Published online May 26, 2014. doi: 10.13105/wjma.v2.i2.29
Revised: March 5, 2014
Accepted: April 11, 2014
Published online: May 26, 2014
Processing time: 226 Days and 16.4 Hours
AIM: To evaluate the “weekend effect” on outcomes in patient admitted on the weekend for upper gastrointestinal bleeding (UGIB).
METHODS: A comprehensive search was performed (March 2014). Studies comparing weekend and weekday endoscopy in patients with UGIB were included. All studies had at least 2 of 3 primary outcomes which included: mortality, need for surgery, time to endoscopy, endoscopy on admission day, and length of hospital stay. Three authors individually extracted data. Meta-analysis was performed using pooled estimates with odds ratio or mean difference by fixed and random effects models.
RESULTS: Eleven studies met the inclusion criteria. Patients admitted with UGIB on the weekend exhibited a statistically significant increase in mortality (OR = 1.13; 95%CI: 1.06-1.20; P < 0.01), need for surgery (OR = 2.46; 95%CI: 1.51-3.99; P < 0.01), and time to endoscopy (MD 2.68; 95%CI: 0.17-5.20; P = 0.04) as compared to patients admitted with UGIB on a weekday. Furthermore, patients with UGIB admitted on weekend experienced statistically significant less endoscopy on day of admission (OR = 0.72; 95%CI: 0.62-0.85; P < 0.01). No difference was noted between the two groups for length of hospital stay (MD -1.29; 95%CI: -3.03-0.45; P = 0.15).
CONCLUSION: A weekend effect seems to be apparent in patients with UGIB with significantly poorer outcomes.
Core tip: Patients admitted on weekends have been suggested by multiple studies to have poorer outcomes, even in those with gastrointestinal bleeding. Therefore, we conducted a meta-analysis of observational studies to examine the effect of weekend vs weekday admissions for patients with upper gastrointestinal bleeding (UGIB). We discovered that patients with UGIB admitted on weekends had higher mortality, need for surgery, and time to endoscopy compared to those admitted on weekdays. This meta-analysis demonstrates the need for policies to decrease these poorer outcomes for our weekend patients with UGIB.
-
Citation: Hinds AM, Ahmad D, Lopez KT, Matteson-Kome ML, Bechtold ML. Weekday
vs weekend endoscopy: Is there a true difference in patient outcomes? A meta-analysis. World J Meta-Anal 2014; 2(2): 29-35 - URL: https://www.wjgnet.com/2308-3840/full/v2/i2/29.htm
- DOI: https://dx.doi.org/10.13105/wjma.v2.i2.29
Emergency room visits and hospital admissions for all causes of upper gastrointestinal bleeding (UGIB) have decreased over the last ten years but still account for around (50-170)/100000 patients per year[1-8]. Mortality from UGIB is approximated between 3%-7% in recent studies[3,7], higher with variceal hemorrhage (approximately 15%)[9,10]. Timely intervention in patients presenting with active bleeds has been shown to reduce mortality[3]. Over half of patients presenting with UGIB has been shown to be from peptic ulcer disease, an increasingly common diagnosis[1,7]. Approximately $750 million spent each year on hospitalizations of patients with UGIB, leading to the importance of timely intervention to not only reduce mortality but also hospital costs[1]. Multiple medical and surgical diagnoses have been shown to have increased mortality over the weekend, leading to a term known as the “weekend effect”[1-3,11-17].
Over the past decade, studies have suggested that patients admitted on the weekend for UGIB have a higher mortality rate, length of stay, time to endoscopy, and increase in hospital costs than patients originally admitted to the hospital on weekdays, thus displaying a “weekend effect”. Multiple reasons for this weekend effect have been proposed, but no cause-effect relationship has been found to be significant[1,11,14]. The main proposed reasons for the weekend effect is the difference in staffing and access to critical procedures in an adequate amount of time; however, this issue seems to be the result of a combination of factors[1,2,18]. There have been multiple studies over the last ten years on this subject, but all have been observational studies with all but one being retrospective. No randomized controlled trial has been performed evaluating the weekend effect for patients with UGIB. Furthermore, of these observational studies, results have varied, adding the need for further examination into this issue. If a weekend effect is present, significant changes in policy must be considered to help reduce poorer outcomes in those patients admitted on the weekend with UGIB. Due to this important need for further examination and given the variation among the studies, a meta-analysis was completed comparing weekend verses weekday admission for UGIB.
A complete search of PubMed, Medline, Scopus, CINAHL and Cochrane databases was completed in March 2014. Search terms were used individually or in various combinations and included weekend endoscopy, weekday endoscopy, upper gastrointestinal bleed, upper gastrointestinal hemorrhage, variceal hemorrhage, non-variceal hemorrhage, esophagogastroduodenoscopy, peptic ulceration, duodenal ulceration, and gastric ulceration. Peer-reviewed studies that compared weekend vs weekday endoscopy with UGIB were selected and reviewed. References of relevant papers were searched as well for possible additional articles that were not identified in the original search. Three investigators reviewed all studies selected for inclusion criteria. Studies in children or in languages other than English were excluded from this meta-analysis.
All studies which met the inclusion criteria were reviewed by three investigators. All prospective and retrospective studies on weekday verses weekend endoscopy for UGIB were selected. All studies had at least 2 of 3 primary outcomes which included: Mortality, need for surgery, time to endoscopy, endoscopy on admission day, and length of hospital stay. If a study had missing data on these subjects or clarification needed to be obtained, attempts were made to contact the authors to obtain the necessary information. Data from the studies chosen were extracted by three separate investigators individually with differences being settled by mutual agreement.
The meta-analysis was performed comparing the outcomes of UGIB in weekend and weekday groups by calculating pooled estimates of mortality, need for surgery, time to endoscopy, endoscopy on admission day, and length of hospital stay by using OR or MD by fixed and random effects models. The meta-analysis was performed in accordance with the meta-analysis of observational studies in epidemiology (MOOSE) guidelines[19]. Publication bias was assessed by funnel plots. Heterogeneity among studies was assessed by calculating the I2 measure of inconsistency, which was considered significant if P value < 0.05 or I2 > 50%. If present, a sensitivity analysis was performed by eliminating one or more studies until heterogeneity was not present and results compared. RevMan 5.1 was used for statistical analysis.
The quality of studies was assessed using the Effective Public Health Practice Project (EPHPP) model[20,21]. This scale assesses study quality as strong, moderate, or weak based upon criteria ratings for selection bias, study design, confounders, blinding, data collection methods, and withdrawal and dropout descriptions. The quality of the study is based upon how many weak ratings per category (≥ 2 ratings is weak, one weak rating is moderate, and no weak ratings strong)[20,21].
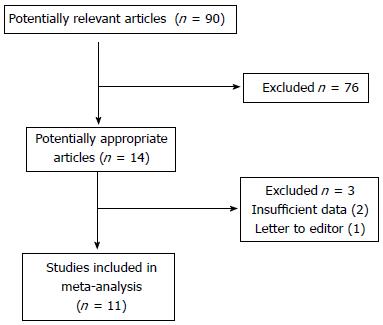
The initial search identified 90 articles through the electronic database search (Figure 1). Of these articles, 14 relevant peer-reviewed articles in English were selected for full-text review by three independent authors (AH, DA, MB). Of these studies, one article was found to be a letter to the editor and two articles had insufficient data for analysis. Therefore, 11 studies were identified that met the inclusion criteria and were included in the meta-analysis[1-4,8-11,14,18,22]. Of the 11 studies included (N = 870824), 10 were retrospective cohorts[1-3,8-11,14,18,22] and one was a prospective cohort[4]. The studies were performed at various locations in the United States and Europe and were published between 2004 and 2012. All studies examined the impact of weekend admissions on UGIB outcomes. Table 1 shows the details of the selected studies. Based upon the EPHPP model for quality assessment of studies, one study[4] was considered strong, eight studies[1-3,10,11,14,18,22] considered moderate, and two studies[8,9] considered weak. Table 2 given that all studies were retrospective except one, blinding and withdrawals/dropout description were not applicable. The study by de Groot et al[4] was the only prospective study.
| Ref. | Study type | Location | Time | # of Pts | Group | Pts/Group |
| Youn et al[3] | Retrospective | South Korea | 1/07-12/09 | 388 | Weekend | 62 |
| 4 centers | Weekday | 326 | ||||
| de Groot et al[4] | Prospective | The Netherlands | 10/09-9/11 | 571 | Weekend | 167 |
| 8 centers | Weekday | 404 | ||||
| Byun et al[9] | Retrospective | South Korea | 1/05-2/09 | 294 | Weekend | 74 |
| 1 center | Weekday | 220 | ||||
| Jairath et al[11] | Retrospective | United Kingdom | 5/07-6/07 | 6749 | Weekend | 1499 |
| 212 centers | Weekday | 5250 | ||||
| Button et al[22] | Retrospective | Wales | 4/99-3/07 | 24421 | Weekend | 5686 |
| 22 centers | Weekday | 18285 | ||||
| Dorn et al[18] | Retrospective | United States | 1998-2003 | 98975 | Weekend | 23339 |
| NIS database | Weekday | 75636 | ||||
| Shaheen et al[1] | Retrospective | United States | 1993-2005 | 237412 | Weekend | 57270 |
| NIS database | Weekday | 180142 | ||||
| Myers et al[10] | Retrospective | United States | 1998-2005 | 36734 | Weekend | 9237 |
| NIS database | Weekday | 27497 | ||||
| Ananthakrishnan et al[2] | Retrospective | United States | 2004 | 419939 | Weekend | 97002 |
| NIS database | Weekday | 322937 | ||||
| Bell et al[14] | Retrospective | Canada | 4/88-3/97 | 45167 | Weekend | 3602 |
| 190 centers | Weekday | 41565 | ||||
| Haas et al[8] | Retrospective | United States | 1/08-10/08 | 174 | Weekend | 50 |
| 1 center | Weekday | 124 |
| Ref. | Selection bias | Study design | Confounders | Blinding | Data collection method | Withdrawals and dropouts | Overall assessment |
| Youn et al[3] | Moderate | Moderate | Weak | N/A | Strong | N/A | Moderate |
| de Groot et al[4] | Strong | STRONG | Moderate | N/A | Strong | Strong | Strong |
| Byun et al[9] | Weak | Moderate | Weak | N/A | Strong | N/A | Weak |
| Jairath et al[11] | Strong | Moderate | Weak | N/A | Strong | N/A | Moderate |
| Button et al[22] | Strong | Moderate | Weak | N/A | Strong | N/A | Moderate |
| Dorn et al[18] | Strong | Moderate | Weak | N/A | Strong | N/A | Moderate |
| Shaheen et al[1] | Strong | Moderate | Weak | N/A | Strong | N/A | Moderate |
| Myers et al[10] | Strong | Moderate | Weak | N/A | Strong | N/A | Moderate |
| Ananthakrishnan et al[2] | Strong | Moderate | Weak | N/A | Strong | N/A | Moderate |
| Bell et al[14] | Strong | Moderate | Weak | N/A | Strong | N/A | Moderate |
| Haas et al[8] | Weak | Moderate | Weak | N/A | Strong | N/A | Weak |
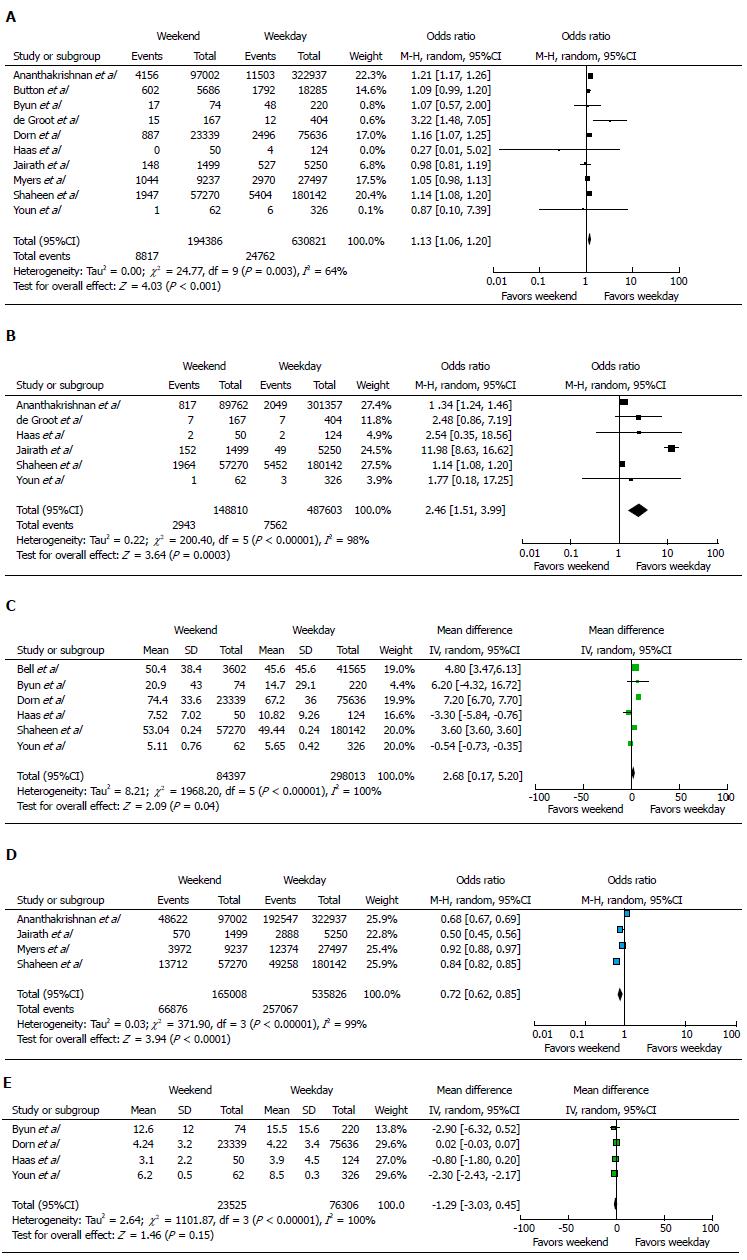
Mortality was examined in 10 studies (N = 825207)[1-4,8-11,18,22]. Mortality was noted in 8817 of 194386 (4.5%) patients with UGIB bleeding admitted on weekends and 24762 of 630821 (3.9%) patients with UGIB admitted on weekdays. A statistically significant increase in mortality was noted for those patients with UGIB admitted on the weekend as compared to those admitted on the weekdays (OR = 1.13; 95%CI: 1.06-1.20; P < 0.01). Figure 2A statistically significant heterogeneity was observed (I2 = 64%, P < 0.01). Upon sensitivity analysis, one study was eliminated[2] and revealed similar results with no significant heterogeneity (OR = 1.11; 95%CI: 1.04-1.17; P < 0.01 with I2 = 42%, P = 0.09).
The need for surgery was examined in six studies (N = 636413)[1-4,8,11]. On weekends, 2943 of 148810 (2%) patients with UGIB required surgery. On weekdays, 7562 of 487603 (1.6%) patients with UGIB required surgery. A statistically significant increase in the need for surgery was discovered in patients with UGIB admitted on weekends as compared to weekdays (OR = 2.46; 95%CI: 1.51-3.99; P < 0.01). Figure 2B statistically significant heterogeneity was observed (I2 = 98%, P < 0.01). Upon sensitivity analysis, if two studies were eliminated[1,11], no heterogeneity was noted and similar results were observed (OR = 1.35; 95%CI: 1.24-1.46; P < 0.01 with I2 = 0%, P = 0.63).
The time to endoscopy was analyzed in six studies (N = 382410)[1,3,8,9,14,18]. A statistically significant increase in the time to endoscopy was noted in patients with UGIB admitted on weekends as compared to weekdays (MD 2.68; 95% CI: 0.17-5.20; P = 0.04). Figure 2C statistically significant heterogeneity was observed (I2 = 100%, P < 0.01). Upon sensitivity analysis, if three studies were eliminated[3,8,18], no significant heterogeneity was noted and similar results were observed (OR = 3.96; 95% CI: 3.04-4.88; P < 0.01 with I2 = 41%, P = 0.19).
Endoscopy on admission day was evaluated in four studies (N = 700834)[1,2,10,11]. On weekends, 66876 of 165008 (40.5%) patients with UGIB underwent endoscopy on day of admission. On weekdays, 257067 of 535826 (48%) patients with UGIB underwent endoscopy on day of admission. A statistically significant decrease in endoscopy on day of admission was found in patients with UGIB admitted on weekends as compared to weekdays (OR = 0.72; 95%CI: 0.62-0.85; P < 0.01). Figure 2D statistically significant heterogeneity was observed (I2 = 99%, P < 0.01). Given limited number of studies for this outcome, sensitivity analysis could not be performed.
The length of hospital stay was analyzed in four studies (N = 99831)[3,8,9,18]. No statistically significant difference in the length of hospital stay was observed in patients with UGIB admitted on weekends as compared to weekdays (MD -1.29; 95%CI: -3.03-0.45; P = 0.15). Figure 2E statistically significant heterogeneity was observed (I2 = 100%, P < 0.01). Upon sensitivity analysis, if two studies were eliminated[3,18], no significant heterogeneity was noted and similar results were observed (MD -1.19; 95%CI: -2.78-0.41; P < 0.01 with I2 = 25%, P = 0.25).
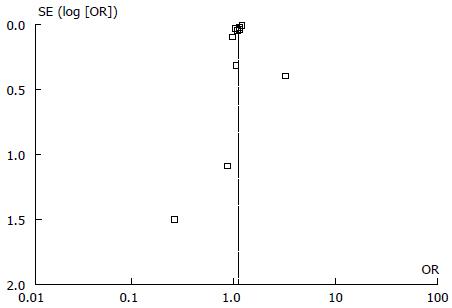
No publication bias was noted for any of the outcomes in this meta-analysis based upon funnel plots (Figure 3).
Several studies have examined the effect of a weekend hospitalization on the outcomes of patients with various medical and surgical emergencies[12-14,23]. Many of the reports provided evidence of the so-called “weekend effect”, a phenomenon in which worse outcomes have been shown in patients admitted during the weekend compared to weekdays[12-14,23]. This effect for patients admitted over the weekend has been thought to be due to lower hospital staffing, more provider workload, and sicker patients[13,15]. Patients admitted on weekends with UGIB may be impacted as well. Many studies have been performed in evaluating this “weekend effect” for patients with UGIB admitted on weekends. These studies comprise of 10 retrospective studies[1-3,8-11,14,18,22] and one prospective study[4]. Unfortunately, no randomized controlled trials have been performed on this subject, limiting the literature to a few prospective and many retrospective studies. Ananthakrishnan et al[2] conducted a respective study on patients with acute variceal hemorrhage and acute non-variceal hemorrhage (ANVH) in which the weekend effect was demonstrated in the ANVH group. In the study performed by de Groot et al[4], weekend admissions were at higher risk of adverse outcomes although the quality of care did not differ between weekday or weekend admissions. Shaheen et al[1] found that mortality and delay in endoscopy were higher in weekend admissions, but the delay in endoscopy did not appear to have affected the patient outcomes. The weekend effect was also demonstrated in studies by Dorn et al[18], Youn et al[3] and Button et al[22] studies. Four studies did not show that weekend admissions influenced in-hospital mortality in patients with UGIB[8-11]. Given the variability in results of the studies, this meta-analysis was performed.
Our meta-analysis demonstrates an increased mortality, need for surgery, and time to endoscopy in patients with UGIB admitted over the weekend as compared to being admitted on the weekday. Furthermore, patients with weekend admissions for UGIB experienced less endoscopy on admission day than those with weekday admissions. Despite these outcomes, the length of hospital stay did not differ between the two groups. Therefore, based upon these results, patients with UGIB who are admitted on the weekend appear to have poorer outcomes than those admitted on the weekday; however, evaluation of the strengths and limitations of this meta-analysis is necessary to clarify impact of results.
The strengths of our meta-analysis are numerous. First, a comprehensive article screening process with an extensive search technique was used to maximize article recognition. Second, a large number of patients in various populations were examined. Third, all of the included studies examined the impact of weekend admissions on patients with UGIB outcome. Fourth, no publication bias was noted. Finally, this represents the first meta-analysis to-date that assesses the weekend effect on patients admitted with UGIB. However, a few limitations were also observed. First, only cohort studies (retrospective and prospective) were included. However, no randomized controlled trials have been performed on this particular subject. Second, statistically significant heterogeneity was observed for all outcomes. To minimize the effect of heterogeneity, a random effects model was utilized. Also, a sensitivity analysis was performed by eliminating various studies resulting in no statistically significant heterogeneity showing similar results on all outcomes but one (endoscopy on admission day). Despite these adjustments, the results of this meta-analysis must be interpreted with some caution given the heterogeneity. Third, no abstracts were included in this meta-analysis. Due to abstracts not being peer reviewed and given the number of very large peer-reviewed studies on this subject, abstracts were deemed less quality and were not included. Fourth, selection bias may be apparent in this meta-analysis though not in traditional sense. Multiple studies utilized the same database for selection of the patients. However, search terms, such as variceal bleeding and non-variceal bleeding, and years were slightly different between the studies. Given this information and in an effort to avoid missing patients, all studies were included with the premise that a given patient may be counted twice in this meta-analysis. In conclusion, this meta-analysis demonstrates that patients with UGIB admitted on weekends have increased mortality, need for surgery, and time to endoscopy while decreased endoscopy on the admission day. Given the limitations in this meta-analysis, the results must be interpreted with caution but does strongly suggest a weekend effect is present in patients with UGIB.
The “weekend effect” showing poorer outcomes in patient admitted on the weekend rather than the weekday has been demonstrated in many different specialties. Upper gastrointestinal bleeding (UGIB) is a common reason for endoscopy and may occur any day of the week. Multiple studies have been performed evaluating the “weekend effect” in patients with UGIB requiring endoscopy with varied results.
Given the differences in the results of studies on weekend vs weekday outcomes in patients admitted with UGIB, the authors performed a meta-analysis comparing weekday to weekend admissions for UGIB to assess for mortality, need for surgery, time to endoscopy, endoscopy on admission day, and length of hospital stay.
This is the first meta-analysis comparing weekend vs weekday admissions for UGIB. The authors found that a “weekend effect” does exist with patients admitted on the weekend having increased mortality, need for surgery, and time to endoscopy while decreased endoscopy on the admission day.
Polices at local and regional levels are necessary to minimize the “weekend effect” in patients admitted with UGIB.
Odds ratio: Statistical term for the odds an event did or did not occur. Mean difference: Statistical term of difference between the means for a given variable. Heterogeneity: Test for uniformity in composition of studies included. Publication bias: Phenomenon where positive studies are more likely to be published than negative studies, leading to possible misrepresentation of data in meta-analysis.
The authors provide a study to evaluate the “weekend effect” on outcomes in patient admitted on the weekend for UGIB. This article is interesting.
P- Reviewer: Zhang LL S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clin Gastroenterol Hepatol. 2009;7:303-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 106] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Ananthakrishnan AN, McGinley EL, Saeian K. Outcomes of weekend admissions for upper gastrointestinal hemorrhage: a nationwide analysis. Clin Gastroenterol Hepatol. 2009;7:296-302e1. [PubMed] |
| 3. | Youn YH, Park YJ, Kim JH, Jeon TJ, Cho JH, Park H. Weekend and nighttime effect on the prognosis of peptic ulcer bleeding. World J Gastroenterol. 2012;18:3578-3584. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | de Groot NL, Bosman JH, Siersema PD, van Oijen MG, Bredenoord AJ. Admission time is associated with outcome of upper gastrointestinal bleeding: results of a multicentre prospective cohort study. Aliment Pharmacol Ther. 2012;36:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | van Leerdam ME, Vreeburg EM, Rauws EA, Geraedts AA, Tijssen JG, Reitsma JB, Tytgat GN. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol. 2003;98:1494-1499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 347] [Cited by in RCA: 365] [Article Influence: 16.6] [Reference Citation Analysis (37)] |
| 6. | Lanas A, García-Rodríguez LA, Polo-Tomás M, Ponce M, Quintero E, Perez-Aisa MA, Gisbert JP, Bujanda L, Castro M, Muñoz M. The changing face of hospitalisation due to gastrointestinal bleeding and perforation. Aliment Pharmacol Ther. 2011;33:585-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 124] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 7. | Laine L, Yang H, Chang SC, Datto C. Trends for incidence of hospitalization and death due to GI complications in the United States from 2001 to 2009. Am J Gastroenterol. 2012;107:1190-1195; quiz 1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 232] [Article Influence: 17.8] [Reference Citation Analysis (1)] |
| 8. | Haas JM, Gundrum JD, Rathgaber SW. Comparison of time to endoscopy and outcome between weekend/weekday hospital admissions in patients with upper GI hemorrhage. WMJ. 2012;111:161-165. [PubMed] |
| 9. | Byun SJ, Kim SU, Park JY, Kim BK, Kim do Y, Han KH, Chon CY, Ahn SH. Acute variceal hemorrhage in patients with liver cirrhosis: weekend versus weekday admissions. Yonsei Med J. 2012;53:318-327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Myers RP, Kaplan GG, Shaheen AM. The effect of weekend versus weekday admission on outcomes of esophageal variceal hemorrhage. Can J Gastroenterol. 2009;23:495-501. [PubMed] |
| 11. | Jairath V, Kahan BC, Logan RF, Hearnshaw SA, Travis SP, Murphy MF, Palmer KR. Mortality from acute upper gastrointestinal bleeding in the United kingdom: does it display a “weekend effect”? Am J Gastroenterol. 2011;106:1621-1628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Barba R, Losa JE, Velasco M, Guijarro C, García de Casasola G, Zapatero A. Mortality among adult patients admitted to the hospital on weekends. Eur J Intern Med. 2006;17:322-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Becker DJ. Do hospitals provide lower quality care on weekends? Health Serv Res. 2007;42:1589-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 14. | Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 779] [Cited by in RCA: 836] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 15. | Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117:151-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 273] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 16. | Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356:1099-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 428] [Cited by in RCA: 469] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 17. | Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke. 2007;38:1211-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 258] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 18. | Dorn SD, Shah ND, Berg BP, Naessens JM. Effect of weekend hospital admission on gastrointestinal hemorrhage outcomes. Dig Dis Sci. 2010;55:1658-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008-2012. [PubMed] |
| 20. | Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1:176-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1161] [Cited by in RCA: 1453] [Article Influence: 85.5] [Reference Citation Analysis (0)] |
| 21. | Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract. 2012;18:12-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 905] [Cited by in RCA: 1086] [Article Influence: 83.5] [Reference Citation Analysis (0)] |
| 22. | Button LA, Roberts SE, Evans PA, Goldacre MJ, Akbari A, Dsilva R, Macey S, Williams JG. Hospitalized incidence and case fatality for upper gastrointestinal bleeding from 1999 to 2007: a record linkage study. Aliment Pharmacol Ther. 2011;33:64-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 121] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 23. | Redelmeier DA, Bell CM. Weekend worriers. N Engl J Med. 2007;356:1164-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.2] [Reference Citation Analysis (0)] |