Published online Jun 20, 2025. doi: 10.5493/wjem.v15.i2.101388
Revised: November 28, 2024
Accepted: December 23, 2024
Published online: June 20, 2025
Processing time: 214 Days and 22.9 Hours
Fever of unknown origin (FUO) remains a diagnostic challenge and was originally defined in 1961. Its classic criteria include fever ≥ 38.3 °C (≥ 101 °F) on multiple occasions, fever lasting three weeks or longer, and a diagnosis after one week of inpatient evaluation. However, these criteria may not fully encompass the varied clinical presentations seen in resource-limited settings such as India. The adap
To investigate the applicability of revised FUO criteria in a tertiary care setting in India.
This longitudinal-exploratory study at All India Institute of Medical Sciences Rishikesh (January 2018–December 2022) analyzed 228 adult patients with fever ≥ 99.1 °F lasting over three days. Patients diagnosed within three days of admission were excluded. Data were collected retrospectively and prospectively using predefined FUO definitions based on durations of nondiagnosis (3-21 days, > 21 days), temperature ranges (99.1 °F-100.9 °F, ≥ 101 °F), and hospitalization durations (3-7 days, > 7 days). Descriptive statistics and comparative tests (Fisher's exact test, χ2 test) evaluated outcomes across definitions.
Among the proposed FUO definitions, Definition B (fever lasting 3-21 days, temperatures between 99.1 °F-100.9 °F, hospitalization > 7 days) predominated (40.8%), while only 2.2% met the classical criteria. Notably, 36.5% of Definition B patients remained undiagnosed after 7-10 days, despite 94% undergoing diagnostic workups within 21 days. Infection emerged as the leading etiology across definitions, without significant variation in outcomes or mortality during hospitalization (χ2 = 27.937, P = 0.142).
Adapting FUO criteria to local contexts improves diagnostic accuracy and treatment. Definition B (40.8% prevalence) showed practical utility, with higher mortality in patients discharged on empirical 'Anti-tuberculosis therapy'.
Core Tip: This study evaluates the feasibility of revising fever of unknown origin (FUO) diagnostic criteria in a tertiary care setting in North India. It proposes a new definition (Definition B), which includes fever lasting 3-21 days, temperatures between 99.1 °F-100.9 °F, and hospitalization for over 7 days. The findings highlight the predominance of infections as the leading etiology, the low applicability of classical FUO criteria, and the importance of adapting diagnostic frameworks to local epidemiology. This approach aims to enhance early diagnosis, optimize resource use, and improve patient outcomes in resource-limited settings.
- Citation: Dhangar P, Panda PK, Kant R, Gupta R, Dua R, Tiwari A, Saini S, Khoiwal K, Bahurupi Y. Evaluating fever of unknown origin definitions in a tertiary care setting: Implications for diagnostic criteria revision. World J Exp Med 2025; 15(2): 101388
- URL: https://www.wjgnet.com/2220-315x/full/v15/i2/101388.htm
- DOI: https://dx.doi.org/10.5493/wjem.v15.i2.101388
Fever of unknown origin (FUO), or pyrexia of unknown origin presents a diagnostic challenge characterized by pro
The definition and management of FUO have evolved significantly since its inception, reflecting advancements in diagnostic techniques, epidemiological shifts, and global healthcare disparities. Early studies predominantly from Western populations emphasized infectious diseases, malignancies, and connective tissue disorders as leading causes of FUO[2]. However, studies from non-Western regions, including Asia and Africa, highlight unique challenges such as endemic infections, tropical diseases, and socioeconomic factors influencing healthcare access and outcomes[3-5].
Recent research suggests that modifying FUO criteria to consider regional epidemiology and resource constraints can enhance diagnostic accuracy and timely intervention[6]. For instance, lowering the temperature threshold for defining fever and adjusting the duration of diagnostic workup may better suit the clinical realities in resource-limited settings, ensuring earlier initiation of empirical treatment and improving patient outcomes[7].
In resource-limited regions such as North India, where infectious diseases, tuberculosis, and endemic tropical illnesses prevail, adapting FUO criteria becomes imperative to enhance diagnostic yield and therapeutic outcomes. The conventional criteria may not fully capture the varied etiologies and clinical presentations encountered in these settings. This paper aims to explore the experience of the “All India Institute of Medical Sciences (AIIMS)”, Rishikesh, a tertiary care center in North India, in managing and defining FUO cases by proposing revisions to existing criteria to better reflect local epidemiological realities and optimize patient care.
This longitudinal-exploratory study was conducted at AIIMS Rishikesh, Uttarakhand, over a five-year period from January 2018 to December 2022. Universal sampling was employed to ensure representation across diverse demographic and clinical profiles. This study employed a retrospective and prospective design to analyze the prevalence, etiology, and outcomes of FUO among adult patients admitted to various departments, including general medicine, gastroenterology, neurology, pulmonology, nephrology, and obstetrics and gynecology.
The study included 228 adult patients who met the inclusion criteria of a documented fever ≥ 99.1 °F on at least two occasions and a fever duration exceeding three days upon admission. Patients with a definitive diagnosis within three days of hospitalization were excluded.
To address the limitations of traditional FUO criteria, this study proposed revised definitions based on the duration of undiagnosed fever (3-21 days, > 21 days), temperature range (99.1 °F-100.9 °F, ≥ 101 °F), and duration of hospitalization (3-7 days, > 7 days). Definitions were designed to capture a broad spectrum of FUO presentations while allowing flexibility in clinical management and diagnostic timelines (Table 1).
| Definition | Days of undiagnosis | Temperature | Days of hospitalization |
| A | 3-21 | 99.1 °F-100.9 °F | 3-7 |
| B | 3-21 | 99.1 °F-100.9 °F | > 7 |
| C | 3-21 | >/= 101 °F | 3-7 |
| D | 3-21 | >/= 101 °F | > 7 |
| E | > 21 | 99.1 °F-100.9 °F | 3-7 |
| F | > 21 | 99.1 °F-100.9 °F | > 7 |
| G | > 21 | >/= 101 °F | 3-7 |
| H | > 21 | >/= 101 °F | > 7 |
Retrospective data were retrieved from hospital records. Prospective data collection involved the follow-up of eligible patients to assess outcomes at discharge and 180 days postadmission through telephone confirmation. Details regarding mortality, the undiagnosis rate, the use of empirical treatment, and the outcomes of the patients discharged on empirical treatment were obtained at follow-up.
A structured data collection protocol was implemented to systematically capture demographic details, clinical parameters, diagnostic investigations, and outcomes. This comprehensive dataset facilitated a detailed analysis of FUO cases, enabling the delineation of distinct categories based on undiagnosed duration, temperature range, and days of hospitalization. The data included demographic details, clinical parameters, diagnostic investigations, and FUO categorization.
Descriptive statistics were used to summarize the demographic and clinical characteristics of the study population. Categorical variables are presented as frequencies and percentages, while continuous variables are reported as the mean ± SD or median (interquartile range) as appropriate. For comparative analyses, Fisher's exact test was used for categorical variables, and χ2 tests were used for outcomes, with P < 0.05 indicating statistical significance. Data management and statistical analyses were performed using IBM SPSS Statistics version 26.0.
The mean age of the patients was approximately 44 years, and 59% were males. The mean duration of hospitalization was 12.88 ± 8.44 days, while the mean duration of fever was 55.93 ± 115.26 days. The study identified Definition B (fever lasting 3-21 days, temperature 99.1 °F-100.9 °F, > 7 days of hospitalization) as the most prevalent FUO definition (40.8%), followed by definitions A, D, and C (Table 2). Surprisingly, only a minority (2.2%) of patients met the classical FUO criteria (Definition H), underscoring the inadequacy of traditional criteria in capturing FUO cases in the study setting.
| Definition | Frequency | Percentage (%) | 95%CI (%) |
| A | 49 | 21.5 | 16.5-27.5 |
| B | 93 | 40.8 | 34.4-47.5 |
| C | 28 | 12.3 | 8.5-17.4 |
| D | 44 | 19.3 | 14.5-25.1 |
| E | 1 | 0.4 | 0.0-2.8 |
| F | 7 | 3.1 | 1.4-6.5 |
| G | 1 | 0.4 | 0.0-2.8 |
| H | 5 | 2.2 | 0.8-5.3 |
Among patients classified under definition B, 36.5% remained undiagnosed beyond 7-10 days despite initiating treatment within 21 days of hospitalization. The majority (94%) of patients underwent comprehensive diagnostic evaluations within the initial 21 days, highlighting the critical window for early intervention in FUO management.
Etiologically, infections emerged as the predominant cause of FUO across all proposed definitions, followed by autoimmune disorders and malignancies. There was no significant variation in the distribution of underlying etiologies among the different FUO definitions, suggesting that the proposed definitions captured similar patterns of disease presentation and etiological diversity.
Analysis of outcomes at discharge and at the 180-day follow-up revealed no significant differences across FUO definitions, indicating consistent clinical outcomes irrespective of diagnostic criteria. Mortality rates were comparable among different definitions, reinforcing the notion that revising FUO criteria to optimize diagnostic pathways does not compromise patient prognosis (Table 3).
| Outcome | Definition | χ² test | |||||||||
| A | B | C | D | E | F | G | H | Total | χ² | P value | |
| Alive | 37 (75.5) | 83 (89.2) | 23 (82.1) | 40 (90.9) | 0 (0.0) | 7 (100.0) | 1 (100.0) | 5 (100.0) | 196 (86.0) | 27.937 | |
| Unstable vital | 4 (8.2) | 3 (3.2) | 1 (3.6) | 1 (2.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 9 (3.9) | ||
| Poor prognosis | 0 (0.0) | 2 (2.2) | 0 (0.0) | 2 (4.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4 (1.8) | ||
| Death | 8 (16.3) | 5 (5.4) | 4 (14.3) | 1 (2.3) | 1 (100) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 19 (8.3) | ||
| Total | 49 (100.0) | 93 (100.0) | 28 (100.0) | 44 (100.0) | 1 (100.0) | 7 (100.0) | 1 (100.0) | 5 (100.0) | 228 (100.0) | ||
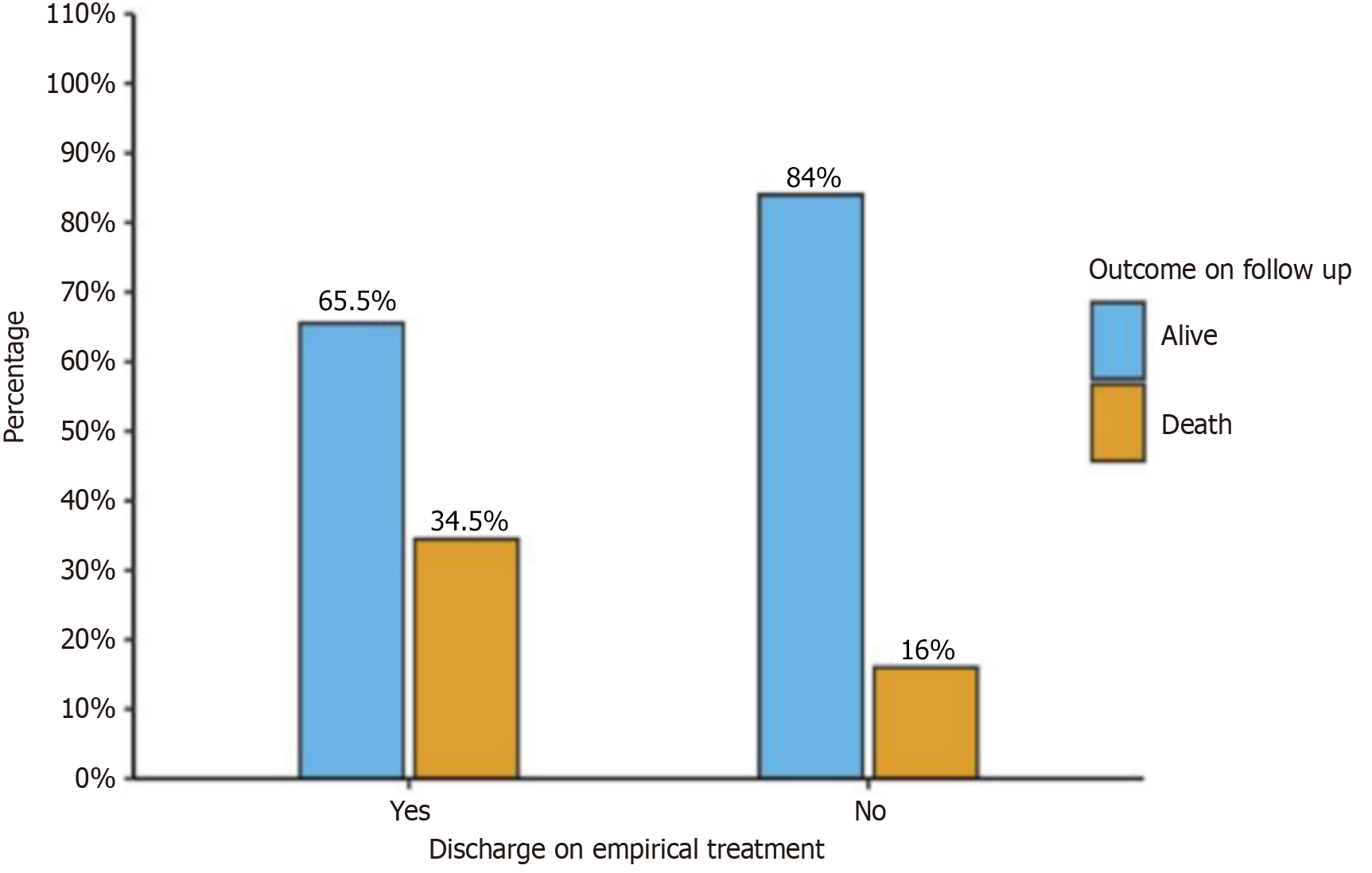
Although only 129 patients were followed up, none of the patients who were followed up required rehospitalization for fever recurrence. Among the patients discharged on empirical treatment (n = 29), 65.5% were alive at the 6-month follow-up, while 34.5% died. However, the majority of patients (n = 100) were not receiving any treatment, and only 16% who did not receive any empirical treatment died (P = 0.029) (Figure 1).
The study of FUO conducted at AIIMS Rishikesh provides valuable insights into the prevalence, etiology, and management of this challenging clinical entity in North India. This discussion expands on the implications of the study findings, compares them with the literature, and proposes recommendations for optimizing FUO diagnosis and management in resource-limited settings.
The predominance of Definition B (fever lasting 3-21 days, temperature 99.1 °F-100.9 °F, > 7 days of hospitalization) among the FUO patients in this study (40.8%) suggested that traditional criteria, such as those defined by Petersdorf and Beeson in 1961, may not adequately capture the spectrum of FUO presentations in North India[1]. The majority of patients in the present study underwent diagnostic workups and received treatment within 21 days of hospitalization. This finding resonates with previous studies advocating for broader temperature ranges and extended hospital stays to improve diagnostic yield without delaying treatment initiation[2,4].
Comparative analysis with the literature reveals consistent trends in FUO etiology and outcomes globally but underscores regional variations in disease prevalence and diagnostic challenges[5,7]. Studies from non-Western regions, including Asia and Africa, highlight endemic infections, tropical diseases, and socioeconomic factors influencing healthcare access and outcomes[8,9].
This study contributes to this body of knowledge by highlighting the unique challenges faced in diagnosing and managing FUO in North India. The high prevalence of infectious etiologies (87.1%) across all proposed definitions underscores the universal relevance of infectious diseases in FUO, necessitating targeted diagnostic approaches tailored to local epidemiological profiles[4].
Based on these findings and comparative analysis, several recommendations can be proposed to optimize FUO management in resource-limited settings such as North India, especially to develop context-specific FUO criteria that consider temperature thresholds, duration of fever, and hospital stays to capture diverse FUO presentations effectively[2,7].
This study implements structured diagnostic protocols that incorporate regional epidemiological data and resource availability to streamline FUO evaluation[4]. This includes prioritizing cost-effective diagnostic modalities and leveraging clinical judgment to initiate timely empirical therapy when indicated. This study also encourages research initiatives to further elucidate FUO epidemiology, optimize diagnostic algorithms, and evaluate emerging therapeutic modalities[3,10]. Continuous medical education programs should emphasize FUO management strategies tailored to regional healthcare contexts, fostering evidence-based clinical practice and enhancing healthcare delivery[6].
Despite its contributions, this study has several limitations that warrant consideration. The retrospective nature of the data collection and single-center design may limit the generalizability of the findings to other healthcare settings in North India[6]. This lack of detailed information may affect the accuracy and reliability of the findings. Additionally, despite attempts to contact patients for follow-up, a significant number (almost 50%) of patients were lost to follow-up. This loss to follow-up introduces potential bias and may impact the accuracy of assessing patient outcomes. Future multicenter studies incorporating larger patient cohorts and longitudinal follow-up are needed to validate the proposed FUO criteria and assess long-term outcomes across diverse patient populations.
Additionally, further research is warranted to explore the impact of socioeconomic factors, geographic variations, and emerging infectious diseases on FUO epidemiology in resource-limited settings[5,11]. This includes investigating the role of novel diagnostic technologies, such as molecular diagnostics and imaging modalities, in enhancing FUO diagnostic yield and therapeutic decision-making.
This study provides valuable evidence suggesting that the criteria for diagnosing FUO need to be revised. Adapting the criteria based on lower temperature thresholds (99.1 °F), less duration of fever (3-21 days), and extended hospital stays (> 7 days) to better reflect the local patient population's needs and resource constraints could improve the early diagnosis and management of FUO patients, ultimately leading to better patient outcomes. The prevalence of FUO according to the new definition B was 40.8%, while the prevalence according to the classical definition (definition H) was 2.2%. There was significantly greater mortality among FUO patients who were discharged with empirical therapy, mostly anti-tu
We extend our sincere gratitude to the various subspecialty departments involved in this study for their invaluable support and resources. We also acknowledge the contributions of our mentors and colleagues whose insights and guidance significantly enriched this research. Our heartfelt thanks go to the study participants for their cooperation and contribution. Finally, we recognize the role of anonymous reviewers and prior researchers whose work laid the foundation for this study. Their collective efforts were instrumental in the successful completion of this work.
| 1. | Petersdorf RG, Beeson PB. Fever of unexplained origin: report on 100 cases. Medicine (Baltimore). 1961;40:1-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 766] [Cited by in RCA: 700] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 2. | Kumar N, Kapoor M, Panda PK, Singh Y, Bhadoria AS, Dhar M. Quantitative Definition of Fever Needs a Change: A Longitudinal Study from the Hospital Workers and their Family Members. J Clin Diagn Res. 2022;. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Jiang L, Wu H, Zhao S, Zhang Y, Song N. Structured diagnostic scheme clinical experience sharing: a prospective study of 320 cases of fever of unknown origin in a tertiary hospital in North China. BMC Infect Dis. 2023;23:452. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Knockaert DC, Vanderschueren S, Blockmans D. Fever of unknown origin in adults: 40 years on. J Intern Med. 2003;253:263-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 160] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 5. | Zhai YZ, Chen X, Liu X, Zhang ZQ, Xiao HJ, Liu G. Clinical analysis of 215 consecutive cases with fever of unknown origin: A cohort study. Medicine (Baltimore). 2018;97:e10986. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Pannu AK, Golla R, Kumari S, Suri V, Gupta P, Kumar R. Aetiology of pyrexia of unknown origin in north India. Trop Doct. 2021;51:34-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Mir T, Nabi Dhobi G, Nabi Koul A, Saleh T. Clinical profile of classical Fever of unknown origin (FUO). Caspian J Intern Med. 2014;5:35-39. [PubMed] |
| 8. | Bleeker-Rovers CP, Vos FJ, de Kleijn EMHA, Mudde AH, Dofferhoff TSM, Richter C, Smilde TJ, Krabbe PFM, Oyen WJG, van der Meer JWM. A prospective multicenter study on fever of unknown origin: the yield of a structured diagnostic protocol. Medicine (Baltimore). 2007;86:26-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 244] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 9. | Tabak F, Mert A, Celik AD, Ozaras R, Altiparmak MR, Ozturk R, Aktuglu Y. Fever of unknown origin in Turkey. Infection. 2003;31:417-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Roth AR, Basello GM. Approach to the adult patient with fever of unknown origin. Am Fam Physician. 2003;68:2223-2228. [PubMed] |
| 11. | Leal HF, Azevedo J, Silva GEO, Amorim AML, de Roma LRC, Arraes ACP, Gouveia EL, Reis MG, Mendes AV, de Oliveira Silva M, Barberino MG, Martins IS, Reis JN. Bloodstream infections caused by multidrug-resistant gram-negative bacteria: epidemiological, clinical and microbiological features. BMC Infect Dis. 2019;19:609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |