrawals and dropouts? | Yes | 1 |
| No | 0 | |
| Was there a clear description of the inclusion/exclusion criteria? | Yes | 1 |
| No | 0 | |
| Was the method used to assess adverse effects described? | Yes | 1 |
| No | 0 | |
| Was the method of statistical analysis described? | Yes | 1 |
| No | 0 |
Two authors participated in data extraction independently. Discrepancies in outcome extraction were resolved by checking relevant studies until consensus was achieved.
Primary outcomes covered assessment of resuming pre-injury job, residual pain, shoe fitting problems, limited walking distance and secondary late arthrodesis. Secondary outcomes were complication rate and subgroup analyses for specific complications.
Statistical heterogeneity was assessed using I2 statistics, which can be calculated from the formula I2 = 100% × (Q - df)/Q, (Q represents Cochrane’s heterogeneity statistic, df represents the degrees of freedom)[25]. An I2 value of 0% means no heterogeneity, with cut-off values of 25%, 50%, 75% or more as low, moderate and high risk of heterogeneity, respectively. For outcomes of heterogeneity test when P > 0.05, a fixed-effects model was used in the meta-analysis. Otherwise, a random-effects model was adopted for P≤ 0.05. Dichotomous variables are revealed as relative risk (RR) with 95%CIs. The data syntheses and publication bias were conducted using Review Manager 5.3 software (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). The level of statistical significance was set at P value ≤ 0.05.
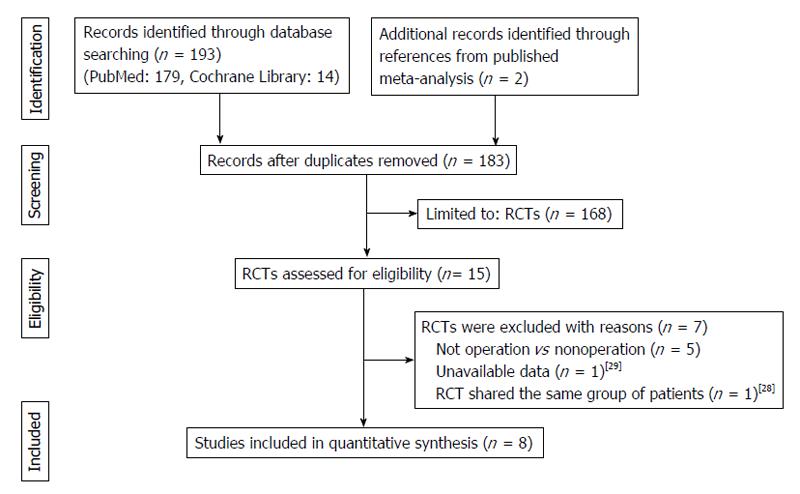
A total of 195 potentially relevant articles were identified (Figure 1). After reference to titles, abstracts and even full texts, eight published RCTs[6-9,15,16,26,27] comprising 767 patients were included for analysis. General information of eligible studies were listed in Table 2.
| Ref. | location | Cases | Sex ratio | Mean age | Follow-up time | Main outcome measures |
| (O/N) | (M/F) | (O/N) (yr) | (O/N) (yr) | |||
| Parmar et al[6] | England | 25/31 | 48/8 | 48.3/48.8 | 2.1/1.8 | Pain level, site, pattern; walking problems; shoe wear; resuming pre-injury job; deformity; ankle and subtalar movement; foot function; complications |
| O’Farrell et al[27] | Ireland | 12/12 | 20/4 | 33/38 | 1.3/1.2 | Shoe wear; pain-free walking distance; resuming pre-injury job; restoration of BÖhler angle and Gissane angle; motion range of ankle, subtalar and calcaneocuboid |
| Chrintz et al[26] | Denmark | 33/35 | NR | NR | 1.5/1.5 | Radiography outcomes |
| Thordarson et al[7] | United States | 15/11 | 21/5 | 35/36 | 1.4/1.2 | Functional assessment scale; motion rage of subtalar and ankle; gait analysis; restoration of BÖhler angle; pain; daily activity; shoe wear; walking; exercise; work; complications |
| Buckley et al[8] | Canada | 206/218 | 381/43 | 41/39 | 3.0/3.0 | Complications; SF-36 scale; VAS; shoe wear; numbness |
| Ibrahim et al[9] | United Kingdom | 15/11 | 21/5 | 61/58 | 15.2/14.8 | AOFAS score; FFI score; calcaneal fracture score; restoration of BÖhler angle and calcaneal height; arthritic grading of the subtalar joint |
| Nouraei et al[16] | Iran | 31/30 | NR | 46/52 | 3.0/3.0 | Motion range of ankle and subtalar; X-ray findings; width of heel; pain in walking; shoe wear; swelling of foot and ankle; reflex systematic dystrophy |
| Agren et al[15] | Sweden | 42/40 | 59/23 | 49/48 | 10 (8-12)1 | VAS; SF-36 scale; AOFAS score; OM scale; complications |
During the process of eligibility assessment, we found that the two RCTs by Buckley et al[8] and Howard et al[28] shared the same groups of patients with the same base line characteristics but reported different measures and clinical outcomes. Therefore, the two studies were regarded as one trial for analysis though the data of outcomes were extracted separately. In addition, one study[29] was excluded because of the unavailability of effective data.
Results of the bias risk was shown in Figure 2, indicating most of the eligible RCTs had low to moderate risk of bias. As revealed in Table 3, six[7-9,15,16,26] out of eight studies scored 4 or more than 4 by current rating scale, implying that most of the eligible RCTs were high quality studies. However, several problems were still existed in these studies. Firstly, none of the eligible studies provided detailed description regarding the blinding method. Moreover, most of the RCTs[6,7,9,15,16,26,27] failed to use method to assess adverse effects. In addition, some trials[6,9,16,26,27] still had problems in randomization and blinding. These disadvantages might cause biases.
| Item assessed | Parmar 1993 | O’Farrell 1993 | Chrintz 1993 | Thordarson 1996 | Buckley 2002 | Ibrahim 2007 | Nouraei 2011 | Agren 2013 |
| Was the study described as randomized? | √ | × | √ | √ | √ | √ | √ | √ |
| Was the method of randomization appropriate? | ? | ? | ? | √ | √ | ? | ? | √ |
| Was the study described as blinded? | × | × | × | √ | √ | × | × | √ |
| Was the method of blinding appropriate? | ? | ? | ? | ? | ? | ? | ? | ? |
| Was there a description of withdrawals and dropouts? | × | √ | √ | √ | √ | √ | √ | √ |
| Was there a clear description of the inclusion/exclusion criteria? | × | × | √ | √ | √ | √ | √ | √ |
| Was the method used to assess adverse effects described? | × | × | × | × | √ | × | × | × |
| Was the method of statistical analysis described? | √ | √ | √ | √ | √ | √ | √ | √ |
| Total score | 2 | 2 | 4 | 5.5 | 6.5 | 4 | 4 | 5.5 |
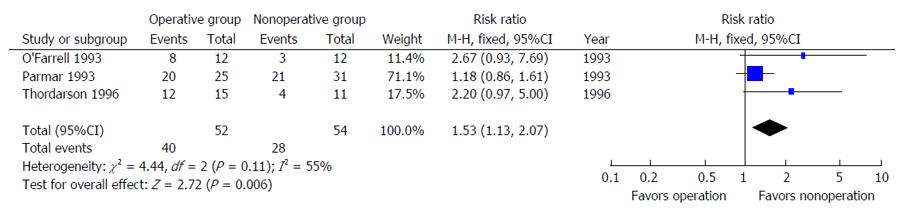
Primary outcomes: As shown in Figure 3, 40 of 52 patients after operation compared with 28 of 54 patients after conservative treatment successfully resumed pre-injury work after treatment. No statistically significant difference was found between the two groups [RR = 1.53, 95%CI: (1.13, 2.07), P = 0.006].
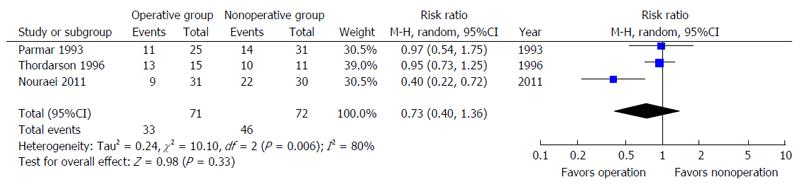
Three RCTs[6,7,16] compared the number of patients who had residual pain during the follow-up period. But no statistical difference was identified [RR = 0.73, 95%CI: (0.40, 1.36), P = 0.33] (Figure 4).
With regard to shoe fitting problems after treatment, outcome based on six RCTs[6-8,15,16,27] indicated similar efficacy [RR = 0.61, 95%CI: (0.37, 1.04), P = 0.07] (Figure 5).
Two RCTs[6,7] reported the number of patients who had limited walking distance during follow-up time. As shown in Figure 6, no significant difference was found between operation and nonoperation groups [RR = 0.88, 95%CI: (0.57, 1.36), P = 0.56].
During the follow-up period, 12 of 248 surgically treated patients compared with 41 of 258 nonsurgically treated patients had secondary late arthrodesis. However, no significant group difference was identified [RR = 0.46, 95%CI: (0.08, 2.64), P = 0.38] (Figure 7).
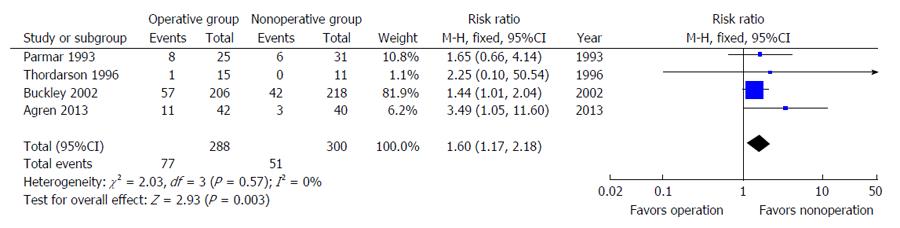
Secondary outcomes: A total of 77 of 288 surgically treated patients compared with 51 of 300 nonsurgically treated patients had complications (26.74% vs 17.0%). The significant difference indicated a higher complication risk in operative group [RR = 1.60, 95%CI: (1.17, 2.18), P = 0.003] (Figure 8).
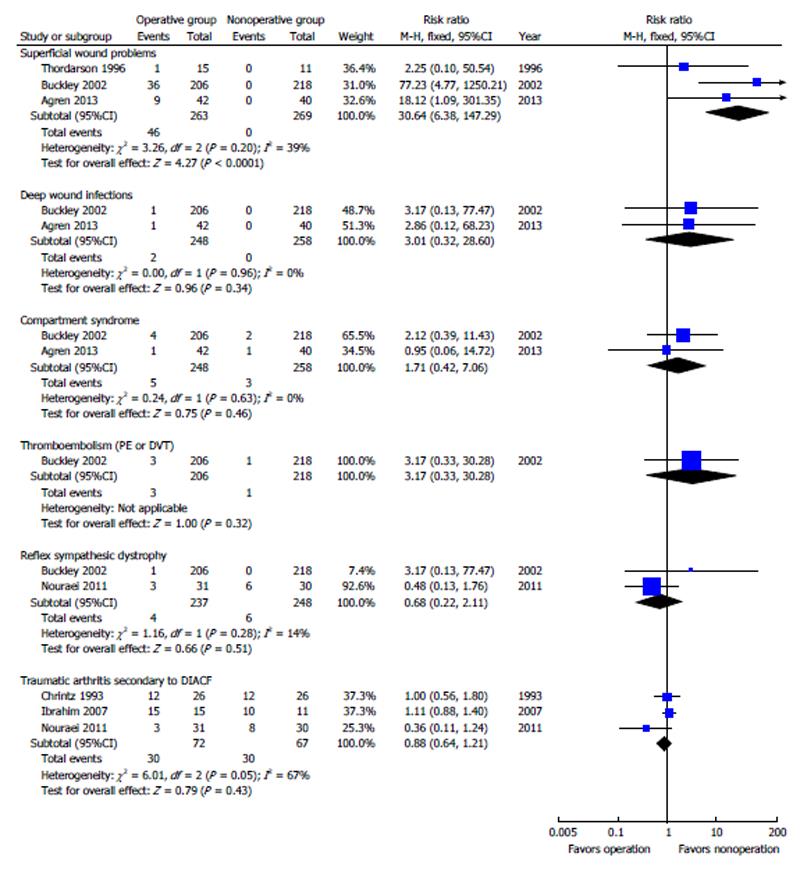
Subgroup analyses were performed to explore further differences between the two approaches regarding the specific complications. As revealed in Figure 9, except for a higher risk of superficial wound problems [RR = 30.64, 95%CI: (6.38, 147.29), P < 0.0001) after operative treatment, no significant differences were found in deep wound infection [RR = 3.01, 95%CI: (0.32, 28.60), P = 0.34], compartment syndrome [RR = 1.71, 95%CI: (0.42, 7.06), P = 0.46], thromboembolism [RR = 3.17, 95%CI: (0.33, 30.28), P = 0.32], reflex sympathetic dystrophy [RR = 0.68, 95%CI: (0.22, 2.11), P = 0.51] or traumatic arthritis secondary to DIACF [RR = 0.88, 95%CI: (0.64, 1.21), P = 0.43].
Sensitivity analysis: Sensitivity analysis was performed by excluding studies with Jadad score lower than 4. As shown in Table 3, we excluded two studies[6,27] of score < 4 and performed another meta-analysis. P values for outcome measures of residual pain, shoe fitting problems, limited walking distance and complications remained unchanged (Table 4). However, after excluding low quality studies[6,27], outcome regarding the number of patients who resumed pre-injury job showed insignificant difference between operative and nonoperative treatment (Table 4).
| Outcomes | All eligible RCTs included | Only high score RCTs included | ||||||||
| n | Patients | I2 | RR (95%CI) | P values | n | Patients | I2 | RR (95%CI) | P values | |
| Resume pre-injury job | 3 | 106 | 55% | 1.53 (1.13, 2.07) | 0.006 | 1 | 26 | NA | 2.20 (0.97, 5.00) | 0.06 |
| Residual pain | 3 | 143 | 80% | 0.73 (0.40, 1.36) | 0.33 | 2 | 87 | 93% | 0.63 (0.19, 2.11) | 0.45 |
| Shoe fitting problems | 6 | 667 | 63% | 0.61 (0.37, 1.04) | 0.07 | 4 | 587 | 73% | 0.57 (0.27, 1.21) | 0.15 |
| Limited walking distance | 2 | 82 | 71% | 0.88 (0.57, 1.36) | 0.56 | 1 | 26 | NA | 0.42 (0.16, 1.08) | 0.07 |
| Complications | 4 | 588 | 0% | 1.60 (1.17, 2.18) | 0.003 | 3 | 532 | 1% | 1.59 (1.14, 2.22) | 0.006 |
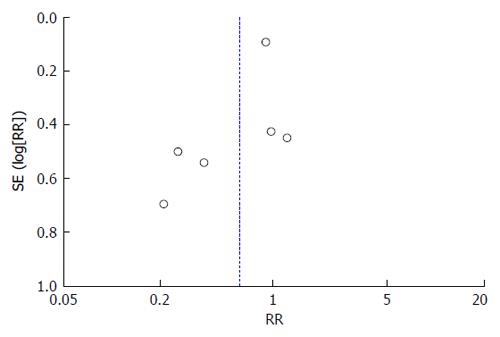
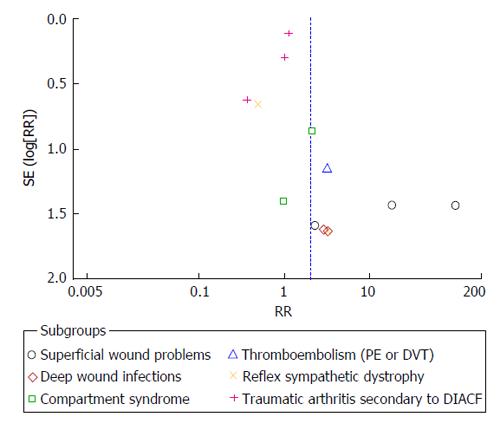
Publication bias: Publication bias was performed for incidence of shoe fitting problems and subgroup analyses of complications. Results indicated a potential publication bias of the above two outcome measures (Figures 10 and 11).
This updated meta-analysis with all retrieved RCTs suggests that compared with operative treatment, conservative treatment of DIACF can bring similar clinical outcomes regarding residual pain, shoe fitting, walking distance and secondary late arthrodesis. The only advantage following operative treatment was that more patients could resume pre-injury job after surgery. However, this superiority disappeared after sensitivity analysis by excluding low quality studies. In addition, operative treatment of DIACF elevated the risk of complications. Outcomes of the present study were different from historical meta-analyses, which was mainly because the inclusion of updated RCTs as well as only inclusion of RCTs for analysis.
The present study based on three RCTs[6,7,27] showed that more surgically treated patients could resume pre-injury job. However, Bruce et al[14] indicated that no significant differences were identified between operation and nonoperation, neither in returning to the same work nor to any work. Although result of the sensitivity analysis also revealed no statistical difference, cautious attitude should be taken due to the following two reasons. On one hand, only one RCT was left for the analysis, making the outcome less reliable. On the other hand, different workload may also affect the result. Just as Buckley et al[8] analyzed, light or moderate workload might lead to better recovery from DIACF, but patients with heavy workload were unlikely to recover well regardless of treatment strategies.
No significant difference was identified regarding the number of patients with residual pain between the two methods. But the heterogeneity among the eligible studies was high (I2 = 80%, P = 0.006), which was probably associated with several factors, such as pain tolerance, fracture type and analgesic strategy. Quite different from our previous study[13] of fewer shoe-wear problems in the operative group, the present study revealed no statistical difference between the two groups, which was probably because of the inclusion of two additional RCTs[8,15]. Howard et al[28] found no significant differences between the two approaches in the number of patients who required shoe-wear modifications at 2 wk, 6 wk, 3 mo, 1 year, 2 years or more than 2 years, respectively. Agren et al[15] reported the incidence of shoe-wear problems following operation and nonoperation was 23% and 19%. However, the authors of the two studies[15,28] did not give possible reasons for their findings.
The pooled result regarding the number of patients who had limited walking distance based on two RCTs[6,7] showed insignificant difference between operation and nonoperation. Parmar et al[6] only listed the percentage of patients without limited walking distance and did not provide the precise definition of the distance. Thordarson et al[7] defined the distance as six blocks. Therefore, the lack of consistent definition of limited walking distance might account for the high heterogeneity of included studies (I2 = 71%, P = 0.06). With respect to the number of patients who had secondary late arthrodesis, outcome based on two studies[8,15] also revealed no statistical difference. One RCT[28] reported the incidence of arthrodesis in nonoperative group was significantly higher than operative group [16% vs 3%, RR = 0.20, 95%CI: (0.09, 0.44), P < 0.0001]. This was probably because the calcaneal geometry was comparatively better preserved after operation[30]. However, Agren et al[15] reported the arthrodesis rates for operative and nonoperative managements were 12% and 10%, respectively [RR = 1.19, 95%CI: (0.34, 4.12), P = 0.78]. The authors also did not give explanations for a relatively higher incidence of arthrodesis following operative treatment. We considered it might due to the slightly larger percentage of more severe types of fracture in the operative group.
The present meta-analysis supported that surgically treated patients had a significantly higher risk of complication than those in nonsurgical group. To investigate the detailed differences of complications between the two groups, subgroup analysis was further performed on specific complications. Outcomes of the subgroup analysis implied that superficial wound problems might be the main cause of a higher complication rate after operation. Although no significant differences were identified in the number of patients who had compartment syndrome, thromboembolism or reflex sympathetic dystrophy, they need to be reported so that patients treated for DIACF are fully informed of potential complications regardless of the treatment strategy chosen. It was interesting that the incidence of traumatic arthritis secondary to DIACF was similar between the two groups (operative group of 41.67% vs nonoperative group of 44.78%). However, the outcome was based on three RCTs[9,16,26] with 139 participants, and it also might be affected by different follow-up time. Therefore, whether difference indeed exists requires more studies with adequate follow-up time.
Several scales or scores were adopted to evaluate clinical efficacy of the two methods in eligible RCTs. Ibrahim et al[9] showed that no significant differences were identified in total AOFAS score, total FFI score or calcaneal fracture score at 15 years’ follow-up time. After analyzed outcomes of SF-36 and VAS scores, Howard et al[28] concluded that the functional outcomes were partly associated with treatment strategy and partly related to the complications. Agren et al[15] used several stratified scales to show clinical efficacy at one year follow-up and at eight to twelve years’ follow-up, including visual analog scale (VAS) pain and function scoring by patients as well as by surgeon, VAS pain at rest and during weight-bearing, SF-36 physical and SF-36 mental scores, AOFAS and OM scores. However, outcomes from all these scales and scores were similar between the two methods. We did not pool these results for meta-analysis due to the following reasons: (1) not correct report form for data synthesis in meta-analysis (correct form should be mean ± standard deviation); (2) a single report; and (3) outcomes were not reported at the same follow-up time.
The main limitation of the current study might be the still limited number of eligible RCTs with limited number of participants. Although a total of eight RCTs with 767 participants was included in our study, more than half of the participants were from one study[8], which may cause a bias. In addition, the current study was purely based on a methodological standpoint, which lacks practical information regarding treatment strategies on different fracture types, especially severe and challenging injuries. Therefore, conclusions of this analysis should be interpreted with caution and more high quality RCTs are needed in the future.
In summary, the current study indicates that compared with operative treatment, conservative treatment of DIACF lead to similar clinical outcomes regarding residual pain, shoe fitting, walking distance and secondary subtalar arthrodesis but a significantly lower complication rate.
The authors thank Professor Allen P Liang for revising and editing this manuscript.
Displaced intra-articular calcaneal fracture (DIACF) can be managed by both operative and nonoperative strategies. However, up till now, controversy still exists regarding the optimal treatment of this fracture, which is mainly due to the conflicting outcomes derived from previous studies.
It is generally believed that intra-articular fractures should be treated operatively as operative management can provide better fracture reduction, promote early functional rehabilitation and reduce the rate of traumatic arthritis. However, several studies showed that conservative treatment can achieve similar functional recovery as surgery but had a lower complication risk. Therefore, whether surgery is a must for DIACF treatment requires more investigations.
Compared with previous systematic reviews or meta-analyses, the present study included more studies with high quality in methodology and thus made the outcomes more reliable. In addition, the current study once again confirmed similar clinical efficacy following operation and nonoperation.
The present study provides evidence to support conservative treatment of DIACF. However, cautious attitude should be taken towards the conclusion because of the still limited number of randomized controlled studies (RCTs) and future more high quality surveys are warranted.
Clinical RCT is a type of scientific experiment, where the people being studied are randomly allocated one or other of the different treatment methods under study. RCT is a golden standard for a clinical trial. However, the quality of an RCT is important, which will affect the reliability of the outcomes. Meta-analysis is a statistical method of combining different treatment outcomes derived from different studies to generate more conclusive and reliable conclusions.
This is a well written meta-analysis which confirms with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
P- Reviewer: Sodergren MH, Tsikouras P S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Daftary A, Haims AH, Baumgaertner MR. Fractures of the calcaneus: a review with emphasis on CT. Radiographics. 2005;25:1215-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 80] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Zwipp H, Rammelt S, Barthel S. [Calcaneal fractures--the most frequent tarsal fractures]. Ther Umsch. 2004;61:435-450. [PubMed] |
| 3. | Bajammal S, Tornetta P, Sanders D, Bhandari M. Displaced intra-articular calcaneal fractures. J Orthop Trauma. 2005;19:360-364. [PubMed] |
| 4. | Juliano P, Nguyen HV. Fractures of the calcaneus. Orthop Clin North Am. 2001;32:35-51, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Bakker B, Halm JA, Van Lieshout EM, Schepers T. The fate of Böhler’s angle in conservatively-treated displaced intra-articular calcaneal fractures. Int Orthop. 2012;36:2495-2499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Parmar HV, Triffitt PD, Gregg PJ. Intra-articular fractures of the calcaneum treated operatively or conservatively. A prospective study. J Bone Joint Surg Br. 1993;75:932-937. [PubMed] |
| 7. | Thordarson DB, Krieger LE. Operative vs. nonoperative treatment of intra-articular fractures of the calcaneus: a prospective randomized trial. Foot Ankle Int. 1996;17:2-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 228] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 8. | Buckley R, Tough S, McCormack R, Pate G, Leighton R, Petrie D, Galpin R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84-A:1733-1744. [PubMed] |
| 9. | Ibrahim T, Rowsell M, Rennie W, Brown AR, Taylor GJ, Gregg PJ. Displaced intra-articular calcaneal fractures: 15-year follow-up of a randomised controlled trial of conservative versus operative treatment. Injury. 2007;38:848-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 118] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 10. | Bridgman SA, Dunn KM, McBride DJ, Richards PJ. Interventions for treating calcaneal fractures. Cochrane Database Syst Rev. 2000;CD001161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Randle JA, Kreder HJ, Stephen D, Williams J, Jaglal S, Hu R. Should calcaneal fractures be treated surgically? A meta-analysis. Clin Orthop Relat Res. 2000;217-227. [PubMed] |
| 12. | Gougoulias N, Khanna A, McBride DJ, Maffulli N. Management of calcaneal fractures: systematic review of randomized trials. Br Med Bull. 2009;92:153-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | Jiang N, Lin QR, Diao XC, Wu L, Yu B. Surgical versus nonsurgical treatment of displaced intra-articular calcaneal fracture: a meta-analysis of current evidence base. Int Orthop. 2012;36:1615-1622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Bruce J, Sutherland A. Surgical versus conservative interventions for displaced intra-articular calcaneal fractures. Cochrane Database Syst Rev. 2013;1:CD008628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Agren PH, Wretenberg P, Sayed-Noor AS. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2013;95:1351-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 149] [Article Influence: 12.4] [Reference Citation Analysis (1)] |
| 16. | Nouraei MH, Moosa FM. Operative compared to non-operative treatment of displaced intra-articular calcaneal fractures. J Res Med Sci. 2011;16:1014-1019. [PubMed] |
| 17. | Järvholm U, Körner L, Thorén O, Wiklund LM. Fractures of the calcaneus. A comparison of open and closed treatment. Acta Orthop Scand. 1984;55:652-656. [PubMed] |
| 18. | Leung KS, Yuen KM, Chan WS. Operative treatment of displaced intra-articular fractures of the calcaneum. Medium-term results. J Bone Joint Surg Br. 1993;75:196-201. [PubMed] |
| 19. | Rodriguez-Merchan EC, Galindo E. Intra-articular displaced fractures of the calcaneus. Operative vs non-operative treatment. Int Orthop. 1999;23:63-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Xia S, Shi D, Wang Z, Wang X, Lu Y, Wang H, Wu Z, Zhu H. Operative versus nonoperative managements for displaced intraarticular fractures of calcaneus. Chin J Orthop Trauma. 2010;12:1089-1091. |
| 21. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13930] [Cited by in RCA: 13305] [Article Influence: 831.6] [Reference Citation Analysis (0)] |
| 22. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264-269, W64. [PubMed] |
| 23. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 24683] [Article Influence: 1763.1] [Reference Citation Analysis (3)] |
| 24. | Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, Moride Y. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement Geriatr Cogn Disord. 2001;12:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 328] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 25. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | Chrintz H, Sonne-Holm S. Radiograhic results after con–servative versus operative treatment of dislocated intraarticular fractures of calcaneus. Acta Orthopaedica Scandinavica-Supplementum. 1993;251:63-64. |
| 27. | O’Farrell DA, O’Byrne JM, McCabe JP, Stephens MM. Fractures of the os calcis: improved results with internal fixation. Injury. 1993;24:263-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 107] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 28. | Howard JL, Buckley R, McCormack R, Pate G, Leighton R, Petrie D, Galpin R. Complications following management of displaced intra-articular calcaneal fractures: a prospective randomized trial comparing open reduction internal fixation with nonoperative management. J Orthop Trauma. 2003;17:241-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 167] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 30. | Radnay CS, Clare MP, Sanders RW. Subtalar fusion after displaced intra-articular calcaneal fractures: does initial operative treatment matter? J Bone Joint Surg Am. 2009;91:541-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 104] [Article Influence: 6.5] [Reference Citation Analysis (0)] |