Published online Jan 12, 2023. doi: 10.13105/wjma.v11.i1.38
Peer-review started: October 15, 2022
First decision: October 31, 2022
Revised: November 11, 2022
Accepted: December 21, 2022
Article in press: December 21, 2022
Published online: January 12, 2023
Processing time: 194 Days and 12.9 Hours
Esophageal foreign bodies are common around the world. Newer approaches, such as cap-assisted endoscopy, have been introduced as an alternative to conventional methods. Therefore, we performed a meta-analysis ono cap-assisted endoscopy versus conventional endoscopy for removal of esophageal foreign bodies.
To investigated the effectiveness of cap-assisted endoscopy with conventional endoscopy.
An extensive literature search was performed (December 2021). For esophageal foreign body removal, cap-assisted endoscopy was compared to conventional endoscopy for procedure time, technical success of the procedure, time of foreign body retrieval, en bloc removal, and adverse event rate using odds ratio and mean difference.
Six studies met the inclusion criteria (n = 1305). Higher odds of technical success (P = 0.002) and en bloc removal (P < 0.01) and lower odds of adverse events (P = 0.02) and foreign body removal time (P < 0.01) were observed with cap-assisted endoscopy as compared to conventional techniques.
For esophageal foreign bodies, the technique of cap-assisted endoscopy demonstrated increased en bloc removal and technical success with decreased time and adverse events as compared to conventional techniques.
Core Tip: Esophageal foreign body impaction is very common worldwide. Many techniques have been used to treat these impactions. A newer technique of using a cap on the endoscope to assist the removal of the foreign body has been introduced. Therefore, we performed a meta-analysis. This meta-analysis showed that cap-assisted endoscopy has higher odds of technical success and en bloc removal as well as lower odds of adverse events and reduced procedure time for removal of impacted esophageal foreign bodies as compared to conventional techniques. With this information, cap-assisted endoscopy should be highly considered in removal of esophageal foreign bodies.
- Citation: Tarar ZI, Farooq U, Bechtold ML, Ghouri YA. Cap-assisted endoscopy for esophageal foreign bodies: A meta-analysis. World J Meta-Anal 2023; 11(1): 38-46
- URL: https://www.wjgnet.com/2308-3840/full/v11/i1/38.htm
- DOI: https://dx.doi.org/10.13105/wjma.v11.i1.38
Foreign body (FB) ingestion is a common gastroenterological emergency with an annual incidence of 120000 cases in the United States[1]. About 86.9% of ingested foreign bodies are lodged in the esophagus and, if left unresolved, it has been linked with the highest adverse event rate when compared to foreign bodies lodged in other parts of the gastrointestinal tract[2-4]. In majority of cases, the FB is ingested accidentally in adults while eating food, this includes impacted food bolus. In other cases, non-consumable objects are mainly ingested by individuals with an underline psychiatric disorder, social or developmental issues, alcohol abuse, or digestive diseases[5,6]. In many cases, when sharp foreign bodies, food boluses, or batteries are ingested, they may lead to complete esophageal obstruction and severe complications such as aspiration, perforation, or hemorrhage. In these cases, emergent assessment and management is warranted[2,7].
About 80%-90% of gastrointestinal foreign bodies pass spontaneously, while 10%-20% require endoscopic management and less than 1% of cases require surgery. Endoscopy has gained popularity as the preferred modality because it is not only effective in FB removal, it is also minimally invasive with low risk of adverse events[8]. Furthermore, endoscopy provides the added benefit of diagnosing other underlying gastrointestinal pathologies and obviates the need for surgical intervention[9].
A push technique can be used to mobilize an impacted FB and preferably push it distally into the stomach. Alternatively, endoscopy-assisted retrieval of the FB can be performed using special devices. Some of these devices include biopsy forceps, grasping forceps (rat-toothed or alligator type), Dormia baskets, snares, tripod graspers and retrieval nets (Roth’s type). However, more recently, endoscopic mucosal resection cap has been added to endoscopes to help remove esophageal foreign bodies more effectively[10-12]. Traditional endoscopic techniques sometime encounter poor esophageal visualization due to its narrow lumen and contrary to this, studies have reported growing evidence of better visualization of esophagus with cap-assisted endoscopy as well higher technical success and shorter procedure time[13,14].
We performed a meta-analysis of published studies comparing the technical success rate of conventional endoscopy (snares, tripod graspers, forceps, Dormia baskets, retrieval nets) vs cap-assisted endoscopy in which a cap has been used in addition to the conventional devices mentioned above. Furthermore, we investigated the FB retrieval time, adverse events rate and en bloc removal rates in both groups.
We comprehensively performed an electronic literature search of MEDLINE/PubMed, EMBASE, Scopus, Reference Citation Analysis, and Web of Science databases; from inception to December 10, 2021. The meta-analysis was conducted in accordance with the preferred reporting items for systematic review and meta-analysis (PRISMA) statement. The search terms were (esophageal foreign body impaction or food impaction or gastrointestinal foreign body ingestion, dysphagia or throat pain or soreness or foreign body sensation) and (endoscopy or endoscopic management of esophageal foreign body or use of assisted device in retrieval of foreign bodies or conventional endoscopic technique or cap-assisted endoscopy or push technique for foreign body management, use of forceps or use of basket). We also manually searched the bibliographies of the included articles to find any studies that we may have missed during our initial literature search.
Study selection was performed by two reviewers (ZIT and UF). They independently screened the abstracts, titles, and full manuscripts to identify the studies eligible for inclusion. Any conflict was resolved through discussion between the two reviewers. We included the studies published only in English, comparing the effectiveness of cap-assisted endoscopy to conventional endoscopy for management of esophageal FB in adult patients (age ≥ 18 years). Outcomes of interest were FB retrieval time, technical success of the procedure, adverse events, and en bloc removal rate.
Data was extracted by two reviewers (ZIT and UF). We extracted information about study design, country of study, study cohort characteristics, procedure performed, type of foreign bodies, rate of adverse events, time required for FB removal, difference in procedure timings, and procedure success rate. Once data was extracted, two reviewers (YG and MB) independently reviewed the extracted data sheet and final data sheet was prepared after discussion between the four reviewers.
Quality was assessed for non-randomized studies[4,14-16] using Cochrane risk of bias tool (Robin -I)[17] and randomized studies using Cochrane tool for risk of bias assessment[12,18,19].
We used RevMan 5.3 (Review Manager, Version 5.3, Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012) for statistical analysis. We calculated the mean difference and corresponding 95% confidence interval (CI) for continuous outcomes and pooled odds ratio (OR) with corresponding 95%CI for dichotomous outcomes. Random effects model was used to calculate the pooled odds ratio with 95%CI and P value < 0.05 was deemed statistically significant. The I2 statistics and Cochran’s Q test was used for heterogeneity and variance. Publication bias was assessed by funnel plots.
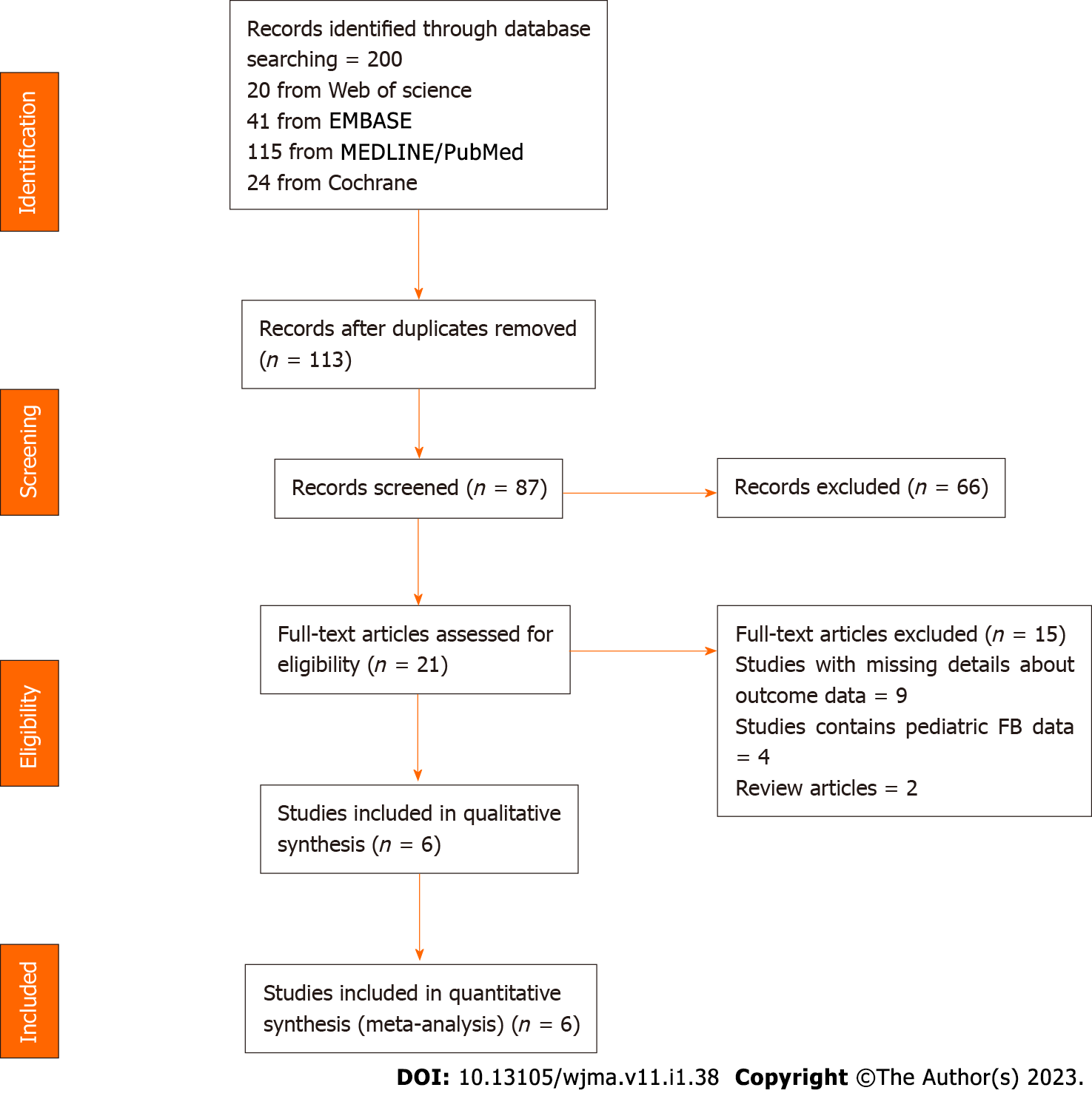
On initial literature search, we shortlisted 200 studies, of which 113 were excluded due to overlap or duplication. On further assessment, 66 studies were excluded after reviewing their respective titles and abstracts. Twenty-one papers were considered potentially relevant for our analysis, so we reviewed them in detail, out of which six[4,12,14-16,19] were included in the final meta-analysis (Figure 1). We also searched the bibliographies of the reviewed full text articles but did not find any additional study that qualified for inclusion. All the six studies included in the final analysis were retrospective, comprising of 1305 patients (636 underwent cap-assisted endoscopy, 669 underwent conventional endoscopy) (Table 1). Three studies only included the patients with food bolus impaction while the other three studies reported patients with any type of esophageal FB. The type of cap utilized differed between the studies. Three studies used an 18.1 mm diameter cap attached to the endoscope with sticky tape[4,12,16], two studies used a 11.3 mm band ligation cap14,15, and one study used an Olympus cap but did not specify the size[19]. The technique differed slightly between the studies as well. For food bolus impactions, the cap-assisted technique used on only suction with very rare use of any additional equipment (forceps, snare, or net). For foreign bodies, especially sharp bones, the cap-assisted technique often used forceps or snares in addition to suction. Lastly, although food bolus impactions were the most studied type of impaction, other impactions such as fish/chicken bones, jujube pits, and sharp objects (keys, wire, etc.) were also included in some studies.
| Ref. | Study type | Location | # of patients | Male % | Mean age conventional endoscopy | Mean age cap-assisted endoscopy | Type of FBs |
| Ooi et al[12], 2021 | RCT | Australia | 342 | 70.5 | 53.6 ± 14.7 | 54.7 ± 15.2 | Food bolus |
| Fang et al[4], 2020 | Retrospective Cohort | China | 448 | 55.4 | 62.4 ± 18.2 | 62.8 ± 16.7 | Jujube pit, fish bones, poultry bones, food bolus, other sharp objects |
| Wahba et al[15], 2019 | Prospective Cohort | Egypt | 216 | 46.2 | 52.9 | 51.7 | Food bolus |
| Ooi et al[16], 2018 | Retrospective Cohort | Australia | 199 | 69.8 | 60.8 ± 19.8 | 57.5 ± 20.2 | Food bolus |
| Zhang et al[19], 2013 | RCT | China | 70 | 58.6 | 48.9 (23-74) | 47.6 (19-73) | Fish bone, chicken bones |
| Zhang et al[14], 2010 | Retrospective cohort | China | 30 | NA | NA | NA | Fish bone, jujube pit, food bolus, coin or metal |
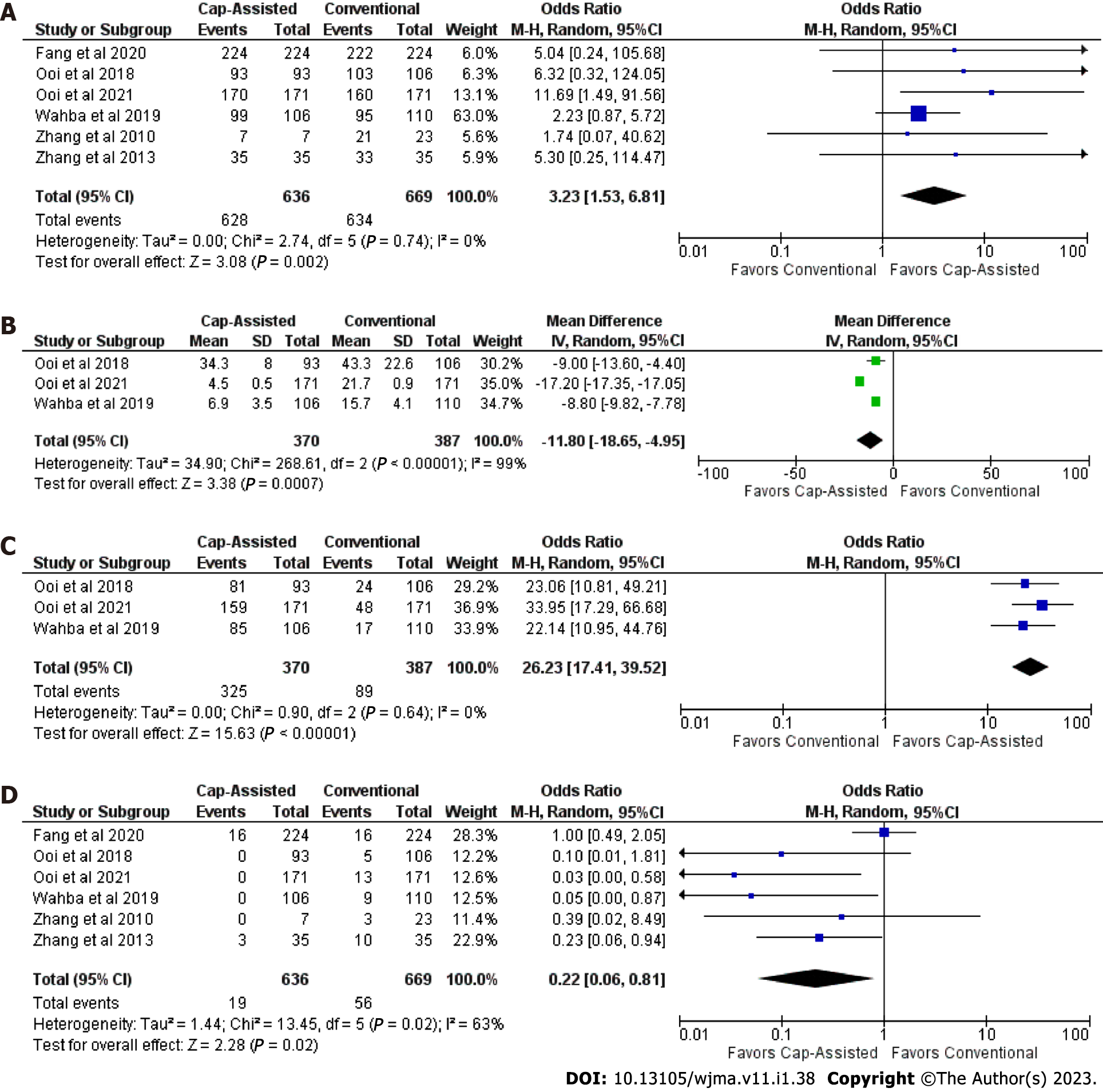
Technical success: Six studies (n = 1305) examined the technical success between cap-assisted endoscopy vs conventional endoscopy for esophageal FB removal[4,12,14-16,19]. Technical success was found in 628 of 636 with cap-assisted endoscopy but only in 634 of 669 with conventional endoscopy. Cap-assisted endoscopy demonstrated higher odds of technical success compared to conventional endoscopy (OR 3.23; 95%CI: 1.53-6.81; P = 0.002; I2 = 0%) (Figure 2A).
Foreign body retrieval time: Three studies (n = 757) provided the information about mean difference in FB retrieval time[12,15,16]. Foreign body retrieval time was significantly lower in cap-assisted endoscopy (MD -11.80 min; 95%CI: -18.65 to -4.95); P < 0.01; I2 = 99%) (Figure 2B).
En bloc removal: Three studies (n = 757) examined en bloc removal of esophageal FBs[12,15,16]. Cap-assisted endoscopy (325 of 370) was more effective in removing the FB as a single piece compared to conventional endoscopy (89 of 387). Cap-assisted endoscopy had a significantly higher pooled rate of removing FB in en bloc fashion as compared to conventional endoscopy (OR 26.23; 95%CI: 17.41-39.52; P < 0.01; I2 = 0%) (Figure 2).
Adverse events: Six studies (n = 1305) reported adverse events between the two groups[4,12,14-16,19]. Cap-assisted endoscopy demonstrated adverse events in 19 of 636 and conventional endoscopy in 56 of 669 procedures. The odds for adverse events were found to be less in cases of cap-assisted endoscopy vs conventional endoscopy (OR 0.22; 95%CI: 0.06-0.81; P = 0.02 I2 = 63% (Figure 2D).
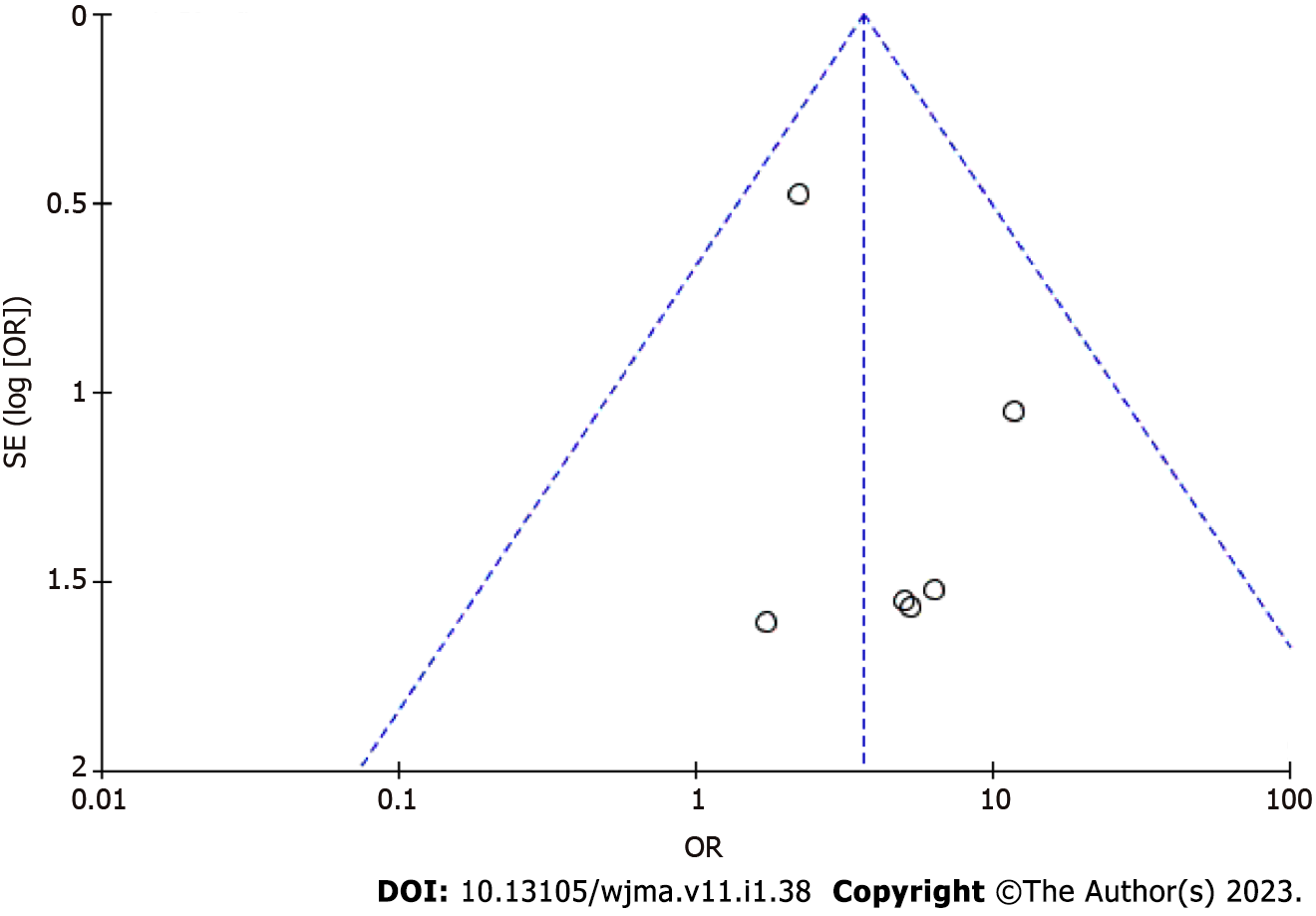
Using funnel plots, no publication bias was deemed significant in any of the outcomes (Figure 3).
Using Cochrane risk of bias tool, all studies were determined to have low risk of bias (Tables 2 and 3).
| Non-randomized studies | ||||||||
| Ref. | Confounding | Selection of participants | Classification of interventions | Deviation from interventions | Missing outcome data | Measurement of outcome | Selection of reported results | Overall |
| Zhang et al[14], 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | Low |
| Ooi et al[16], 2018 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | Low |
| Wahba et al[15], 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | Low |
| Fang et al[4], 2020 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | Low |
In the current analysis, we found that addition of a cap to the end of the endoscope in cases of esophageal foreign body impaction demonstrated significantly higher rates of technical success and en bloc removal with reduction in adverse events and time of foreign body retrieval as compared to conventional techniques. This is the first meta-analysis performed to compare the effectiveness of cap-assisted endoscopy when compared to conventional endoscopy.
In cases of esophageal foreign body impaction, 1 out of 5 requires endoscopic management[20]. Current European Society of Gastrointestinal Endoscopy recommendations are to apply gentle push technique initially to push FB into the stomach; however; if resistance is felt during pushing, a pull technique should be considered to extract the foreign body[7]. Traditionally, various endoscopic devices has been utilized, such as snares, forceps, tripod graspers, and net retrievers to remove FBs, but these methods are often time-consuming and, in most cases, the FB requires fragmentation before extraction[15]. Contrary to this, the addition of a cap allows better visualization of the narrow esophageal lumen and helps in en bloc removal of the FB by enlarging the suction area[14,21].
We found that cap-assisted endoscopy demonstrated better results for esophageal FB removal when compared to conventional endoscopy for all outcomes. Technical success of cap-assisted endoscopy was successful in 98.7% (628/636) of cases while conventional group was successful in only 94.76% (634/669) of cases. Ooi et al[12] postulated that the likely explanation for the lower success rate in conventional techniques was the failure to extract the esophageal FB in an en bloc manner which results in longer procedure times. Procedure times (recorded from the time of starting esophageal assessment with endoscopy to the extraction of FB) is shorter with the application of cap to the endoscope, likely due to the ability to remove the FB in en bloc fashion, which also causes less trauma to the surrounding tissue. Furthermore, with conventional techniques, the maneuver requires repeated removal and insertion of the attached device or endoscope which not only increases the retrieval time, but also leads to trauma of the surrounding tissue[14,16,19]. Cap-assisted endoscopy was successful in en bloc removal in 87.8% (325/370) of cases compared to 23% (89/387) of cases when conventional endoscopy was performed. En bloc retrieval is a major advantage of cap-assisted endoscopy due to strong suction applied to esophageal FB, which not only shortens the procedure time but also decreases the complication risk. Finally, adverse events in cap-assisted endoscopy were 2.98% (19/636), consisting of minor events such as mucosal tears and bleeding, while the conventional endoscopy were 8.37% (56/669). The risk of increased mucosal trauma and minor bleeding in conventional endoscopy group was likely due to the inability to remove the esophageal FB in en bloc fashion, which results in fragmentation and repeated insertion of the device.
This meta-analysis has several strengths. First, this is the first systematic review and meta-analysis that compares the efficacy of cap-assisted endoscopy with conventional endoscopy methods for esophageal FBs. Second, a thorough literature search was conducted and good quality studies were selected after establishing well-defined inclusion and exclusion criteria. Third, half of the outcomes (technical success and en bloc removal) demonstrated 0% heterogeneity. Fourth, no publication bias was identified. However, some limitations do exist. Firstly, only two of the studies were randomized controlled trials. Ideally, meta-analysis of randomized controlled trials is desired; however, the literature to-date lacks in this aspect. Furthermore, despite including retrospective studies, the quality assessment demonstrated low risk of bias. Secondly, half of the outcomes (FB retrieval time and adverse events) demonstrated significant heterogeneity. An exclusion sensitivity analysis was performed to evaluate the effect of heterogeneity on the results of these two outcomes. For FB retrieval, if Ooi et al[12] was removed, then the results were similar without heterogeneity (MD -8.81 min; 95%CI: -9.8 to -7.82; P < 0.01; I2 = 0%). For adverse events, if Fang et al[4] was excluded, then the results were similar without heterogeneity (OR 0.14; 95%CI: 0.05-0.4; P < 0.01; I2 = 0%). Therefore, heterogeneity seems to have minimal impact on the overall results.
In conclusion, our study has many clinical implications. Cap-assisted endoscopy for esophageal FB removal demonstrates higher odds of technical success and en bloc removal while reducing procedure times and adverse events. Therefore, cap-assisted endoscopy should be considered for removal of impacted esophageal foreign bodies.
Cap-assisted endoscopy for removal of esophageal foreign bodies is a new technique.
With any new technique, studies need to be performed to truly evaluate the effectiveness and adverse events.
This meta-analysis examines cap-assisted endoscopy vs conventional endoscopy for removal of esophageal foreign bodies.
An extensive literature search was conducted using multiple databases. Studies that compared cap-assisted endoscopy to conventional endoscopy for the removal of esophageal foreign bodies were included. Odds ratio or mean difference was used to analyze outcomes.
Cap-assisted endoscopy demonstrated higher odds of technical success (P = 0.002) and en bloc removal (P < 0.01) as compared to conventional techniques. Furthermore, cap-assisted endoscopy showed decreased odds of adverse events (P = 0.02) and mean time of foreign body removal (P < 0.01) as compared to conventional techniques.
Cap-assisted endoscopy should be considered as a potential first-line option for impacted esophageal foreign bodies.
Endoscopists may utilize cap-assisted endoscopy for removal of esophageal foreign bodies.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Okasha H, Egypt; Zhang JW, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Mowry JB, Spyker DA, Cantilena LR Jr, McMillan N, Ford M. 2013 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 31st Annual Report. Clin Toxicol (Phila). 2014;52:1032-1283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 390] [Cited by in RCA: 320] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 2. | Mosca S, Manes G, Martino R, Amitrano L, Bottino V, Bove A, Camera A, De Nucci C, Di Costanzo G, Guardascione M, Lampasi F, Picascia S, Picciotto FP, Riccio E, Rocco VP, Uomo G, Balzano A. Endoscopic management of foreign bodies in the upper gastrointestinal tract: report on a series of 414 adult patients. Endoscopy. 2001;33:692-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 118] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 3. | Geng C, Li X, Luo R, Cai L, Lei X, Wang C. Endoscopic management of foreign bodies in the upper gastrointestinal tract: a retrospective study of 1294 cases. Scand J Gastroenterol. 2017;52:1286-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 4. | Fang R, Cao B, Zhang Q, Li P, Zhang ST. The role of a transparent cap in the endoscopic removal of foreign bodies in the esophagus: A propensity score-matched analysis. J Dig Dis. 2020;21:20-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Yoo DR, Im CB, Jun BG, Seo HI, Park JK, Lee SJ, Han KH, Kim YD, Jeong WJ, Cheon GJ, Na HK, Lee JH, Choi KD, Jung KW, Kim DH, Song HJ, Lee GH, Jung HY, Gong EJ, Ahn JY. Clinical outcomes of endoscopic removal of foreign bodies from the upper gastrointestinal tract. BMC Gastroenterol. 2021;21:385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Bekkerman M, Sachdev AH, Andrade J, Twersky Y, Iqbal S. Endoscopic Management of Foreign Bodies in the Gastrointestinal Tract: A Review of the Literature. Gastroenterol Res Pract. 2016;2016:8520767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 7. | Birk M, Bauerfeind P, Deprez PH, Häfner M, Hartmann D, Hassan C, Hucl T, Lesur G, Aabakken L, Meining A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 388] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 8. | Feng S, Peng H, Xie H, Bai Y, Yin J. Management of Sharp-Pointed Esophageal Foreign-Body Impaction With Rigid Endoscopy: A Retrospective Study of 130 Adult Patients. Ear Nose Throat J. 2020;99:251-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Wang X, Su S, Chen Y, Wang Z, Li Y, Hou J, Zhong W, Wang Y, Wang B. The removal of foreign body ingestion in the upper gastrointestinal tract: a retrospective study of 1,182 adult cases. Ann Transl Med. 2021;9:502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Chauvin A, Viala J, Marteau P, Hermann P, Dray X. Management and endoscopic techniques for digestive foreign body and food bolus impaction. Dig Liver Dis. 2013;45:529-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Katsinelos P, Kountouras J, Paroutoglou G, Zavos C, Mimidis K, Chatzimavroudis G. Endoscopic techniques and management of foreign body ingestion and food bolus impaction in the upper gastrointestinal tract: a retrospective analysis of 139 cases. J Clin Gastroenterol. 2006;40:784-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 72] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Ooi M, Duong T, Holman R, Huynh D, Lafta A, Grimpen F, Appleyard M, Rayner CK, Nguyen NQ. Comparison of Cap-Assisted vs Conventional Endoscopic Technique for Management of Food Bolus Impaction in the Esophagus: Results of a Multicenter Randomized Controlled Trial. Am J Gastroenterol. 2021;116:2235-2240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Lee JS, Chun HJ, Lee JM, Hwang YJ, Kim SH, Kim ES, Jeen YT, Lee HJ. Salvage technique for endoscopic removal of a sharp fish bone impacted in the esophagus using a transparent cap and detachable snares. Korean J Gastroenterol. 2013;61:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Zhang S, Cui Y, Gong X, Gu F, Chen M, Zhong B. Endoscopic management of foreign bodies in the upper gastrointestinal tract in South China: a retrospective study of 561 cases. Dig Dis Sci. 2010;55:1305-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 15. | Wahba M, Habib G, Mazny AE, Fawzi M, Elfeki MA, Sabry S, ELbaz M, Nasr SMSE. Cap-Assisted Technique versus Conventional Methods for Esophageal Food Bolus Extraction: A Comparative Study. Clin Endosc. 2019;52:458-463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Ooi M, Young EJ, Nguyen NQ. Effectiveness of a cap-assisted device in the endoscopic removal of food bolus obstruction from the esophagus. Gastrointest Endosc. 2018;87:1198-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Sterne JAC HM, McAleenan A, Reeves BC, Higgins JPT. Assessing risk of bias in a non-randomized study. In: Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). ed. Cochrane Handbook for Systematic Reviews of Interventions version 63 (updated February 2022):chap 25. |
| 18. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 24848] [Article Influence: 1774.9] [Reference Citation Analysis (3)] |
| 19. | Zhang S, Wang J, Zhong B, Chen M, Cui Y. Transparent cap-assisted endoscopic management of foreign bodies in the upper esophagus: a randomized, controlled trial. J Gastroenterol Hepatol. 2013;28:1339-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: epidemiology and therapy. A retrospective, observational study. Gastrointest Endosc. 2001;53:193-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 161] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 21. | Soehendra N, Seewald S, Groth S, Omar S, Seitz U, Zhong Y, de Weerth A, Thonke F, Schroeder S. Use of modified multiband ligator facilitates circumferential EMR in Barrett's esophagus (with video). Gastrointest Endosc. 2006;63:847-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 90] [Article Influence: 4.7] [Reference Citation Analysis (0)] |