Copyright
©The Author(s) 2017.
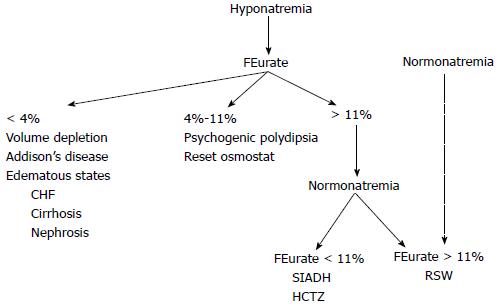
Figure 1 Proposed algorithm based on determinations of FEurate to evaluate hyponatremic patients without the need to assess the volume status of the patient or determinations of UNa, plasma renin or aldosterone levels.
The dotted line connecting normonatremia and RSW with FEurate > 11% needs further verification. Modified from Ref. [28]. SIADH: Syndrome of inappropriate anti-diuretic hormone; RSW: Renal salt wasting; HCTZ: Hydrochlorothiazide; CHF: Congestive heart failure.
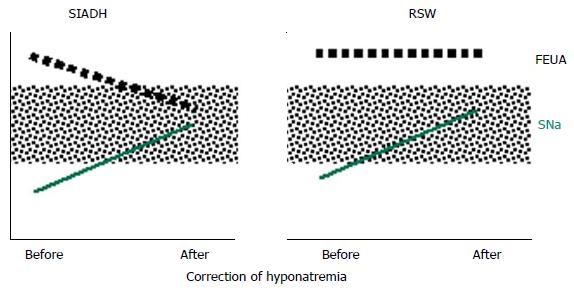
Figure 2 Figure depicting the relationship between serum sodium and FEurate in syndrome of inappropriate anti-diuretic hormone and renal salt wasting.
Dotted areas denote normal values. Note FEurate to be increased when patients with SIADH and RSW are hyponatremic but normalize in SIADH and remain increased in RSW. Modified from Ref. [28]. SIADH: Syndrome of inappropriate anti-diuretic hormone; RSW: Renal salt wasting; FEUA: Feurate; SNa: Serum sodium.
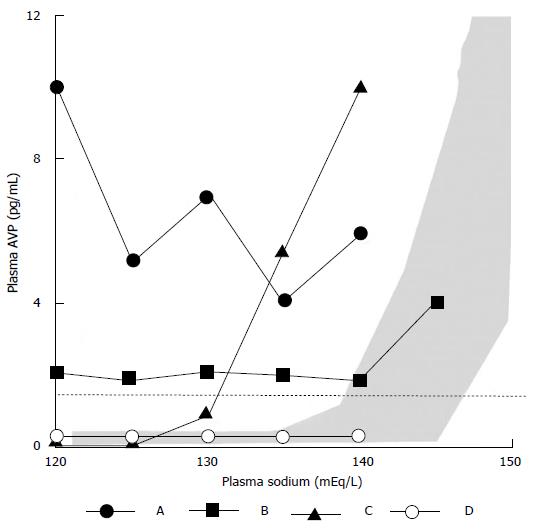
Figure 3 Types of the syndrome of inappropriate anti-diuretic hormone.
Printed with permission, Ref. [66]. AVP: Arginine vasopressin.
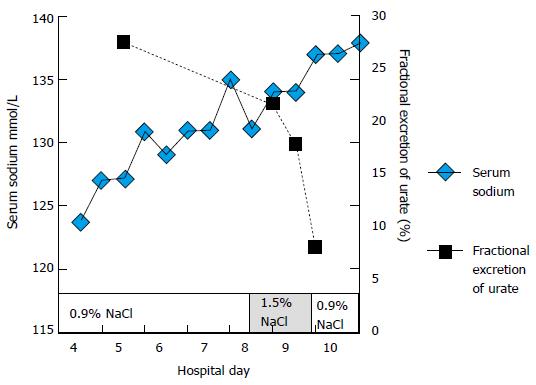
Figure 4 Illustrating how FEurate progressively decreases from an increased rate of 26.
2% to a normal of 8% as serum sodium increases to a normal of 138 mEq/L in syndrome of inappropriate anti-diuretic hormone. Normalization of serum sodium did not occur after receiving large volumes of isotonic saline and was possible by using 1.5% hypertonic saline after receiving volumes of isotonic saline. The increase in serum sodium from 131 to 135 mEq/L occurred when he was on very large salt supplementation. This figure also confirms saline does not increase FEurate. Printed with permission, Ref. [31].
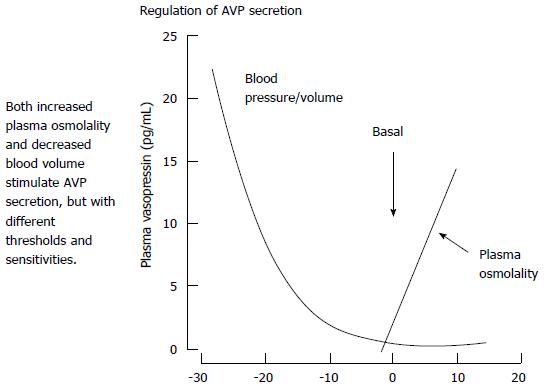
Figure 5 Effect of changes in extracellular volume, pressure and osmolality on plasma vasopressin levels.
Note the marked increase in vasopressin levels with volume depletion which is more potent that the osmolar stimulus so a volume depleted will maintain high vasopressin levels despite the coexisting hypo osmolality of plasma. Printed with permission, Stricker et al[37]. AVP: Arginine vasopressin.
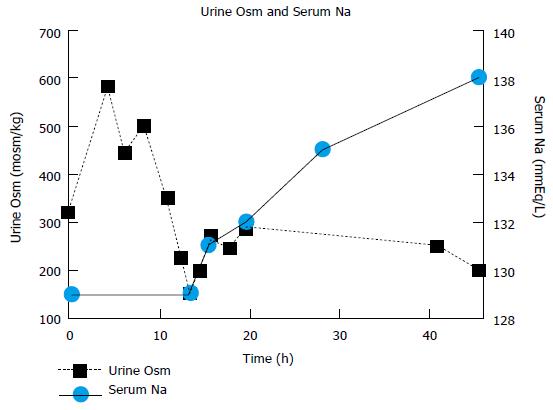
Figure 6 Changes in urine osmolality and serum sodium concentration during isotonic infusion in a hyponatremic patient with a hip fracture without clinical evidence of cerebral disease.
The low Uosm at baseline reflected a low sodium intake when UNa was only 6 mEq/L and a weakened medullary solute concentration, which increased rapidly with a marked increase in Uosm after 4 h of saline infusion. Plasma antidiuretic hormone (ADH) was increased with increased plasma renin and aldosterone levels at baseline and ADH level was undetectable when the urine was dilute 13 h with increase in serum sodium to 138 mEq/L within 48 h after initiation of isotonic saline infusion. Printed with permission, Ref. [12].
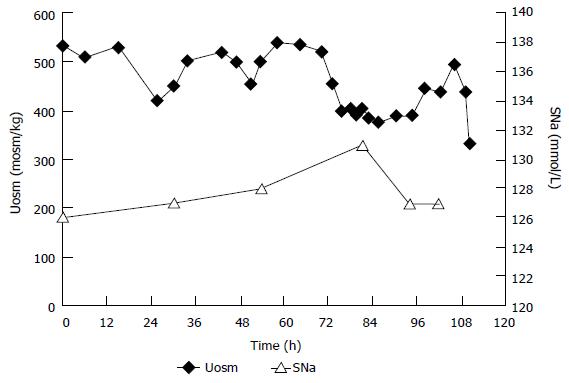
Figure 7 Effect of isotonic infusion in patient with syndrome of inappropriate anti-diuretic hormone in whom blood volume determination by 51chromium-labeled red blood cells and radio iodinated serum albumin was increased.
Note persistently increased urine osmolality or failure of urine to become dilute or correction of hyponatremia which are common features of SIAD response to isotonic saline infusion. Printed with permission, Ref. [13]. SIADH: Syndrome of inappropriate anti-diuretic hormone; SNa: Serum sodium; Uosm: Urine osmolality.
- Citation: Maesaka JK, Imbriano LJ, Miyawaki N. Application of established pathophysiologic processes brings greater clarity to diagnosis and treatment of hyponatremia. World J Nephrol 2017; 6(2): 59-71
- URL: https://www.wjgnet.com/2220-6124/full/v6/i2/59.htm
- DOI: https://dx.doi.org/10.5527/wjn.v6.i2.59