Published online Feb 28, 2022. doi: 10.13105/wjma.v10.i1.37
Peer-review started: November 22, 2021
First decision: December 10, 2021
Revised: December 17, 2021
Accepted: January 27, 2022
Article in press: January 27, 2022
Published online: February 28, 2022
Processing time: 97 Days and 16.5 Hours
Unexplained infertility (UI) is usually used for any heterosexual couple who failed to have a successful clinical pregnancy without identifying clear causes after they undergo all standard fertility tests. Evidence shows that leptin is one of the most accurate biomarkers for UI. Nevertheless, conflicting results regarding leptin levels in women with UI have been reported.
To find the serum leptin levels in women with UI.
All studies written in English and conducted before April 30, 2021 from PubMed/MEDLINE, Embase, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, Google Scholar, OpenGrey, OATD, and the infertility conference abstract were included. Studies were found eligible if they provided the mean and standard deviation of leptin for the case group and control group. The quality assessment of individual studies was evaluated using the Joanna Briggs Institute Quality Assessment Tool. Data synthesis and statistical analysis were done using STATA software version 16.
A total of 378 studies were reviewed, and just six studies that fulfilled the eligibility criteria were included in this meta-analysis. The pooled result showed that leptin levels were significantly higher in women with UI compared to fertile women, with a standardized mean difference of 0.97 (95% confidence interval: -0.49-2.43). However, heterogeneity across studies was highly significant (P < 0.00001; I2 = 98.8%).
The results of this study suggest that leptin levels are elevated in women with UI compared with fertile women; hence, leptin could be a potential biomarker for UI in women, and it may be useful for identifying women with a high risk of infertility.
Core Tip: A comprehensive systematic review and meta-analysis was conducted to find the serum leptin levels in women with unexplained infertility. Six studies were included in this meta-analysis, after passing all quality checkups. The pooled result showed that leptin levels were significantly higher in women with unexplained infertility compared to fertile women, with a standardized mean difference of 0.97. Leptin could be a potential biomarker for unexplained infertility in women, and it may be useful for identifying women with a high risk of infertility.
- Citation: Abdullah AA, Ahmed M, Oladokun A. Leptin levels in women with unexplained infertility: A systematic review and meta-analysis. World J Meta-Anal 2022; 10(1): 37-45
- URL: https://www.wjgnet.com/2308-3840/full/v10/i1/37.htm
- DOI: https://dx.doi.org/10.13105/wjma.v10.i1.37
Reproductive medicine has made many breakthroughs in the field of infertility diagnosis and treatment. Following this breakthrough, many untreated infertility cases now can be treated using one of the advanced reproduction methods such as assisted reproductive technologies[1]. Despite this, some infertility cases cannot still be diagnosed or treated using the current methods, especially in developing countries[2]. This type of infertility is widely known as unexplained infertility (UI)[3].
UI is usually used for any heterosexual couple who failed to have a successful clinical pregnancy without clear causes after they undergo all standard fertility tests[4]. Worldwide, the prevalence of UI ranges from 10% to 37%[2,5-7], and females are found to be responsible for at least 50%. The complexity of the reproductive process especially in females[8], makes it very hard to identify the source of UI. Despite this, many studies have been done to find the pathophysiologic basis and the possible relationship between obesity, endocrinological imbalance, genetic factors, immunological factors, and UI[7,9,10], but unfortunately, till now, the pathophysiology and exact role of these factors and how they contribute to UI have not been fully understood. To overcome this diagnostic issue, many serum biomarkers have been used as predictive markers for UI in females. Out of these biomarkers, leptin was found to be one of the most accurate biomarkers[10,11].
Leptin is an adipokinetic hormone that plays a key role in energy homeostasis and body weight regulation, and acts as a neuroendocrine mediator in different body systems, including the reproductive system[12-15]. Leptin is secreted mainly from adipocyte cells in the white adipose tissues, and altered with obesity[16]. Also, it can be produced from other cells related to the reproductive system in both males and females, such as placental syncytiotrophoblast cells, hypothalamus cells, and pituitary cells[12]. Evidence shows that leptin receptors can be found along the hypothalamic-pituitary-ovarian (HPO) axis of females. Therefore, leptin has direct regulatory effects, both inhibitory and stimulatory depending on its concentration, on all parts of the HPO axis, and all stages of the reproductive process starting from puberty, menstrual cycle, pregnancy, early embryo development, and lactations[13,17].
In the context of reproduction, several scholars have tried to find a relationship between adipose tissue hormones (adipokines) and the female reproductive system in general, and especially between leptin and ovarian functions. Findings have shown that high leptin concentration inhibited ovarian steroidogenesis, folliculogenesis, and oogenesis. The high level of leptin is associated with low levels of ovarian hormones, estradiol, and progesterone, and the poor quality of produced ova[18-20]. Therefore, it may be considered that the concentration of leptin is related to female infertility, and it could explain some cases of female UI. Meanwhile, studies on the association between leptin and UI reported conflicting results. Some studies showed that serum leptin levels were higher in women with UI compared with the fertile women[11,19-21], whereas other studies showed that there was no significant difference in leptin in women with UI compared to fertile women[22,23]. Thus, this study was aimed to find serum leptin levels in women with UI by conducting a systematic review and meta-analysis in order to quantitatively pool all findings from the relevant studies.
All studies that defined UI based on the World Health Organization standard definition and reported the plasma level of leptin in women with UI and fertile women were eligible for this study. Studies were not eligible for this study if: (1) They were reviews, letters, editorials, or studies using animals or cell lines; (2) No healthy control group was included; or (3) The study enrolled participants who had diseases other than UI, and/or were on any kind of medication.
The current study was performed according to PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)[24]. The information was retrieved from electronic and non-electronic database sources. Electronic sources included: PubMed/MEDLINE, Embase, Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov. Non-electronic sources included: Direct Google search, Google Scholar, OpenGrey, OATD, WorldCat.org, American Society for Reproductive Medicine and Canadian Fertility and Andrology Society (ASRM/CFAS) Conjoint Annual Meeting, Abstracts of the Scientific Oral and Poster Sessions, and European Society of Human Reproduction and Embryology (ESHRE) Annual Meeting, Abstracts of the Scientific Oral and Poster Sessions. All those databases were searched from their inception to April 30, 2021, for human studies published in English.
The terms AND, OR, and NOT were used as Boolean search terms to develop the research strategy, and the final search strategy included the use of Title/Abstract related to (Women with Unexplained Infertility) AND (Leptin) taken from the study questions. Non-electronic sources were used combined with direct Google search, Google Scholar, OpenGrey, OATD, and WorldCat.org, American Society for Reproductive Medicine and Canadian Fertility and Andrology Society (ASRM/CFAS) Conjoint Annual Meeting, Abstracts of the Scientific Oral and Poster Sessions, and ESHRE Annual Meeting, Abstracts of the Scientific Oral and Poster Sessions. In addition, a manual search by the investigators was done for the grey literature and unpublished thesis/papers.
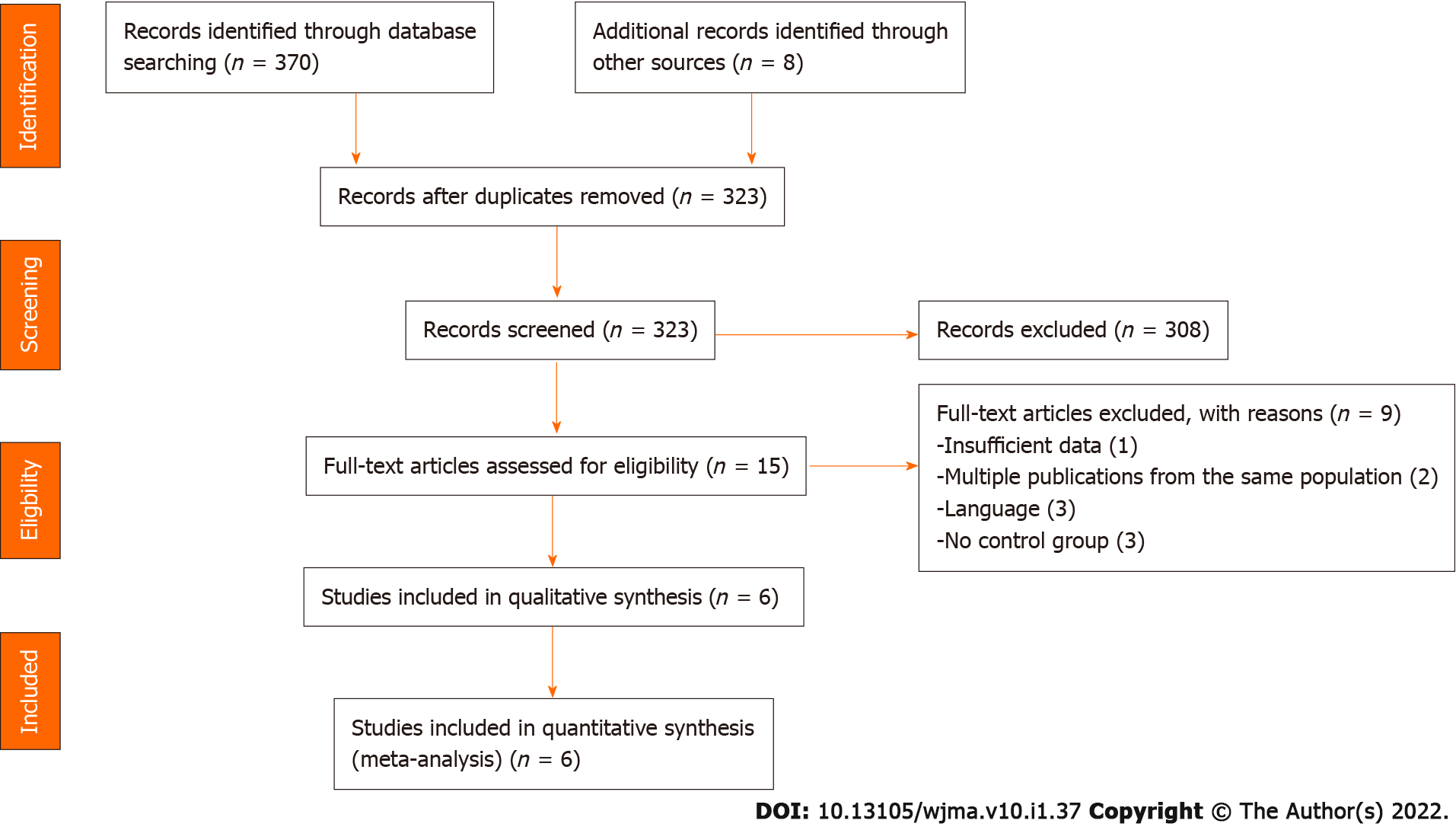
The selection of the studies was done following these steps: (1) All retrieved studies were exported to the EndNote X9 citation manager, to check for duplication, and then the duplicated articles were removed; (2) Three authors (AA, MA, and SO) screened and evaluated the remaining studies independently by carefully reading the title and abstract, and all studies that mentioned the outcomes of the review [(Women with Unexplained Infertility)/Leptin] in their titles and abstracts were considered for further evaluation based on the objectives, methods, participants, and the key findings, serum levels of leptin in women with UI; (3) Two authors (AA and MA) independently evaluated the quality of the relevant studies against the checklist; and (4) Any discrepancy was resolved by discussion between the two authors (AA and MA), or by asking a third reviewer if consensus could not be reached. The selection process of the studies is presented using PRISMA statement flow diagram (Figure 1).
After the selection of all appropriate articles for this study, the relevant data were extracted by two investigators independently (AA and MA) using a data extraction template and presented using Microsoft Word 2016. The investigators contacted the authors of any study who did not report the aforementioned data (via email) to obtain the original data and after the expiration of the 2-wk timeline, the studies with the missing data that could not be obtained were removed. The extraction template contained author name, year of publication, study design, method of serum leptin measurement, body mass index (BMI), age, sample size, leptin concentration, and the LH/FSH ratio (Table 1). The data extraction accuracy was verified by comparing the data extraction results from the two investigators (AA and MA), who independently extracted the data in a randomly selected subset of papers (30% of the total).
| Ref. | Region | Study design | Method | BMI (kg/m2) | Age, years | Sample size | Leptin (mean + SD), ng/mL | LH/FSH ratio | ||||
| UI | Controls | UI | Controls | UI | Controls | UI | Controls | |||||
| Tafvizi and Masomi[20], 2016 | Iran | Case–control | EIA | 23.6 ± 0.27 | 23.66 ± 0.33 | 29.3 ± 4.2 | 31.03 ± 3.76 | 40 | 30 | 31.20 ± 2.83 | 24.89 ± 2.94 | 0.85 |
| Al-Fartosy et al[21], 2019 | Iraq | RCT | EIA | 22.3 ± 3 | 21.7 ± 1.4 | 29.45 ± 6.38 | 30.92 ± 5.90 | 63 | 33 | 28.4 ± 1.3 | 27.2 ± 2.3 | 0.61 |
| Kamyabi and Gholamalizad[22], 2015 | Iran | Case-control | EIA | 24.84 | 22.26 | 30 | 29 | 30 | 30 | 27.83 ± 25.29 | 31.27 ± 11.02 | NR |
| Kumari et al[11]1, 2017 | Indian | Case-control | EIA | 24.1 ± 3.9 | 24.31 ± 3.19 | 29.53 ± 4.43 | 29.58 ± 4.01 | 120 | 109 | 68.9 ± 2.46 | 37.5 ± 1.84 | 0.85 |
| Baig et al[23], 2019 | Pakistan | Case-control | RIA | NR | NR | NR | NR | 235 | 205 | 35.32 ± 0.9 | 37.11 ± 1.19 | 2.16 |
| Demir et al[19], 2007 | Turkey | PCS | RIA | 25 | 24.5 | 29.3 | 28.9 | 27 | 30 | 7 ± 1 | 3.4 ± 1 | 1.17 |
The main outcome of this study was the serum leptin levels in women with UI, and it was measured by the direct report from the individual studies. To quantify the outcome “serum leptin levels in women with UI”, the investigators considered studies that reported serum leptin levels in their results. The result is expressed as the mean and standard deviation (SD).
The inclusion criteria were appraised for all retrieved articles by using their title and abstract first, and then, the full text was screened to check the quality of each study before the final selection. The following was the quality assessment criteria for the studies in the current review: (1) The diagnosis of female UI occurred after performing all available fertility tests; (2) The sample was representative for the cases and controls; (3) The controls enrolled were taken from the same population; (4) The controls had no any past history of UI; (5) The cases and controls were matched for age or BMI or the two of them together; and (6) The methods which were used to check the serum level of leptin were the same for cases and controls for each individual study.
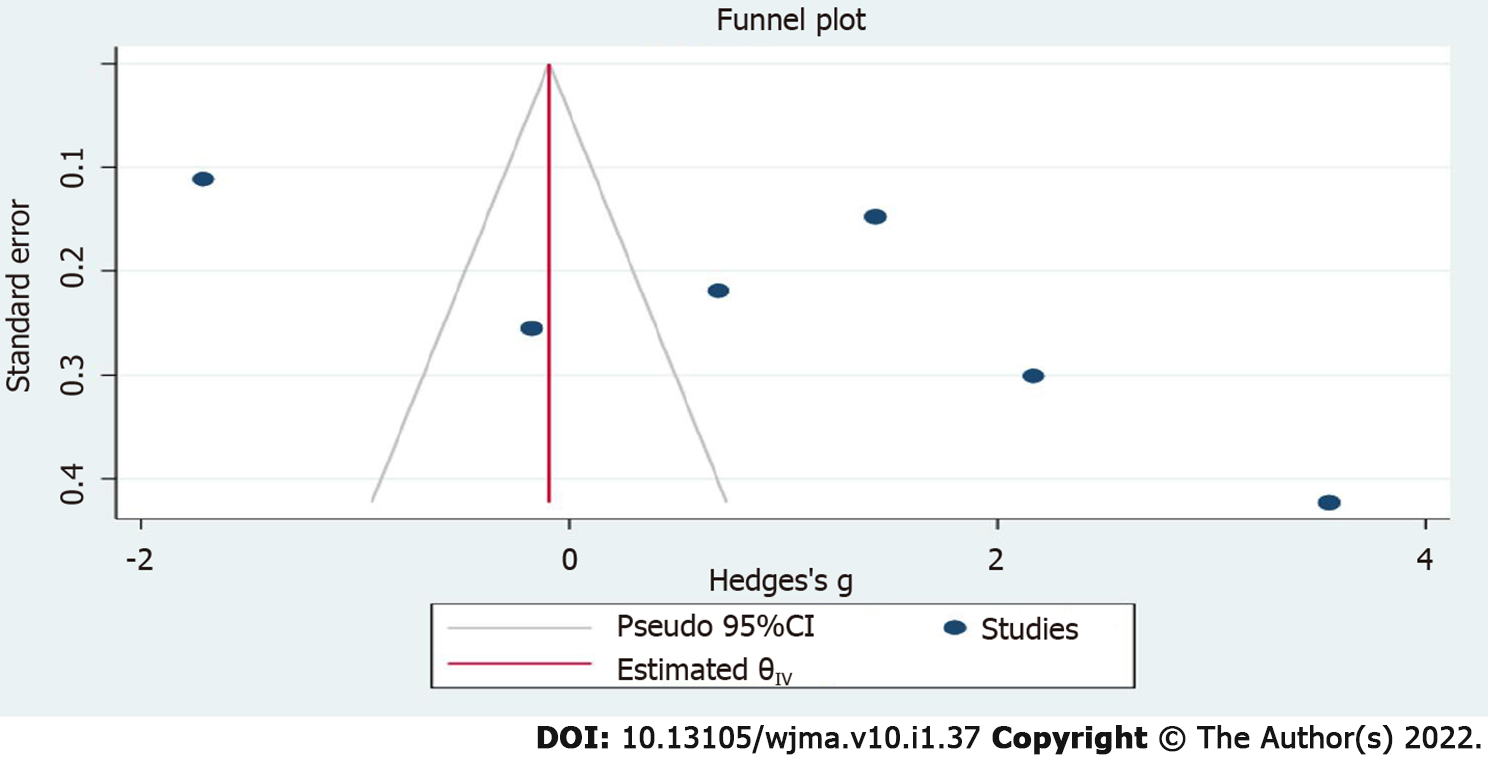
A comprehensive search (electronic/database search, manual search, grey literature search, and unpublished studies search) was done to minimize the risk of bias. The risk of bias from the included studies was individually appraised by three investigators (AA, MA, and SO) using a critical appraisal tool (Joanna Briggs Institute Quality Assessment Tool)[25]. The publication bias for the included studies was checked by visual inspection of the funnel plot and checking the statistical symmetry of the funnel plot using Egger’s regression test.
In light of the study objectives, the mean difference was used to synthesize and present the results for the analysis.
STATA software version 16 was used to synthesize and analyze the meta-analysis data. The recommendations of the I2 statistic described by Higgins et al[26] (I2 of 75/100% and above suggesting considerable heterogeneity) were used to perform this meta-analysis. The standardized mean difference (SMD) and 95% confidence interval (CI) were calculated for each study, based on the sample size, study mean, and SD of serum leptin levels in the case and control groups.
The potential publication bias was checked using a funnel plot and Egger’s regression test, and it was assumed to be significant if P values were less than 0.10. To identify the sources of heterogeneity, meta-regression was performed to evaluate the between-study heterogeneity and to assess the influence of different study features, such as sample size, test method, BMI, and LH/FSH ratio.
The studies were excluded from the final review if: (1) They had missing data; and (2) They had a high risk of bias. The study results were reported according to the PRISMA guidelines and the findings of the included studies are first presented using a narrative synthesis, followed by a meta-analysis chart.
As shown in Figure 1, a total of 378 articles were identified through the major electronic and non-electronic databases, and other relevant sources. A total of 55 studies were removed due to duplication, and the remaining 323 studies were kept for further critical screening. From the 323 studies which were kept in the first phase, 308 were excluded after they went through a very careful screening according to their titles and abstracts. From the remaining 15 articles, 9 studies were excluded due to inconsistency with the study inclusion criteria. Finally, 6 studies that fulfilled the eligibility criteria, involving 515 women with UI and 437 controls, were included for the systematic review and meta-analysis.
The circulating leptin levels in patients with UI vs controls were evaluated in all 6 studies. In 4 studies, serum leptin levels were measured by enzyme-linked immunosorbent assay and by radioimmunoassay in the remaining two studies. Two studies were done in Iran, and one in each in Pakistan, Iraq, India, and Turkey. All studies were matched using both BMI and age. However, one study did not report them, but it stated that “the study was matched using BMI and age”. In all included studies, the mean range was between 21.7 and 24.8 for BMI, and between 29 and 31 years for age. In addition, some missing information in the original studies was retrieved from the corresponding authors. Table 1 shows the detailed characteristics of all included studies.
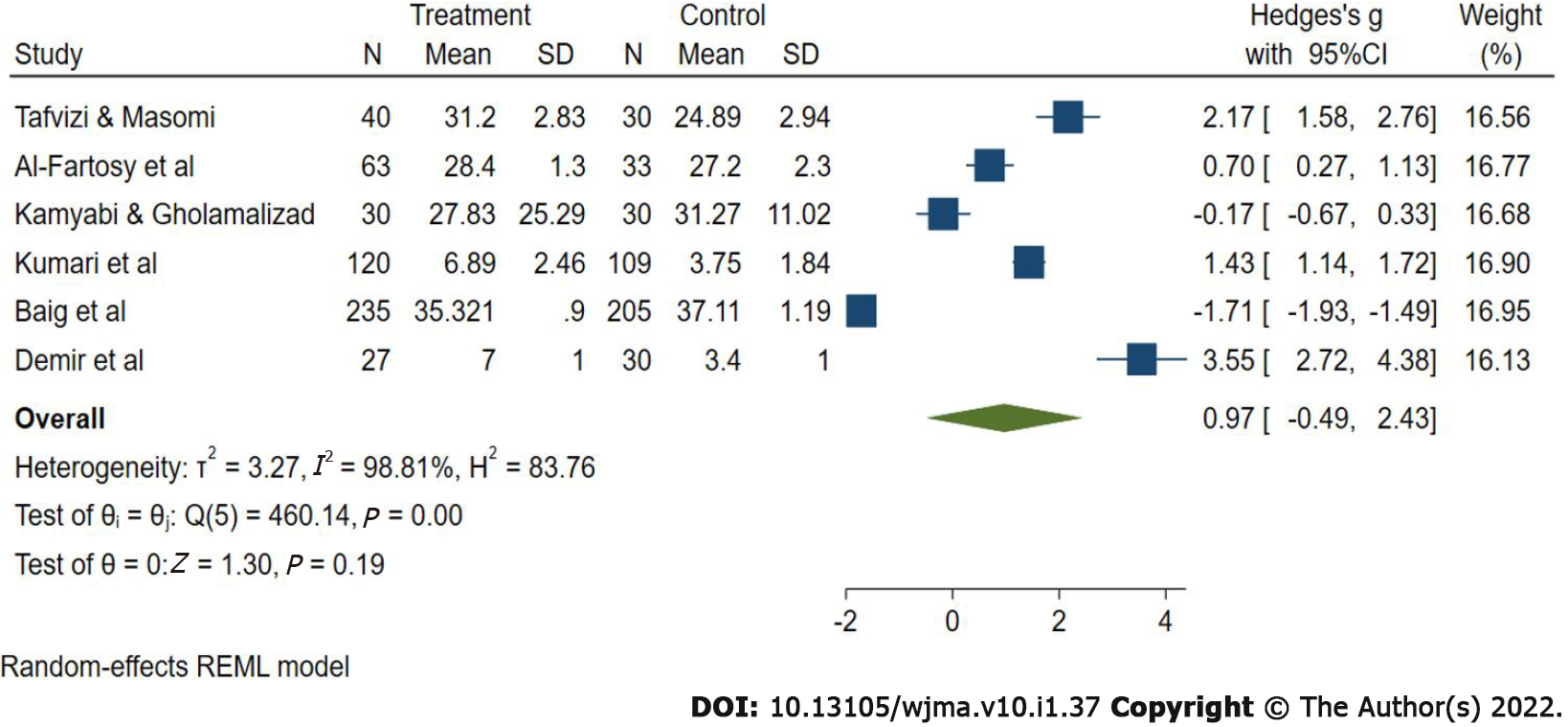
Figure 2 shows the result of this meta-analysis. The pooled estimate of the included studies showed that leptin levels were significantly higher in UI cases than in controls, with an SMD of 0.97 (95%CI: -0.49 to 2.43). The heterogeneity across studies was highly significant (P < 0.00001; I2 = 98.8%), hence the random effect model was employed for the analysis.
A sensitivity analysis was conducted by sequentially excluding studies from the meta-analysis to further investigate the possible sources of the heterogeneity among the studies, and the results suggested that the meta-analysis result was stable. In addition, multivariate meta-regression was performed to evaluate the influence of several factors that may modify the association between serum leptin levels and UI, including test method, BMI, sample size, and LH/FSH ratio (adjusted P = 0.177, 0.208, 0.997, and 0.15, respectively). However, the results showed that these confounding factors did not substantially affect the heterogeneity. For the test of publication bias, the funnel plots (Figure 3) were visually symmetric and the Egger's test for publication bias yielded a P value of 0.279, hence these results did not provide evidence of a significant effect.
The term UI emerged due to the fact that the current knowledge on assessment and treatment of the reproductive system is still inadequate[3]. Many studies have been carried out to find the exact cause of UI and the best diagnostic biomarker. However, leptin has been found as one of the best biomarkers. Leptin displays biological activities by binding and activating specific leptin receptors, which are found in many organs including the hypothalamus-pituitary-ovarian axis (HPO axis) in females. Leptin plays a role in the function of the HPO axis by stimulating the release of gonadotrophin-releasing hormone, gonadotrophins, and aromatase enzymes from the hypothalamus, pituitary gland, and ovaries, respectively[13,15,17,27,28]. Also, the available evidence indicated that a high level of leptin has negative effects on female reproduction due to its inhibitory effect on the HPO axis, ovarian physiology, folliculogenesis, steroidogenesis, and the production and release of oxytocin and prostaglandin[29-32]. In line with available evidence, the current study showed that leptin level was significantly higher in women with UI compared with the control group. Similar results were found when leptin concentrations were pooled in endometriosis and polycystic ovary syndrome (PCOS) cases, pathological conditions with a strong correlation with infertility. In these studies, leptin levels were higher in women with endometriosis and PCOS groups compared with control groups[33,34].
Studies have suggested that factors like age and BMI have effects on leptin levels, and usually have a positive correlation with female infertility[35,36]. However, in the present study, all the included studies were matched by both age and BMI, and because of that, the effect of age and BMI on leptin level was not examined.
This is the first comprehensive quantitative meta-analysis summarizing available evidence to determine the serum leptin level in women with UI.
The results of this meta-analysis suggest the presence of elevated levels of leptin levels in women with UI compared with fertile women. Hence, leptin could be a potential biomarker for UI in women, and it may be useful for identifying women at a high risk of infertility. However, further investigations need to be carried out in order to clarify the exact association between leptin levels and UI.
Despite many breakthroughs in the field of infertility diagnosis and treatment, there are still some infertility cases with unknown causes (unexplained infertility). To overcome this diagnostic issue, many serum biomarkers have been used as predictive markers for unexplained infertility in females.
Leptin is one of the most accurate biomarkers for unexplained infertility. Nevertheless, conflicting results regarding leptin levels in women with unexplained infertility have been reported.
The objective of this study was to conduct a systematic review and meta-analysis to find the serum leptin levels in women with unexplained infertility.
A systematic literature search was conducted before April 30, 2021 from PubMed/MEDLINE, Embase, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov, Google Scholar, OpenGrey, OATD, and the infertility conferences abstract.
A total of six articles were included in this meta-analysis after 15 articles had been subjected to full-text evaluations.
Leptin could be a potential biomarker for unexplained infertility in women.
The effect of other adipokines should be evaluated in future studies to find their possible relation with female infertility.
Provenance and peer review: Unsolicited article; externally peer reviewed.
Peer-review model: Single blind
Specialty type: Reproductive Biology
Country/Territory of origin: Nigeria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chava V, Liu Z S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Patrizi G, Manna C, Moscatelli C, Nieddu L. Pattern recognition methods in human‐assisted reproduction. Int Trans Oper Res. 2004;11:365-379. [DOI] [Full Text] |
| 2. | Abebe MS, Afework M, Abaynew Y. Primary and secondary infertility in Africa: systematic review with meta-analysis. Fertil Res Pract. 2020;6:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (1)] |
| 3. | Mol BW, Tjon-Kon-Fat R, Kamphuis E, van Wely M. Unexplained infertility: Is it over-diagnosed and over-treated? Best Pract Res Clin Obstet Gynaecol. 2018;53:20-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 4. | Abdallah KS, Hunt S, Abdullah SA, Mol BWJ, Youssef MA. How and Why to Define Unexplained Infertility? Semin Reprod Med. 2020;38:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | World health Organization. Infertility 2021 [April 29, 2021]. Available from: https://www.who.int/reproductivehealth/topics/infertility/keyissues/en/. |
| 6. | Abdullah AA, Ahmed M, Oladokun A. Prevalence of infertility in Sudan: A systematic review and meta-analysis. Qatar Med J. 2021;2021:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (3)] |
| 7. | Abdelazim IA, Purohit P, Farag RH, Zhurabekova G. Unexplained infertility: prevalence, possible causes and treatment options. A review of the literature. J Obstet Gynecol Investig. 2018;1 1:e17-e22. [DOI] [Full Text] |
| 8. | Christensen A, Bentley GE, Cabrera R, Ortega HH, Perfito N, Wu TJ, Micevych P. Hormonal regulation of female reproduction. Horm Metab Res. 2012;44:587-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Ehsani M, Mohammadnia-Afrouzi M, Mirzakhani M, Esmaeilzadeh S, Shahbazi M. Female Unexplained Infertility: A Disease with Imbalanced Adaptive Immunity. J Hum Reprod Sci. 2019;12:274-282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Qu T, Yan M, Shen WJ, Li L, Zhu P, Li Z, Huang J, Han T, Hu W, Zhou R, Li P, Xu L, Huang T, Zhong Y, Gu J. Predictive serum markers for unexplained infertility in child-bearing aged women. Am J Reprod Immunol. 2020;83:e13194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Kumari P, Jaiswar SP, Shankhwar P, Deo S, Ahmad K, Iqbal B, Mahdi AA. Leptin as a Predictive Marker in Unexplained Infertility in North Indian Population. J Clin Diagn Res. 2017;11:QC28-QC31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Herrid M, Palanisamy SK, Ciller UA, Fan R, Moens P, Smart NA, McFarlane JR. An updated view of leptin on implantation and pregnancy: a review. Physiol Res. 2014;63:543-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Mantzoros CS, Magkos F, Brinkoetter M, Sienkiewicz E, Dardeno TA, Kim SY, Hamnvik OP, Koniaris A. Leptin in human physiology and pathophysiology. Am J Physiol Endocrinol Metab. 2011;301:E567-E584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 407] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 14. | Blüher S, Mantzoros CS. Leptin in reproduction. Curr Opin Endocrinol Diabetes Obes. 2007;14:458-464. |
| 15. | Pérez-Pérez A, Sánchez-Jiménez F, Maymó J, Dueñas JL, Varone C, Sánchez-Margalet V. Role of leptin in female reproduction. Clin Chem Lab Med. 2015;53:15-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 88] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 16. | Mitchell M, Armstrong DT, Robker RL, Norman RJ. Adipokines: implications for female fertility and obesity. Reproduction. 2005;130:583-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 179] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 17. | Khan SM, Hamnvik OP, Brinkoetter M, Mantzoros CS. Leptin as a modulator of neuroendocrine function in humans. Yonsei Med J. 2012;53:671-679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Fornari MC, Sarto A, Berardi VE, Martínez MA, Rocha MG, Pasqualini S, Diez RA. Effect of ovaric hyper-stimulation on blood lymphocyte subpopulations, cytokines, leptin and nitrite among patients with unexplained infertility. Am J Reprod Immunol. 2002;48:394-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Demir B, Guven S, Guven ES, Atamer Y, Gunalp GS, Gul T. Serum leptin level in women with unexplained infertility. J Reprod Immunol. 2007;75:145-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Tafvizi F, Masomi M. Comparison of Serum Leptin Level in Women with Unexplained Infertility and Fertile Women in Iran. J Obstet Gynaecol India. 2016;66:466-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Al-Fartosy AJM, Awad NA, Mahmood RA. A comparative study of leptin, oxidant/antioxidant status and some trace elements in women of healthy control and unexplained infertility in Basrah-Iraq. Indones Biomed J. 2019;11:327-337. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Kamyabi Z, Gholamalizade T. A Comparative Study of Serum and Follicular Fluid Leptin Concentrations among Explained Infertile, Unexplained Infertile and Fertile Women. Int J Fertil Steril. 2015;9:150-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 23. | Baig M, Azhar A, Rehman R, Syed H, Tariq S, Gazzaz ZJ. Relationship of Serum Leptin and Reproductive Hormones in Unexplained Infertile and Fertile Females. Cureus. 2019;11:e6524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 40520] [Article Influence: 10130.0] [Reference Citation Analysis (2)] |
| 25. | Jordan Z, Lockwood C, Munn Z, Aromataris E. The updated Joanna Briggs Institute Model of Evidence-Based Healthcare. Int J Evid Based Healthc. 2019;17:58-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 214] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 26. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46535] [Article Influence: 2115.2] [Reference Citation Analysis (3)] |
| 27. | Catalano S, Marsico S, Giordano C, Mauro L, Rizza P, Panno ML, Andò S. Leptin enhances, via AP-1, expression of aromatase in the MCF-7 cell line. J Biol Chem. 2003;278:28668-28676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 209] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 28. | Panwar S, Herrid M, Kauter KG, McFarlane JR. Effect of passive immunization against leptin on ovarian follicular development in prepubertal mice. J Reprod Immunol. 2012;96:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Masarwi M, Shamir R, Phillip M, Gat-Yablonski G. Leptin stimulates aromatase in the growth plate: limiting catch-up growth efficiency. J Endocrinol. 2018;237:229-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Ashrafi Mahabadi S, Tafvizi F. Reduction of Soluble Leptin Receptor Levels in Women with Unexplained Infertility and the Effect of Leptin Receptor Gln223Arg Polymorphism on its Serum Level. J Obstet Gynecol Cancer Res. 2020;5:149-158. [DOI] [Full Text] |
| 31. | Vilariño-García T, Pérez-Pérez A, Santamaría-López E, Prados N, Fernández-Sánchez M, Sánchez-Margalet V. Sam68 mediates leptin signaling and action in human granulosa cells: possible role in leptin resistance in PCOS. Endocr Connect. 2020;9:479-488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Landry DA, Sormany F, Haché J, Roumaud P, Martin LJ. Steroidogenic genes expressions are repressed by high levels of leptin and the JAK/STAT signaling pathway in MA-10 Leydig cells. Mol Cell Biochem. 2017;433:79-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 33. | Kalaitzopoulos DR, Lempesis IG, Samartzis N, Kolovos G, Dedes I, Daniilidis A, Nirgianakis K, Leeners B, Goulis DG, Samartzis EP. Leptin concentrations in endometriosis: A systematic review and meta-analysis. J Reprod Immunol. 2021;146:103338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 34. | Zheng SH, Du DF, Li XL. Leptin Levels in Women With Polycystic Ovary Syndrome: A Systematic Review and a Meta-Analysis. Reprod Sci. 2017;24:656-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 35. | Daghestani MH, Daghestani M, Daghistani M, El-Mazny A, Bjørklund G, Chirumbolo S, Al Saggaf SH, Warsy A. A study of ghrelin and leptin levels and their relationship to metabolic profiles in obese and lean Saudi women with polycystic ovary syndrome (PCOS). Lipids Health Dis. 2018;17:195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 36. | Van Zyl S, Van der Merwe LJ, Van Rooyen FC, Joubert G, Walsh CM. The relationship between obesity, leptin, adiponectin and the components of metabolic syndrome in urban African women, Free State, South Africa. South Afr J Clin Nutr. 2017;30:8-13. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |