Copyright
©The Author(s) 2021.
World J Clin Infect Dis. Jan 15, 2021; 11(1): 19-26
Published online Jan 15, 2021. doi: 10.5495/wjcid.v11.i1.19
Published online Jan 15, 2021. doi: 10.5495/wjcid.v11.i1.19
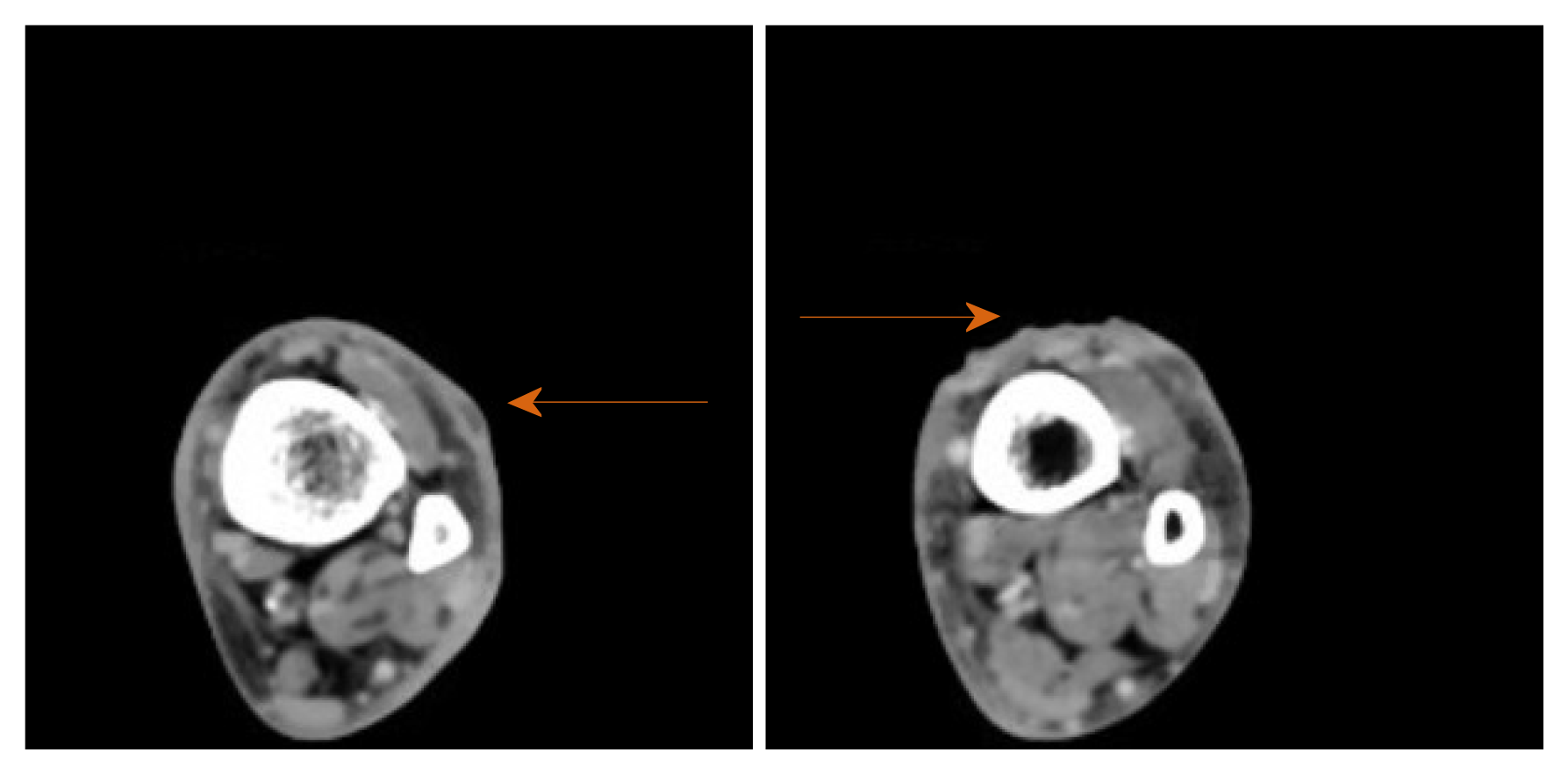
Figure 1 Physical examination.
A: Skin ulcer with tracking nodules on admission; B and C: Skin ulcer after antibiotics for cellulitis.
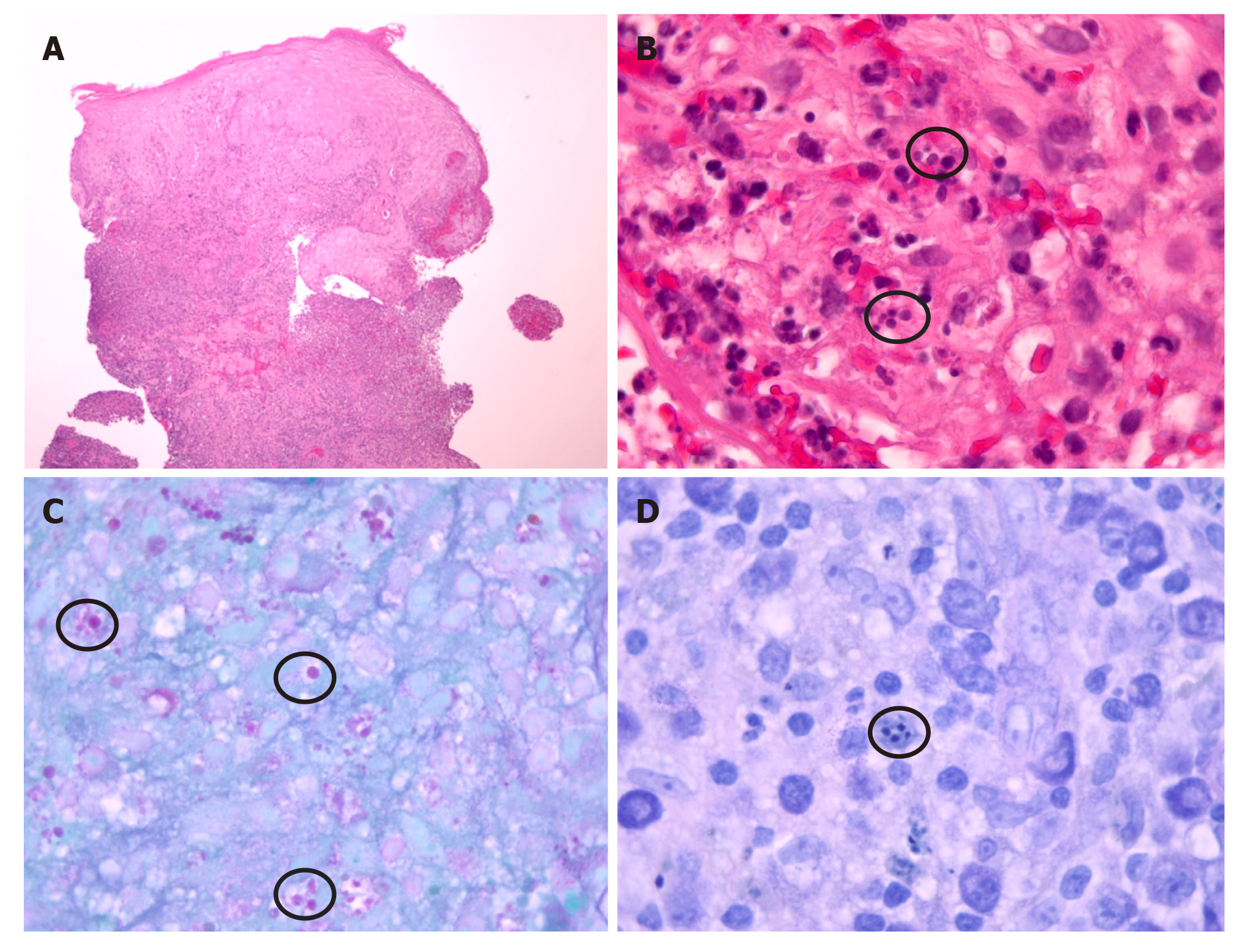
Figure 2 Computer tomography scan of left lower extremity, cross sectional view showing phlegmon and ulcerated skin (orange arrows).
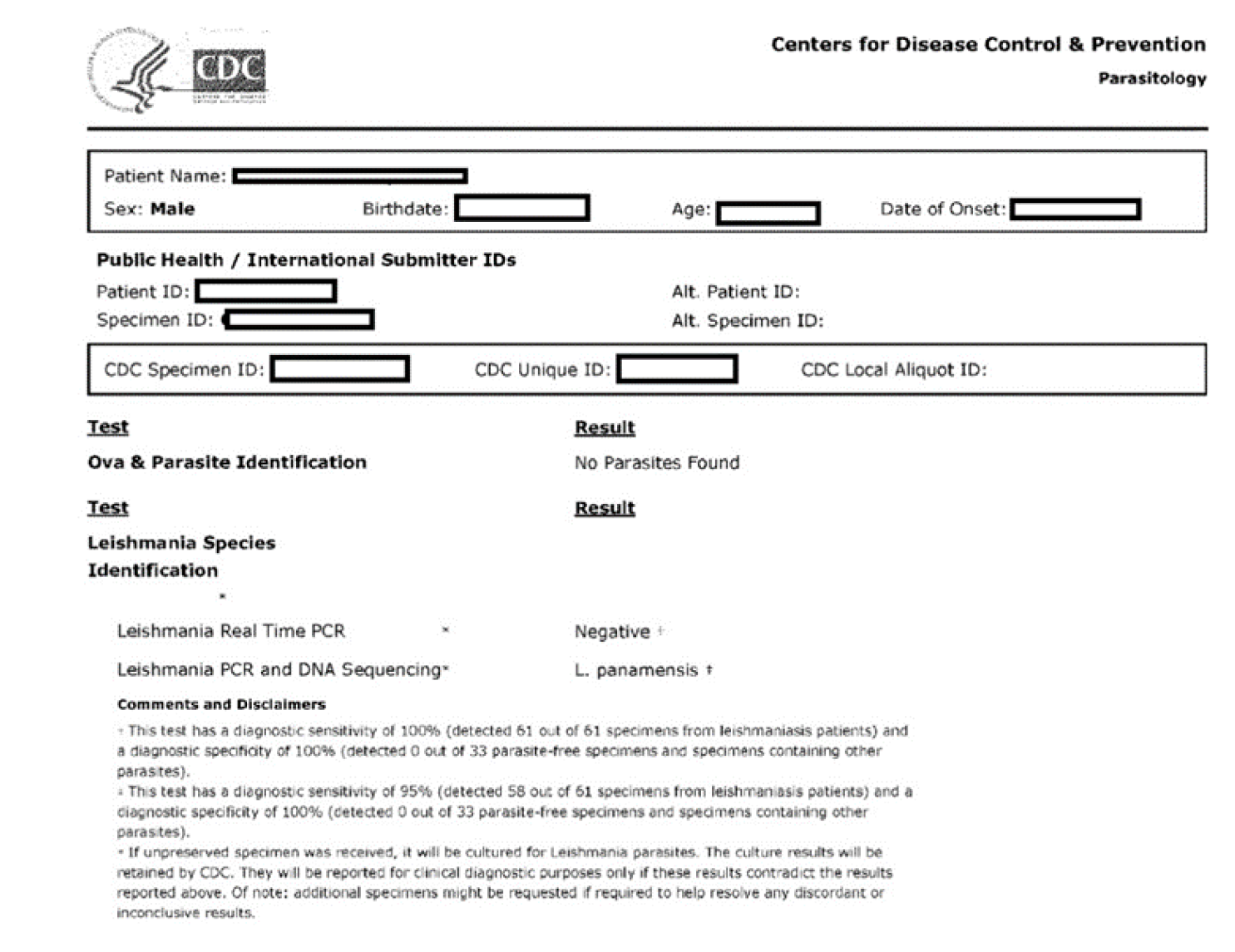
Figure 3 Histopathology was compatible with leishmaniasis amastigotes.
A: Reactive squamous epithelium with mixed superficial and deep inflammatory infiltrate (hematoxylin-eosin staining, original magnification × 40); B: Organisms compatible with Leishmania amastigotes (hematoxylin-eosin staining, original magnification × 1000). Location within histiocytes is obscured by marked acute inflammatory infiltrate; C: Parasitized histiocytes with staining of Leishmania amastigotes (PAS, original magnification × 1000); and D: Parasitized histiocytes with staining of Leishmania amastigotes (Giemsa, original magnification × 1000).
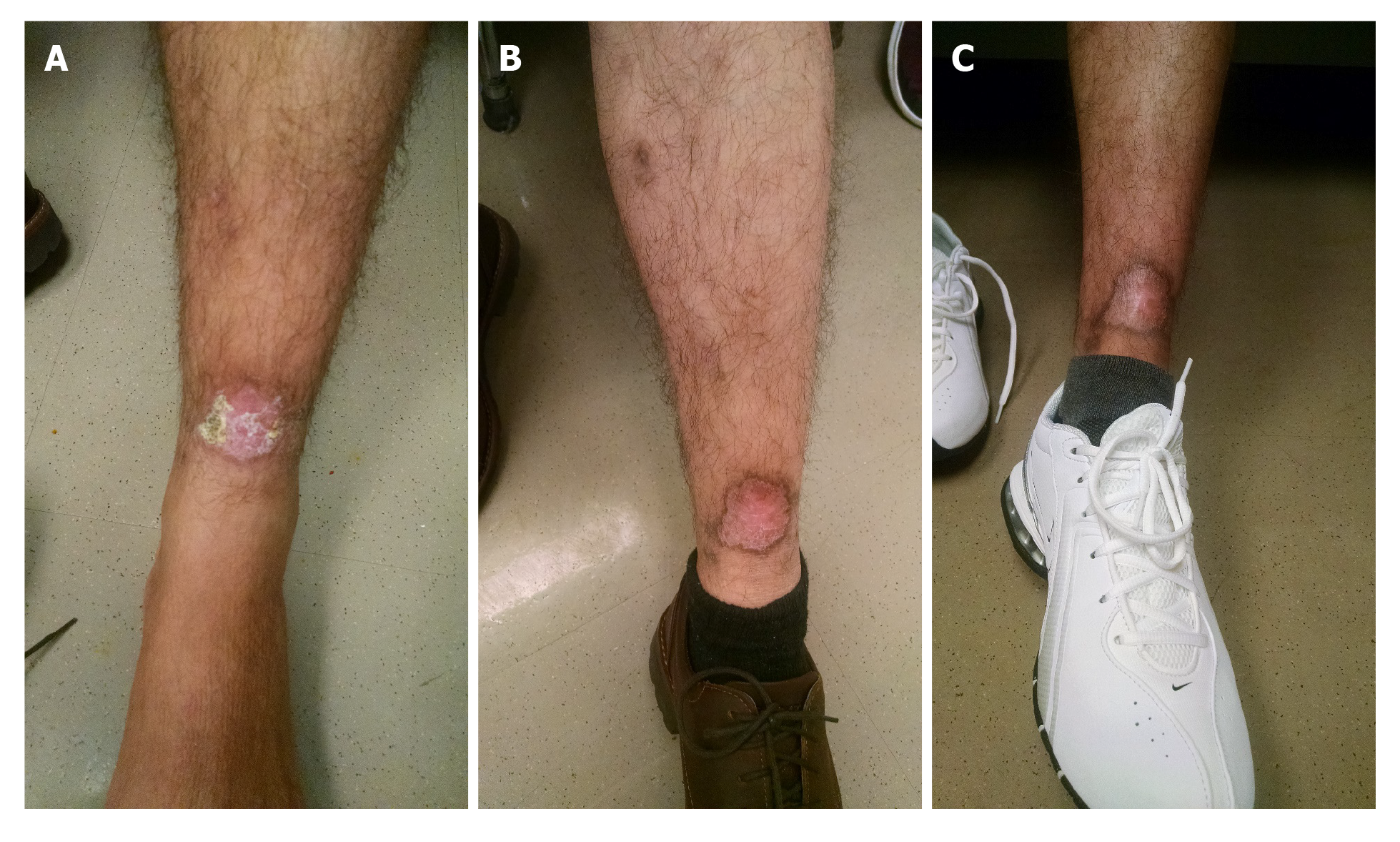
Figure 4 Report from centers for disease control and prevention.
Figure 5 Patient followed up with dermatology and infectious diseases clinic at several occasions, and then visited at approximately 11 mo with a healed ulcer.
A: Skin ulcer after 13 d of 28 d treatment with miltefosine; B: After 5 mo of treatment; and C: After 11 mo of treatment.
- Citation: Azhar A, Connell HE, Haas C, Surla J, Reed D, Kamboj S, Love GL, Bennani Y. Cutaneous leishmaniasis in Louisiana - one-year follow-up: A case report. World J Clin Infect Dis 2021; 11(1): 19-26
- URL: https://www.wjgnet.com/2220-3176/full/v11/i1/19.htm
- DOI: https://dx.doi.org/10.5495/wjcid.v11.i1.19