Published online Oct 28, 2022. doi: 10.13105/wjma.v10.i5.244
Peer-review started: June 26, 2022
First decision: July 13, 2022
Revised: July 26, 2022
Accepted: October 12, 2022
Article in press: October 12, 2022
Published online: October 28, 2022
Processing time: 123 Days and 16.9 Hours
Type 1 diabetes (DT1) in adolescents brings behavioural changes, altered nutritional habits, and eating disorders.
To identify and analyze the validated instruments that examine the disordered eating behaviour and eating disorders among adolescents with DT1.
An integrative review was accomplished based on the following databases: PubMed, LILACS, CINAHL, Scopus, Web of Science, and Reference Citation Analysis (RCA), including publications in Portuguese, English, or Spanish, without time limit and time published.
The main instruments to evaluate disordered eating behaviour were The Diabetes Eating Problem Survey-Revised, The Diabetes Eating Problem Survey, and the eating attitudes test-26, and for eating disorders the main instruments used were The Bulimic Investigation Test of Edinburgh, The Binge Eating Scale, The Child Eating Disorder Examination, The five questions of the (Sick, Control, One, Fat and Food), and The Mind Youth Questionnaire. These instruments showed an effect in evaluating risks regarding nutritional habits or feeding grievances, with outcomes related to weight control, inadequate use of insulin, and glycaemia unmanageability. We did not identify publication bias.
Around the world, the most used scale to study the risk of disordered eating behaviour or eating disorder is The Diabetes Eating Problem Survey-Revised. International researchers use this scale to identify high scores in adolescents with DT1 and a relationship with poorer glycemic control and psychological problems related to body image.
Core Tip: Adolescents with type 1 diabetes are more vulnerable to disordered eating behaviour.
- Citation: Oliveira Cunha MCS, Dutra FCS, Cavaleiro Brito LMM, Costa RF, Gaspar MWG, Sousa DF, Moura de Araújo MF, Queiroz MVO. Disordered eating behaviour and eating disorder among adolescents with type 1 diabetes: An integrative review. World J Meta-Anal 2022; 10(5): 244-254
- URL: https://www.wjgnet.com/2308-3840/full/v10/i5/244.htm
- DOI: https://dx.doi.org/10.13105/wjma.v10.i5.244
Type 1 diabetes (DT1) in adolescents brings behavioural changes, highlighting altered nutritional habits and eating disorders (ED). It is worth emphasizing that the greatest challenge of diabetes treatment is glycaemic control through insulin therapy, good nutritional habits, and regular physical activity[1], in addition to other health behaviours. However, studies about behaviours with DT1 showed a higher risk of developing ED and dissatisfaction with their body image than their pairs without diabetes[2,3].
The disordered eating behaviour (DEB) is related to active behaviouring on a diet or to feast, com
The prevalence of DEBs among adolescents is estimated at 10% in Western cultures[6]. In Israel, the estimates are 8.2% among female adolescents and 2.8% for male adolescents[7]. DEB and ED were already associated with diabetes mellitus (DM)[8,9].
ED encompass a group of psychiatric conditions that may lead to a persistent failure in attending to nutritional and metabolic needs, thus resulting in severe psychosocial impairment[10]. EDs are most prevalent among individuals with DM1 than in the average population[11].
EDs are eating disorder habits with central psychopathology related to eating, food concerns, and body image. There are four main types of ED: Anorexia nervosa, bulimia nervosa, periodic compulsive eating disorder, and specified eating or ED[12].
The knowledge of validated instruments that examined DEB and ED of adolescents with DT1 may subsidize prevention actions for potential risks to altered eating habits and the handling of grievances related to these disorders, thus supporting the decision in nursing clinical practice and other professionals that give care to adolescents with DT1. Therefore, the purpose of this study was to identify and analyze validated instruments that examined disordered eating behaviour and ED among adolescents with DT1.
This is an integrative review of the literature conducted from February to April 2021 on a single desktop machine. The PICO strategy, which represents the acronym Patient, Intervention, Comparison, and Outcomes, was used to construct the guiding question of the research. The categories of this strategy are respectively fulfilled by: “Adolescents with type 1 diabetes mellitus”; “validation studies”; and “eating disorders” and “disordered eating behaviour”. Therefore, the following question was made: What validated instruments examined the DEB or ED of adolescents with DT1?
The article selection was based on titles and abstracts of the quoted articles, with the selection of the studies’ inclusion and exclusion conditions, without establishing a temporal cut for the inclusion of studies. The inclusion conditions were as follows: Fully available articles in the electronic networks; national and international periodicals; studies regarding validated tools about disordered behaviour or eating disorder of adolescents with DT1; written in Portuguese, Spanish, or English. In contrast, the exclusion conditions were: Incomplete or incompatible texts about the subject, case reports, book chapters, monographs, review studies, editorials, stories in newspapers, or any non-scientific text.
The search for articles was done in the following databases: PubMed/Medline, LILACS, Cinahl, Scopus, Reference Citation Analysis (RCA), and Web of Science. The Periodical Portal, CAFe, from the Coordination for Improving Higher Education Personnel (CAPES), was used to access these five databases. The following Health Science Descriptors (DeCS) and (MeSH) were used: “Adolescente”, “diabetes mellitus tipo 1”, and “Transtornos da Alimentação e da Ingestão de Alimentos”, and their respective English versions are “Adolescent”, “type 1 diabetes mellitus”, and “disorders from eating and food intake”. The crossings were made using the Boolean operator “AND” to combine the descriptors: Adolescent” AND “diabetes mellitus type 1” AND “feeding and eating disorders”.
The descriptors were delimited for each selected database (Medical Subject Headings – MeSH, Health Science Descriptors – DeCS, and CINAHL Headings – MH). There was no publication year threshold. The study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations[13].
The evidence level classification regarding the guiding question concerning studies of Intervention/ Treatment or Diagnosis/Diagnostic test[14] was added and presented the following seven levels: (1) Evidence of a systematic review or a meta-analysis of all relevant randomized controlled studies; (2) evidence obtained from well-made randomized controlled studies; (3) evidence obtained from adequately designed controlled studies without randomization; (4) evidence of well-designed case-control and cohort studies; (5) evidence of systematic reviews from descriptive and qualitative studies; (6) evidence of unique descriptive or qualitative studies; and (7) evidence from authorities opinions or reports from a committee of experts.
Random effects meta-analysis of proportions was perform using the 'meta' package in R 4.0.
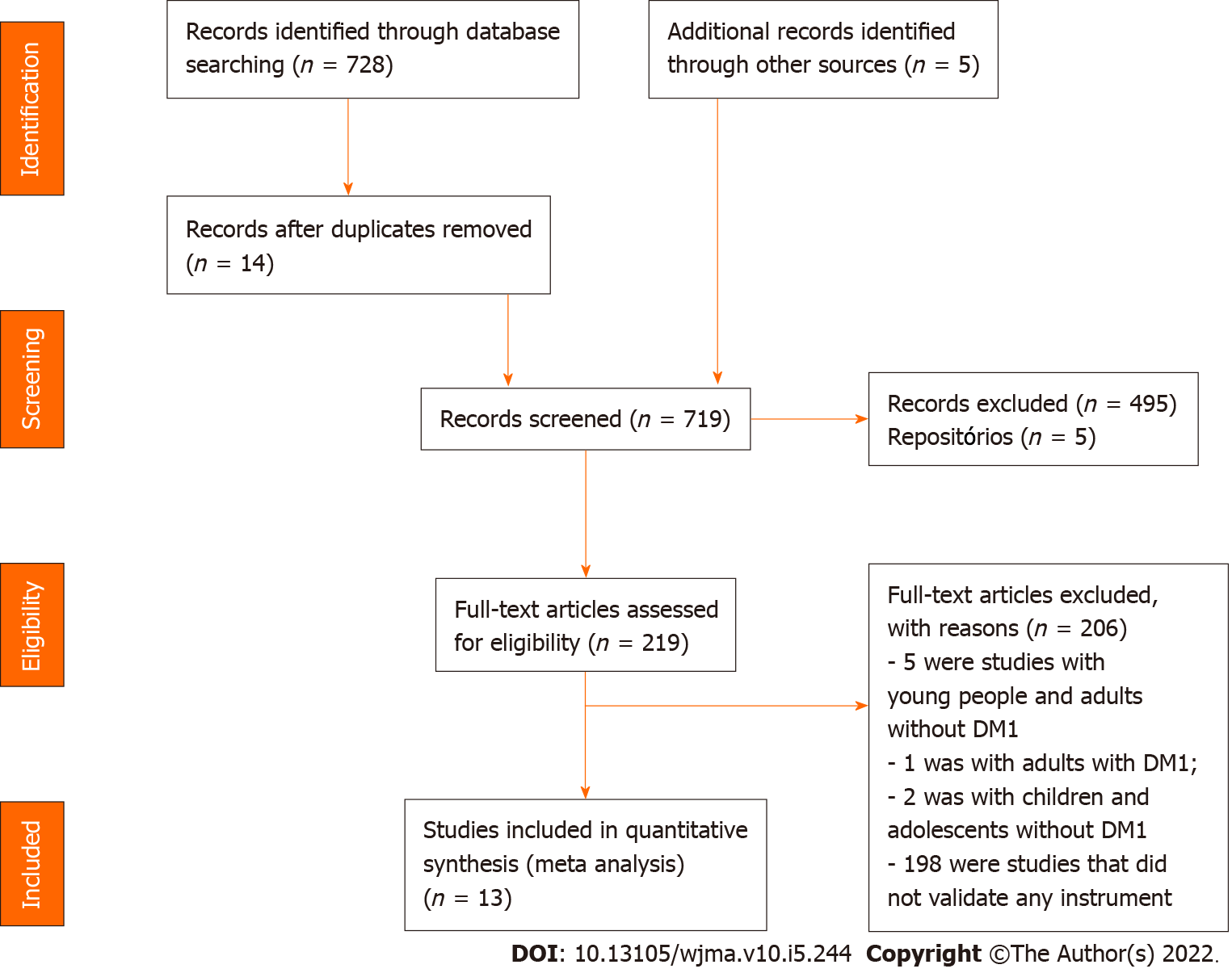
An initial search for the literature that composed the integrative review obtained a result of 728 studies, distributed in 258 articles published in PubMed/MedLine, 6 in Lilacs, 100 in Cinahl, 207 in Scopus, and 157 in Web of Science. After the application of the inclusion and exclusion conditions, the final sample was composed of 13 studies in the following databases: LILACS (1); PubMed/MedLine (4); Cinahl (2); Scopus (3); and Web of Science (3).
The stages of search and selection of studies for the review are summarized in Figure 1, which was made according to the PRISMA[13].
Thirteen studies from nine different English and non-English countries were found; two each were conducted in Norway, Italy, Canada, and Turkey. The others were published in the following countries: Brazil, United States, Germany, Netherlands, and China, each with one study. There was an intense time variation regarding the publication year, where only one study was published annually and, exceptionally, two studies in a few years. The first study was published in 2010, and the most recent in 2021. Two studies each were conducted in 2013 and 2018 and three in 2017. The other years had one study as per Table 1.
| Ref. | Title | Objective | Instrument | Conclusion | Evidence level |
| Philippi et al[20], 2013 | Risk behaviours for eating disorders in adolescents and adults with type 1 diabetes | To evaluate the frequency of risk behaviour concerning the risk of eating disorder in patients with diabetes (DT1) and its association with sex, nutritional status, variables related to DT1, and satisfaction with their body | The Eating Attitude Test (EAT-26); The Bulimic Investigation Test of Edinburgh (BITE); The Binge Eating Scale (BES) | Patients with DT1 demonstrated a high frequency of dissatisfaction with their body image and risk of an eating disorder; the omission or reduction of insulin was a significant risk factor for eating disorders | Level VI |
| Frampton et al[15], 2011 | Reliability and validity of the Norwegian translation of the Child Eating Disorder Examination (ChEDE) | To evaluate the psychometric properties of the Norwegian version of the ChEDE 12.0 | The Child Eating Disorder Examination (ChEDE) | The Norwegian version of the ChEDE has good psychometric properties and can be recommended for clinical use and in research with young people with eating disorders in Norway | Level II |
| Cherubini et al[8], 2018 | Disordered eating behaviours in adolescents with type 1 diabetes: A cross-sectional population-based study in Italy | To evaluate the association of the following factors: Clinical, metabolic, and socio-economical with disordered eating behaviour (DEB) among adolescents with DT1, tracked through the Diabetes Eating Problem Survey-Revised (DEPS-R) | TheDiabetes Eating Problem Survey-Revised (DEPS-R) | The study suggests that skipping insulin injections, little time in physical activities, having an elevated BMI, and having a family profile of low education and occupation must be considered a sign of attention for DEB among pre-adolescents and adolescents with DT1 | Level VI |
| Akgül et al[16], 2018 | Can having a sibling with type 1 diabetes cause disordered eating behaviours? | To evaluate if the risk of disordered eating behaviour (DEB) is also applied to the brother who shares the same environment | The eating attitudes test-26 (EAT-26) | Although a direct relation was not observed, the probability of having a pathological EAT-26 was higher among groups whose brothers had DT1 | Level III |
| Zuijdwijk et al[21], 2014 | The mSCOFF for Screening Disordered Eating in Pediatric Type 1 Diabetes | To validate the screening for eating disorders in female adolescents with type 1 diabetes | The five questions of (Sick, Control, One, Fat, and Food) (mSCOFF) | It is a tool that shows a great potential to track the risk of eating disorders in female adolescents with DT1 and requires validation against a gold standard | Level VI |
| Gagnon et al[17], 2017 | Psychometric Properties of the French Diabetes Eating Problem Survey Revised (DEPS-R) | To develop and examine the psychometric properties and factorial structure of a French version of the Diabetes Eating Problem Survey Revised (DEPS-R) among participants with type 1 and 2 diabetes | A French version of the Diabetes Eating Problem Survey–Revised (DEPS-R) | Although it cannot be used alone to establish a formal diagnosis of an eating disorder, the French version is a valid and reliable scale to evaluate the risk of eating disorders among patients with any type of diabetes | Level III |
| Atik Altınok et al[22], 2017 | Reliability and Validity of the Diabetes Eating Problem Survey in Turkish Children and Adolescents with Type 1 Diabetes Mellitus | To show the reliability and validity of a Turkish version of the Eating Problem Survey-Revised (DEPS-R) among children and adolescents with type 1 diabetes mellitus | The Diabetes Eating Problem Survey-Revised (DEPS-R) | Disordered eating behaviours and insulin restriction were associated with poor metabolic control. The screening tool for diabetes to DEB can be used daily during the clinical care of adolescents with DT1 | Level VI |
| Saßmann et al[23], 2015 | Psychometric properties of the German version of the Diabetes Eating Problem Survey Revised: additional benefit of disease-specific screening in adolescents with Type 1 diabetes | To examine psychometric properties of the German version of the Diabetes Eating concerning 16 items, research was performed in a sample of adolescents with type 1 diabetes | The Diabetes Eating Problem Survey Revised (DEPS-R) | The DEPS-R delivered more specific information than the tracking of generic instruments and identified more Young ones with an eating disorder than reported by the doctor, especially concerning the detection of boys at risk. The DEPS-R identifies the eating disorder in the initial stage of adolescents | Level VI |
| Wit et al[24], 2012 | Assessing the diabetes-related quality of life of youth with type 1 diabetes in routine clinical care: the MIND Youth Questionnaire (MY-Q) | To report the development and validation of the MIND Youth Questionnaire (MY-Q) among Dutch adolescents with type 1 diabetes | The MIND Youth Questionnaire (MY-Q) | The MY-Q is a survey of QVRS projected for use in clinical care. It has good measurement properties and seems adequate to implement in the daily care of adolescents with diabetes | Level VI |
| Wisting et al[19], 2013 | Psychometric Properties, Norms, and Factor Structure of the Diabetes Eating Problem Survey Revised in a Large Sample of Children and Adolescents with Type 1 Diabetes | To examine psychometric properties of the Diabetes Eating Problem Survey – Revised (DEPS-R) in a large sample of young patients with DT1 to establish rules and validate it against the Eating Attitudes Test 12 (EAT-12) | The Diabetes Eating ProblemSurvey–Revised (DEPS-R) | The DEPS-R is a useful screening tool for DEB in people with DT1, which is relevant in practical clinics. The discoveries support this important screening tool's utility in identifying eating disorders among young patients with type 1 diabetes | Level IV |
| Markowitz et al[25], 2010 | Brief Screening Tool for Disordered Eating in Diabetes | To update and validate a specific diabetes tracking tool for eating disorders (Diabetes Eating Problem Survey DEPS) in young ones with type 1 diabetes. | The Diabetes Eating ProblemSurvey-Revised (DEPS-R) | Future studies must focus on using DEPS-R to identify high-risk populations for the prevention and early intervention of disordered eating behaviours | Level VI |
| Pinna et al[26], 2017 | Assessment of eating disorders with the diabetes eating problems survey revised (DEPS-R) in a representative sample of insulin-treated diabetic patients: a validation study in Italy | To evaluate patients with type 1 and type 2 diabetes treated with insulin and the psychometric characteristics of the Italian version of the DEPS-R scale | The Diabetes Eating Problem Survey-Revised (DEPS-R) | Adults and adolescents with type 1 and type 2 diabetes treated with insulin participated in the study. The Italian version of the DEPS-R scale showed a good construct validity, internal consistency, and an excellent reasonable degree of reproducibility in this public | Level VI |
| Lv et al[18], 2021 | Instrument Context Relevance Evaluation, Translation, and Psychometric Testing of the Diabetes Eating Problem Survey-Revised (DEPS-R) among People with Type 1 Diabetes in China | To adapt the DEPS-R for Mandarin and test its psychometric properties among adolescents and adults with type 1 diabetes in China | The Diabetes Eating Problem Survey-Revised (DEPS-R) | The Chinese version of the DEPS-R described a high proportion of disordered eating behaviour among adolescents and adults with DT1, thus indicating a need for special attention by health professionals and researchers in China | Level III |
Concerning the evidence level, based on the methodological analysis of the studies, nine are descriptive studies with a quantitative approach, and four are experimental studies of the clinical trial type. Among the observational studies, nine are descriptive with a quantitative approach.
All studies varied in the evidence level among II, III, IV, and VI. Two clinical trials[15,16] were classified as level II. A clinical trial without randomization and a quasi-experimental study[17,18] were classified as level III. A cohort study[19] was classified as level IV. The other studies[8,20-26] that identified the clinical question associated with the diagnosis/diagnostic test, were classified as level VI.
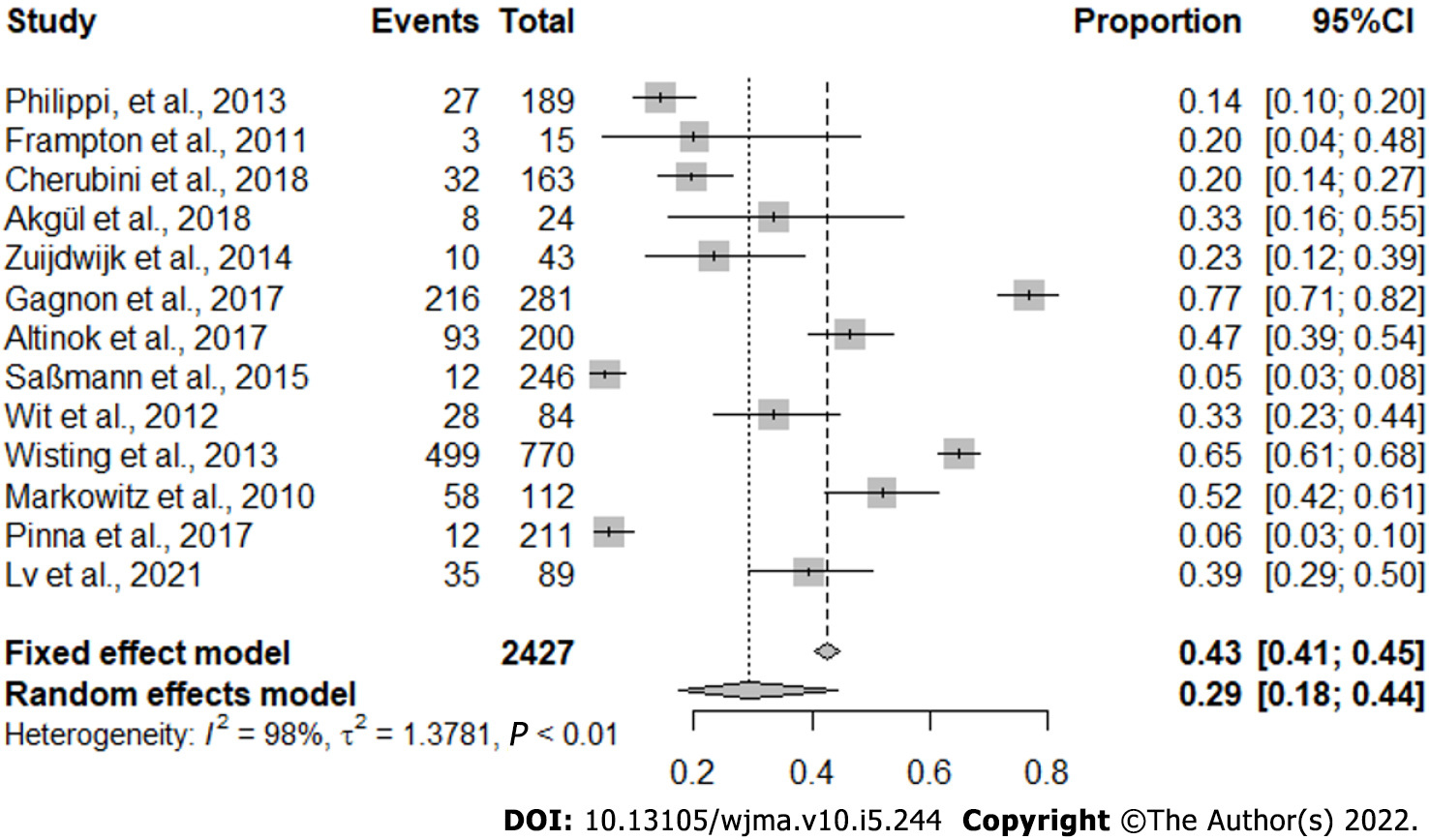
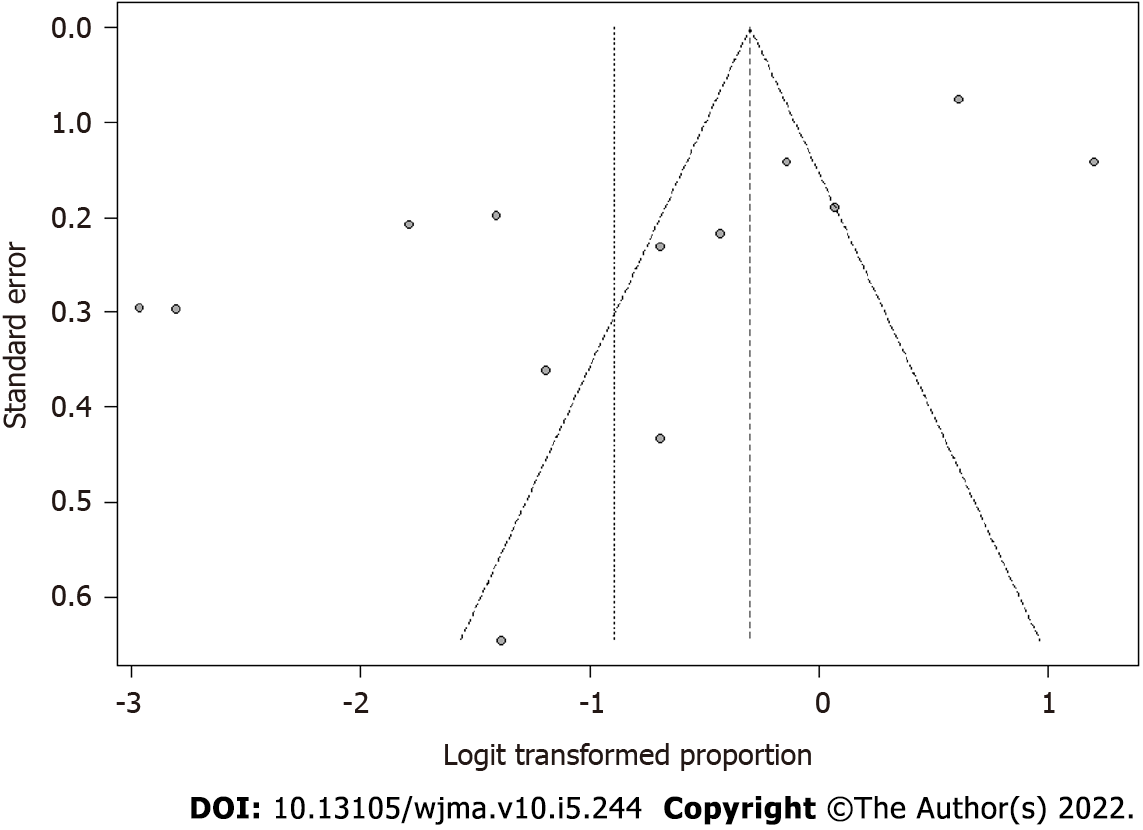
Due to the asymmetry of the points, we did not identify publication bias (Figure 2). We observed a proportion of 0.29 with a confidence interval of 0.18 to 0.44 and a significant P value representing almost 30% of the analyzed cases (Figure 3).
We have concluded that the most used psychometric scale for analyzing eating behaviour and risk for ED is The Diabetes Eating Problem Survey-Revised (DEPS-R).
Previous research showed that patients with DT1 have a higher frequency of ED and nutritional risk behaviours than the standard population[20]. For sure, these disorders contribute to an increased risk of complications from diabetes, such as abnormal lipid profiles, diabetic ketoacidosis, retinopathy, neuropathy, nephropathy, and mortality increase[11,27,28]. Therefore, evaluating these clinical conditions for follow-up and damage reduction with the subjects’ effective participation is relevant[29].
A study evaluated risks of eating disorders using the following tools: The Eating Attitude Test (EAT-26), The Bulimic Investigation Test of Edinburgh (BITE), and the Binge Eating Scale (BES). It showed that the percentages of patients at risk of eating disorders were 45% per EAT, 40% per BITE, and 16% per BES[20]. These tools evaluated a specific type of disorder. Although of great value, they are not directed to patients with DT1, but to the standard population.
Researchers affirmed that ED are characterized by significant hassles in the cognition of the body's image and morbid concern with food, weight, and shape. Adolescents, when trying to control their weight, appeal to behaviours that include self-starvation, self-induced vomit, abusive use of laxatives and diuretics, and a tremendous and significant volume of physical exercise[15].
One considers habits such as the restriction or omission of insulin as an exclusive disorder eating behaviour of people with DT1. They are usually considered boundary conditions to an eating disorder because their symptoms have yet to reach a threshold of high degree. Such conditions would be classified as an eating disorder as such[8,30].
A study involving adolescents with DT1 demonstrated that a higher body mass index (BMI) was significantly associated with a less positive body image among girls with diabetes. This data emphasizes that higher BMI is associated with low self-esteem and lower levels of social support among adolescents with diabetes, especially girls. Another addition is that worries about body image and several psychosocial factors can be forerunners to developing eating disorder symptoms[31].
Instruments capable of validating the eating disorder must be projected to combine the participants’ cognitive capacity and the adolescents’ development stage. Researchers from Norway observed that no evaluation measures for ED were available to the younger population. Therefore, they used an adaption of the EDE 12.0 tool, which is recognized as a gold standard measure of psychopathology about ED among adults[32]. For this, they adapted and evaluated the psychometric properties of the Norwegian version of the “ChEDE” for children and adolescents[15].
It is worth highlighting that adolescents with DT1 usually have a complicated state of worries around eating and diet but generally are not associated with weight and body shape issues. This finding confirms that the ChEDE tool could distinguish eating problems in this group and cognitive and behavioural psychopathology in anorexia[15].
Another study in Norway to evaluate DEB adapted and validated the DEPS-R with children and adolescents with DT1. When comparing the DEPS-R with the EAT-12, the DEPS-R seemed to be a better screening tool for DEB among young patients with DT1. In addition to the internal consistency, the DEPS-R was strongly correlated with glycated hemoglobin (HbA1c), rather than EAT-12, although both correlations were presented as relatively weak. Overall, male adolescents reported fewer DEBs than female ones[19].
Concerning the risk of ED, a study analyzed it using the mSCOFF tool, an adaptation of the SCOFF, for people with DT1. The tool mCOFF was adapted and evaluated for the risk of ED among female adolescents with DT1[21]. The researchers affirmed that when the mSCOFF tool was applied to 43 female adolescents with DT1, compared with the mEDI instrument, 10 (23.2%) participants were identified as being at high risk of developing an eating disorder[21].
In other studies that investigated ED in a similar population, the female participants presented more elevated results compared to male participants. The studies[15,21] showed these results as intrinsically connected to personal dissatisfaction with body image. Such an issue is the one the girls report the most. It is stated that the genesis and occurrence of ED can diverge between boys and girls, and the prevalence in male adolescents with DT1 is low[33].
One study highlights another tool to analyze the DEB in children and adolescents with DT1 – DEPS-R. Researchers from the USA used a DEPS adapted tool developed for adults with DT1[25]. Such specific tools for diabetes are needed due to the inefficient use of insulin and a potential purgative behaviour. These issues are seen as exclusive to individuals with diabetes[34]. The DEPS-R can avoid developing ED, such as bulimia and anorexia.
Therefore, the DEPS-R tool was adapted and validated in several countries, and a study[8] evaluated the prevalence of DEB in the region of Marche, Italy, through the use of the Italian version of the DEPS-R for the screening adolescents with DT1. The finding indicates a significantly higher prevalence (a score of ≥ 20 DEPS-R of 34.4%), among patients with overweight (65.7%). It was also identified that the participants with a score ≥ 20 in the DEPS-R had significantly higher levels of HbA1c, used higher doses of insulin, and spent less time doing physical exercise.
Researchers observed that there was no instrument planned to support health professionals in identifying DEBs in the French adult population with diabetes. Due to this, there was a need to adapt and validate the DEPS-R. Therefore, a study was performed to validate the DEPS-R tool in adolescents and adults with DT1 and DT2[17].
The study aforementioned adapted and validated the tool to compare it with the following instruments: The Eating Disorders Examination Questionnaire (EDE-Q6)[35] and Eating Disorder Inventory 2-Body (EDI-2)[36]. However, the study found significant barriers and limitations, one of which was the reduced participation of adolescents. Thus, the adults prevailed. In addition to this, different constructs of body dissatisfaction could be used to provide more empirical support for the tool The Questionnaire des Attitudes et des Comportements liés à la gestion du Diabète (QACD). This study’s innovation was the use of a tool for a heterogeneous public, where there were adolescents and adults diagnosed with DT1 and DT2[17].
The Turkish version of the DEPS-R adapted and validated this tool for children and adolescents with DT1[22]. The results have shown that 25% of the participants had a score of DEPS-R ≥ 20. Of these, most were women, and the patients with a score ≥ 20 were not adequately using their insulin to fulfill the demand from the meals at times where they ate beyond what is recommended; a few skipped the follow-up dose of insulin after overeating.
In Germany, researchers adapted and validated the DEPS-R for adolescents with DT1. They reported that the insulin restriction or its omission reported to the doctor seems not to be insufficient to the identification of ED. The disordered behaviour may come accompanied by feelings of shame and guilt, which can be a barrier for adolescents to talk about their eating behaviours[23].
For the Italian population, a study used the DEPS-R adapted and validated with patients with DT1 and DT2, aged between 13 to 55 years old, being treated with insulin. In general, 21.8% of the sample met the conditions for at least one diagnosis of DSM-5 eating disorder, and 12.8% met the conditions for at least one diagnosis of DSM-IV eating disorder[26]. Moreover, in China, a study adapted and validated the DEPS-R in adolescents aged 8 to 17 years old with DT1 and 61 adults with DT1. It was registered that the average score of C-DEPS-R was 21.0. The high risk of DEBs among adolescents in this study was 39.3%[18].
Another tool that evaluated the risk of DEB is the Eating Attitudes Test-26 (EAT-26), which had a valid, sensitive, and specific measure to detect individuals at high risk for a diagnosable eating disorder. The researchers used the tool EAT-26 in eight cases in a group of healthy brothers. Three were diagnosed with DEB, and one case with anorexia nervosa. In the control group, five cases had a pathological score, where three of these cases were diagnosed with DEB. From this control group, no case was diagnosed with an eating disorder[16].
Norwegian researchers[24] developed and validated the tool “MIND Youth Questionnaire (MY-Q)” for adolescents with DT1. The tool adopted the following domains: Family functioning, depression symptoms, and disordered eating. The multidimensional survey consists of seven subscales (social impact, country, control perceptions of diabetes, responsibility, worries, satisfaction with the treatment and body image, and eating behaviour). The results showed that the body image had a higher association with what was disclosed by the female group, in contrast to what the male group verbalized.
It was observed that the common ground of all research is the fact of applying the tools and evaluating some critical variables related to DT1, such as BMI evaluation, HbA1c, and insulin use, to ascertain the possible metabolic changes and DEB. A study[37] quoted the importance of analyzing the sociodemographic data with emphasis on the age group and sex as relevant variables to correlate with BMI and HbA1c.
Another observation is related to the age group and the type of diabetes. A study[15] explored a younger public beginning at nine years old with DT1. In contrast, another study[17] explored a younger public and adults with an age limit of 84 years old with DT2. Therefore, the tools have shown themselves as essential for identifying DEB or ED of adolescents and adults afflicted by DT1, thus possibly contributing to the prevention of possible complications related to this type of grievance.
It is essential to highlight some limitations of this review before any external generalization. The analyzed studies did not employ the same psychometric instrument in all their investigations. Overall, the authors employed four different scales, however, in the same population: Adolescents with DT1. Even though we have conducted a broad sweep of the central databases, publication bias is possible because some industry pharmaceuticals privately own some scales. In this point of view, the scales can be marketed to the public and are not necessarily published in scientific journals.
Based on the scales analyzed, we concluded that adolescents with DT1 achieve high scores that indicate risk for eating behaviour and ED. Both eating phenomena are related to variables such as female gender, BMI, and HbA1c in adolescents with DT1.
The disordered eating behaviour (DEB) is related to active behaviouring on a diet or to feast, compulsive eating, or purging (inefficient use of laxatives, diuretics, and self-induced vomit) and its frequency has become considerably higher in the last years at different parts of the world
The knowledge of validated instruments that examined DEB and eating disorders of adolescents with type 1 diabetes (DT1) may subsidize prevention actions for potential risks to altered eating habits
To identify and analyze the validated instruments that examine the DEB and eating disorders among adolescents with DT1.
This is an integrative review of the literature conducted from February to April 2021 on a single desktop machine.
We concluded that the most used psychometric scale for analyzing eating behaviour and risk for eating disorders is The Diabetes Eating Problem Survey-Revised.
Therefore, the tools have shown themselves as essential for identifying DEB or eating disorders of adolescents and adults afflicted by DT1.
Further studies should be conducted to explore the best scale to study the eating behaviour of adolescents with diabetes.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Behavioural sciences
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chrcanovic BR, Sweden; Serban D, Romania S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Sociedade Brasileira de Diabetes (SBD). Diretrizes da sociedade brasileira de diabetes 2019-2020. Editora científica. 2019 [cited 2021 Mai 17]. Available from: https://www.diabetes.org.br/profissionais/images/DIRETRIZES-COMPLETA-2019-2020.pdf. |
| 2. | Baechle C, Castillo K, Straßburger K, Stahl-Pehe A, Meissner T, Holl RW, Giani G, Rosenbauer J; German Paediatric Surveillance Unit (ESPED) and the DPV-Science Initiative. Is disordered eating behaviour more prevalent in adolescents with early-onset type 1 diabetes than in their representative peers? Int J Eat Disord. 2014;47:342-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Toni G, Berioli MG, Cerquiglini L, Ceccarini G, Grohmann U, Principi N, Esposito S. Eating Disorders and Disordered Eating Symptoms in Adolescents with Type 1 Diabetes. Nutrients. 2017;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 4. | Santana DD, Barros EG, Costa RSD, da Veiga GV. Temporal changes in the prevalence of disordered eating behaviours among adolescents living in the metropolitan area of Rio de Janeiro, Brazil. Psychiatry Res. 2017;253:64-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | da Luz FQ, Sainsbury A, Mannan H, Touyz S, Mitchison D, Hay P. Prevalence of obesity and comorbid eating disorder behaviours in South Australia from 1995 to 2015. Int J Obes (Lond). 2017;41:1148-1153. [PubMed] [DOI] [Full Text] |
| 6. | Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68:714-723. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1243] [Cited by in RCA: 1038] [Article Influence: 74.1] [Reference Citation Analysis (0)] |
| 7. | Katz B. Gender and disordered eating of adolescents in Israel. Isr J Psychiatry Relat Sci. 2014;51:137-144. [PubMed] |
| 8. | Cherubini V, Skrami E, Iannilli A, Cesaretti A, Paparusso AM, Alessandrelli MC, Carle F, Ferrito L, Gesuita R. Disordered eating behaviours in adolescents with type 1 diabetes: A cross-sectional population-based study in Italy. Int J Eat Disord. 2018;51:890-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Tokatly Latzer I, Rachmiel M, Zuckerman Levin N, Mazor-Aronovitch K, Landau Z, Ben-David RF, GrafBar-El C, Gruber N, Levek N, Weiss B, Stein D, Lerner-Geva L, Pinhas-Hamiel O. Increased prevalence of disordered eating in the dual diagnosis of type 1 diabetes mellitus and celiac disease. Pediatr Diabetes. 2018;19:749-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Wisting L, Reas DL, Bang L, Skrivarhaug T, Dahl-Jørgensen K, Rø Ø. Eating patterns in adolescents with type 1 diabetes: Associations with metabolic control, insulin omission, and eating disorder pathology. Appetite. 2017;114:226-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Colton PA, Olmsted MP, Daneman D, Farquhar JC, Wong H, Muskat S, Rodin GM. Eating Disorders in Girls and Women With Type 1 Diabetes: A Longitudinal Study of Prevalence, Onset, Remission, and Recurrence. Diabetes Care. 2015;38:1212-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 99] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 12. | Battle DE. Diagnostic and Statistical Manual of Mental Disorders (DSM). Codas. 2013;25:191-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 305] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 13. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13930] [Cited by in RCA: 13355] [Article Influence: 834.7] [Reference Citation Analysis (0)] |
| 14. | Fineout-Overholt E, Stillwell SB. Asking compelling, clinical questions. In: Melnyk BM, Fineout-Overholt, E. Evidence-based practice in nursing & healthcare. A guide to best practice. Philadelphia: Wolters Kluwer, Lippincot Williams & Wilking. 2011 [cited 2021 Mai 21]; 25-39. |
| 15. | Frampton I, Wisting L, Øverås M, Midtsund M, Lask B. Reliability and validity of the Norwegian translation of the Child Eating Disorder Examination (ChEDE). Scand J Psychol. 2011;52:196-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Akgül S, Alikaşifoğlu A, Özon A, Gönç N, Düzçeker Y, Örs S, Derman O, Kanbur N. Can having a sibling with type 1 diabetes cause disordered eating behaviours? J Pediatr Endocrinol Metab. 2018;31:711-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. |
Gagnon C, Aimé A, Bélange C. Psychometric Properties of the French Diabetes Eating Problem Survey –Revised (DEPS-R).
BAOJ Diabet. 2017;(3): 022. Available from: |
| 18. | Lv W, Zhong Q, Guo J, Luo J, Dixon J, Whittemore R. Instrument Context Relevance Evaluation, Translation, and Psychometric Testing of the Diabetes Eating Problem Survey-Revised (DEPS-R) among People with Type 1 Diabetes in China. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Wisting L, Frøisland DH, Skrivarhaug T, Dahl-Jørgensen K, Rø O. Psychometric properties, norms, and factor structure of the diabetes eating problem survey-revised in a large sample of children and adolescents with type 1 diabetes. Diabetes Care. 2013;36:2198-2202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Philippi ST, Cardoso MG, Koritar P, Alvarenga M. Risk behaviours for eating disorder in adolescents and adults with type 1 diabetes. Braz J Psychiatry. 2013;35:150-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Zuijdwijk CS, Pardy SA, Dowden JJ, Dominic AM, Bridger T, Newhook LA. The mSCOFF for screening disordered eating in pediatric type 1 diabetes. Diabetes Care. 2014;37:e26-e27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Atik Altınok Y, Özgür S, Meseri R, Özen S, Darcan Ş, Gökşen D. Reliability and Validity of the Diabetes Eating Problem Survey in Turkish Children and Adolescents with Type 1 Diabetes Mellitus. J Clin Res Pediatr Endocrinol. 2017;9:323-328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 23. | Saßmann H, Albrecht C, Busse-Widmann P, Hevelke LK, Kranz J, Markowitz JT, Marshall LF, Meurs S, de Soye IH, Lange K. Psychometric properties of the German version of the Diabetes Eating Problem Survey-Revised: additional benefit of disease-specific screening in adolescents with Type 1 diabetes. Diabet Med. 2015;32:1641-1647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 24. | de Wit M, Winterdijk P, Aanstoot HJ, Anderson B, Danne T, Deeb L, Lange K, Nielsen AØ, Skovlund S, Peyrot M, Snoek F; DAWN Youth Advisory Board. Assessing diabetes-related quality of life of youth with type 1 diabetes in routine clinical care: the MIND Youth Questionnaire (MY-Q). Pediatr Diabetes. 2012;13:638-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 25. | Markowitz JT, Butler DA, Volkening LK, Antisdel JE, Anderson BJ, Laffel LM. Brief screening tool for disordered eating in diabetes: internal consistency and external validity in a contemporary sample of pediatric patients with type 1 diabetes. Diabetes Care. 2010;33:495-500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 186] [Cited by in RCA: 227] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 26. | Pinna F, Diana E, Sanna L, Deiana V, Manchia M, Nicotra E, Fiorillo A, Albert U, Nivoli A, Volpe U, Atti AR, Ferrari S, Medda F, Atzeni MG, Manca D, Mascia E, Farci F, Ghiani M, Cau R, Tuveri M, Cossu E, Loy E, Mereu A, Mariotti S, Carpiniello B. Assessment of eating disorders with the diabetes eating problems survey - revised (DEPS-R) in a representative sample of insulin-treated diabetic patients: a validation study in Italy. BMC Psychiatry. 2017;17:262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 27. | Reinehr T, Dieris B, Galler A, Teufel M, Berger G, Stachow R, Golembowski S, Ohlenschläger U, Holder M, Hummel M, Holl RW, Prinz N. Worse Metabolic Control and Dynamics of Weight Status in Adolescent Girls Point to Eating Disorders in the First Years after Manifestation of Type 1 Diabetes Mellitus: Findings from the Diabetes Patienten Verlaufsdokumentation Registry. J Pediatr. 2019;207:205-212.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 28. | Scheuing N, Bartus B, Berger G, Haberland H, Icks A, Knauth B, Nellen-Hellmuth N, Rosenbauer J, Teufel M, Holl RW; DPV Initiative; German BMBF Competence Network Diabetes Mellitus. Clinical characteristics and outcome of 467 patients with a clinically recognized eating disorder identified among 52,215 patients with type 1 diabetes: a multicenter german/austrian study. Diabetes Care. 2014;37:1581-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 29. | International Diabetes Federation. IDF diabetes atlas [Internet]. 9th ed. Brussels: IDF; 2019 [cited 2021 Mai 26]. Available from: https://www.diabetesatlas.org. |
| 30. | Takii M, Uchigata Y, Kishimoto J, Morita C, Hata T, Nozaki T, Kawai K, Iwamoto Y, Sudo N, Kubo C. The relationship between the age of onset of type 1 diabetes and the subsequent development of a severe eating disorder by female patients. Pediatr Diabetes. 2011;12:396-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Kaminsky LA, Dewey D. The association between body mass index and physical activity, and body image, self esteem and social support in adolescents with type 1 diabetes. Can J Diabetes. 2014;38:244-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Wilson T. Assessment of binge eating. In C. G. Fairburn & G. T. Wilson (Eds.), Binge eating: Nature, assessment and treatment. New York: Guilford Press. 1993 [cited 2021 Mai 26]; 227–249. Available from: https://psycnet.apa.org/record/1993-98750-011. |
| 33. | Wisting L, Bang L, Skrivarhaug T, Dahl-Jørgensen K, Rø Ø. Adolescents with Type 1 Diabetes--The Impact of Gender, Age, and Health-Related Functioning on Eating Disorder Psychopathology. PLoS One. 2015;10:e0141386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 34. | d'Emden H, McDermott B, Gibbons K, Harris M, Cotterill A. Choosing a screening tool to assess disordered eating in adolescents with type 1 diabetes mellitus. J Diabetes Complications. 2015;29:2-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16:363-370. [PubMed] |
| 36. | Garner D, Olmstead P, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. [cited 2021 Mai 26]. International journal of eating disorders. 1983;2:15-34. [DOI] [Full Text] |
| 37. | La Banca RO, Sparapani VC, Bueno M, Costa T, Carvalho EC, Nascimento LC. Estratégias para educar jovens com diabetes mellitus tipo 1 sobre insulinoterapia: revisão sistemática. Texto Contexto Enferm. 2020;e20180338. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |