Published online Oct 20, 2020. doi: 10.5412/wjsp.v10.i2.3
Peer-review started: June 18, 2020
First decision: July 25, 2020
Revised: August 23, 2020
Accepted: September 25, 2020
Article in press: September 25, 2020
Published online: October 20, 2020
Cholangioscopy has been described in case reports and series to facilitate guidewire placement in difficult benign biliary strictures. Specifically, it has been infrequently used in difficult benign anastomotic liver transplant biliary strictures to visualize the stricture orifice for guidewire placement. Here we describe a case of guidewire placement through a difficult malignant biliary stricture using single operator cholangioscopy.
A 74-year-old female presented with jaundice and weight loss. Endoscopic ultrasound and endoscopic retrograde cholangiopancreatography (ERCP) by other endoscopists demonstrated pancreatic adenocarcinoma with a dilated cystic duct (CD) and proximal common bile duct (CBD). The associated distal CBD stricture was dilated and stented with a plastic stent. However she subsequently developed cholangitis, prompting referral for a repeat ERCP. The stent was found to have migrated distally to the confluence of the dilated CD and CBD stricture. Despite using multiple hydrophilic guidewires, the stricture could not be traversed due to preferential wire passage into the dilated CD. SpyGlass DS (Boston Scientific Corp, Marlborough, MA, United States) was then used to visualize the orifices of the CD and CBD stenosis, enabling the guidewire to be placed directly through the stricture into the proximal CBD. A WallFlex covered metal stent (Boston Scientific Corp, Marlborough, MA, United States) was successfully placed, resulting in resolution of her cholangitis.
To our knowledge, this is one of the first cases to describe successful cholangioscopic guidewire placement for malignant biliary strictures.
Core Tip: Cholangioscopy has been described in case reports and series to facilitate guidewire placement in difficult benign biliary strictures, especially in the setting of liver transplants. Most biliary strictures are successfully traversed with standard techniques utilizing hydrophilic guidewires during endoscopic retrograde cholangiopancreatography, but challenges with difficult wire placement can occur when the biliary tree consists of multiple strictures and sharp angulations. Here we describe a case of guidewire placement through a difficult malignant biliary stricture using single operator cholangioscopy, highlighting the versatility of cholangioscopy especially in anatomically challenging patients.
- Citation: Kim GE, Lo DYA. Cholangioscopy-assisted guidewire placement in a malignant biliary stricture: A case report. World J Surg Proced 2020; 10(2): 3-8
- URL: https://www.wjgnet.com/2219-2832/full/v10/i2/3.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v10.i2.3
Cholangiopancreatoscopy allows direct visualization of biliary and pancreatic ducts, and it remains an adjunct to fluoroscopic evaluation during endoscopic retrograde cholangiopancreatography (ERCP)[1]. Diagnostic and therapeutic applications of cholangiopancreatoscopy include evaluation and tissue sampling of indeterminate and malignant pancreaticobiliary strictures, and lithotripsy of difficult stones[2-6]. Selective biliary guidewire access utilizing cholangioscopy to directly visualize ductal anatomy for guidewire placement has been described previously in the cystic duct and anastomotic benign biliary strictures due to liver transplant[1,3-7], and more recently in malignant strictures[8]. Here we describe a case of guidewire placement through a difficult malignant biliary stricture using single operator cholangioscopy.
Epigastric pain.
A 74-year-old female initially presented with epigastric pain, nausea, and vomiting. She also endorsed having increasing fatigue, weight loss, and back pain for the past few months. Upon further questioning, she also reported being more “tanned” for the several weeks for which she attributed to significant sun exposure. She denied alcohol or tobacco use.
Her past medical history is significant for atrial fibrillation, hypothyroidism, and gastroesophageal reflux disease, and her surgical history is notable for thyroidectomy and total abdominal hysterectomy with bilateral salpingo-oophorectomy. She did not drink alcohol or smoke tobacco.
Family history was negative for any chronic gastrointestinal diseases.
Upon examination, she was markedly jaundiced with mild epigastric tenderness, without any palpable mass.
Her laboratory markers were notable for a total bilirubin of 10 mg/dL (reference range 0.1-1.4 mg/dL), alkaline phosphatase of 515 IU/L (reference range 30-140 IU/L), and aspartate aminotransferase and alanine aminotransferase of 148 IU/L and 174 IU/L (reference range 7-40 IU/L and 10-65 IU/L, respectively). White blood cell count was within normal limits at 6.4 × 109/L (reference range 4.0-10.8 × 109/L).
The initial computed tomography of abdomen and pelvis demonstrated a 4.3 cm mass in the pancreatic head causing a biliary stricture. Given the clinical presentation with painless jaundice and weight loss, pancreatic adenocarcinoma was high on the differential.
Endoscopic ultrasound at the time showed a 30 mm × 26 mm mass in the pancreatic head with common bile duct (CBD) and pancreatic duct obstruction, staged as T3N1Mx. Fine needle aspiration revealed adenocarcinoma, and ERCP demonstrated markedly dilated cystic duct (CD) and proximal common bile duct (CBD).
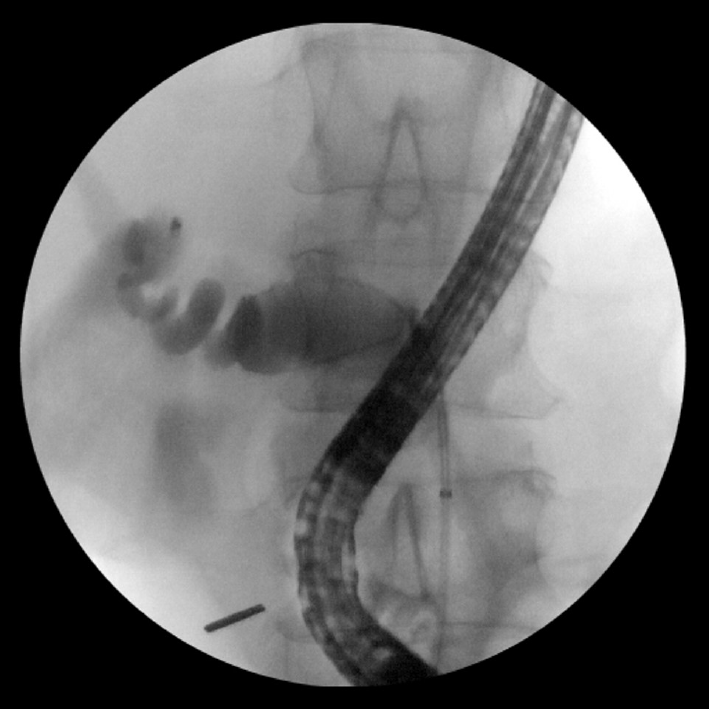
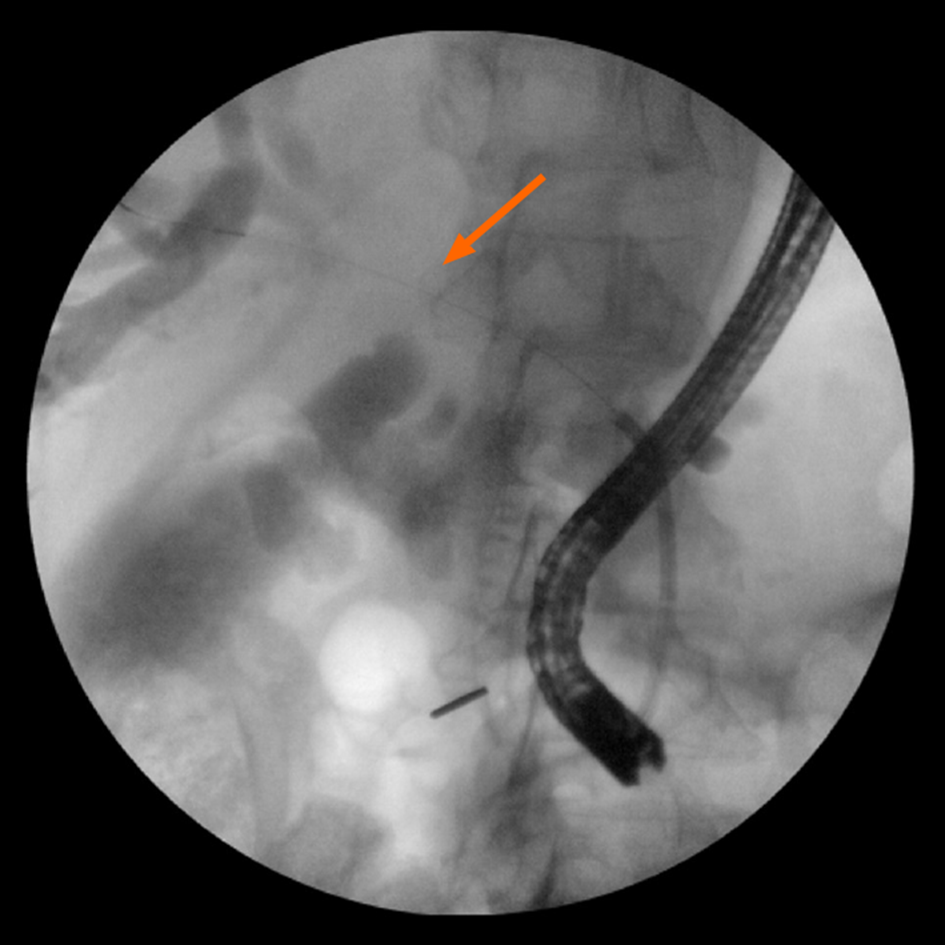
The associated distal CBD stricture was dilated with an 8 mm balloon and stented with a 10 Fr stent. However, the patient persisted to have jaundice and subsequently developed cholangitis two days later, prompting a referral for a repeat ERCP. The previously-placed biliary stent was found to have migrated distally to the confluence of the markedly dilated cystic duct and high-grade CBD stricture (Figure 1). Despite using multiple hydrophilic guidewires, the stricture could not be traversed due to preferential wire passage into the dilated cystic duct. SpyGlass DS (Boston Scientific Corp, Marlborough, MA, United States) was then used to visualize the orifices of the cystic duct and CBD stenosis (Figure 2), enabling the guidewire to be placed directly through the stricture into the proximal CBD (Figure 3). A 10 mm × 80 mm WallFlex fully-covered metal stent (Boston Scientific Corp, Marlborough, MA, United States) was successfully placed in the CBD.
Patient's abdominal pain and elevated transaminases resolved to normal limits on follow up appointment, and patient was referred to oncology for further management of her pancreatic adenocarcinoma.
Most biliary strictures are successfully traversed with standard techniques utilizing hydrophilic guidewires during ERCP, but challenges with difficult wire placement can occur when the biliary tree consists of severe strictures and sharp angulations. Techniques used to combat this problem include varying the angle of approach to the papilla and biliary tree, along with changing the cannulation device and guidewire type, which can optimize the guidewire’s alignment with the axis of the stricture. Despite these measures, there may still be difficulty in selective biliary access, which can lead to prolonged procedure time, increased risk for post-procedure adverse events, and need for repeat ERCP or possibly a more invasive approach such as EUS-rendezvous, percutaneous or surgical intervention[9,10].
In difficult stricture cases, single operator cholangioscopy provides direct visualization of the ducts, facilitating wire access for therapeutic stenting. This method has been described previously with technical success achieved in anastomotic biliary strictures in liver transplant patients[11,12,13], as well as cystic duct stone removal and stenting[14]. More recently, a small case series (seven cholangiocarcinomas, one pancreatic carcinoma, and three unspecified malignancies) noted a collective success rate of 46% for selective duct access in malignant strictures, as compared to a higher success rate of 88% for benign etiologies[8]. The series did not discuss which malignant cases were unsuccessful, and the Bismuth classification of strictures, which could impact the success rate.
In our patient, the CBD stricture and severely dilated cystic duct emerged in the same vicinity, which resulted in preferential guidewire placement in the latter. This unique situation made it technically challenging to traverse the guidewire through the stricture. Utilizing cholangioscopy to visualize and characterize the specifics of the stricture orifice enabled optimal manipulation of the guidewire to correctly access the stricture for successful stenting and biliary decompression.
Cholangiopancreatoscopy is becoming increasingly popular and more ubiquitous in its application, ranging from diagnostic biopsy of biliary strictures to therapeutic lithotripsy of gallstones[2,15-17]. To our knowledge, this is one of the first cases to describe using cholangioscopy for a successful guidewire placement in a malignant biliary stricture from pancreatic cancer, further highlighting its versatility. Cholangioscopy is an effective tool for accurate guidewire placement in difficult benign as well as malignant biliary strictures, and further studies are warranted to evaluate the success rate as well as the financial costs of utilizing cholangioscopy for difficult malignant strictures.
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chow WK, Fu TL, Sperti C S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Petersen BT. Cholangioscopy for special applications: primary sclerosing cholangitis, liver transplant, and selective duct access. Gastrointest Endosc Clin N Am. 2009;19:579-586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Moon JH, Terheggen G, Choi HJ, Neuhaus H. Peroralcholangioscopy: diagnostic and therapeutic applications. Gastroenterology. 2013;144:276-282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Chathadi KV, Chen YK. New kid on the block: development of a partially disposable system for cholangioscopy. Gastrointest Endosc Clin N Am. 2009;19:545-555. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Draganov PV, Lin T, Chauhan S, Wagh MS, Hou W, Forsmark CE. Prospective evaluation of the clinical utility of ERCP-guided cholangiopancreatoscopy with a new direct visualization system. Gastrointest Endosc. 2011;73:971-979. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 77] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Chen YK, Pleskow DK. SpyGlass single-operator peroralcholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video). Gastrointest Endosc. 2007;65:832-841. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 310] [Cited by in F6Publishing: 333] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 6. | Ramchandani M, Reddy DN, Lakhtakia S, Tandan M, Maydeo A, Chandrashekhar TS, Kumar A, Sud R, Rerknimitr R, Makmun D, Khor C. Per oral cholangiopancreatoscopy in pancreatico biliary diseases--expert consensus statements. World J Gastroenterol. 2015;21:4722-4734. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 35] [Cited by in F6Publishing: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Shah RJ, Langer DA, Antillon MR, Chen YK. Cholangioscopy and cholangioscopic forceps biopsy in patients with indeterminate pancreaticobiliary pathology. Clin Gastroenterol Hepatol. 2006;4:219-225. [PubMed] [Cited in This Article: ] |
| 8. | Bokemeyer A, Gross D, Brückner M, Nowacki T, Bettenworth D, Schmidt H, Heinzow H, Kabar I, Ullerich H, Lenze F. Digital single-operator cholangioscopy: a useful tool for selective guidewire placements across complex biliary strictures. Surg Endosc. 2019;33:731-737. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Rerknimitr R, Sherman S, Fogel EL, Kalayci C, Lumeng L, Chalasani N, Kwo P, Lehman GA. Biliary tract complications after orthotopic liver transplantation with choledochocholedochostomy anastomosis: endoscopic findings and results of therapy. Gastrointest Endosc. 2002;55:224-231. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 218] [Cited by in F6Publishing: 231] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 10. | Verdonk RC, Buis CI, Porte RJ, van der Jagt EJ, Limburg AJ, van den Berg AP, Slooff MJ, Peeters PM, de Jong KP, Kleibeuker JH, Haagsma EB. Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl. 2006;12:726-735. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 214] [Cited by in F6Publishing: 222] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 11. | Wright H, Sharma S, Gurakar A, Sebastian A, Kohli V, Jabbour N. Management of biliary stricture guided by the Spyglass Direct Visualization System in a liver transplant recipient: an innovative approach. Gastrointest Endosc. 2008;67:1201-1203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Kumar S. Cholangioscopy-directed endoscopic intervention for post-liver transplantation anastomotic biliary stricture. Gastrointest Endosc. 2015;81:1014-1015. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Woo YS, Lee JK, Noh DH, Park JK, Lee KH, Lee KT. SpyGlasscholangioscopy-assisted guidewire placement for post-LDLT biliary strictures: a case series. Surg Endosc. 2016;30:3897-3903. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Parsi MA. Peroralcholangioscopy-assisted guidewire placement for removal of impacted stones in the cystic duct remnant. World J Gastrointest Surg. 2009;1:59-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Navaneethan U, Moon JH, Itoi T. Biliary interventions using single-operator cholangioscopy. Dig Endosc. 2019;31:517-526. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Salerno R, Mezzina N, Ardizzone S. Endoscopic retrograde cholangiopancreatography, lights and shadows: Handle with care. World J Gastrointest Endosc. 2019;11:219-230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 8] [Cited by in F6Publishing: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Badshah MB, Vanar V, Kandula M, Kalva N, Badshah MB, Revenur V, Bechtold ML, Forcione DG, Donthireddy K, Puli SR. Peroralcholangioscopy with cholangioscopy-directed biopsies in the diagnosis of biliary malignancies: a systemic review and meta-analysis. Eur J Gastroenterol Hepatol. 2019;31:935-940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |