Copyright
©The Author(s) 2015.
World J Immunol. Nov 27, 2015; 5(3): 152-159
Published online Nov 27, 2015. doi: 10.5411/wji.v5.i3.152
Published online Nov 27, 2015. doi: 10.5411/wji.v5.i3.152
Figure 1 Patients with Sjögren’s syndrome develop an autoimmune response that has systemic and local (anti-exocrine gland) components.
Both responses are most obviously manifested by the presence of autoantibodies directed, respectively, against ubiquitous (e.g., Ro) and tissue-specific (e.g., muscarinic receptor 3) antigens. The anti-exocrine gland response is also notable by the presence of chronic inflammatory cellular infiltrates composed of activated lymphocytes. Autoantibodies contribute to systemic manifestations through immune complex deposition, but also contribute to sicca symptoms by affecting cholinergic function and causing acinar cell apoptosis. Cellular infiltrates directly affect exocrine gland function by inducing local inflammatory damage and local B cell proliferation probably precedes lymphoma development. Injury to acinar cells perpetuates the local immune response by releasing antigens and inflammatory mediators (e.g., IL-1, type I IFN). IL-1: Interleukin-1; IFN: Interferon.
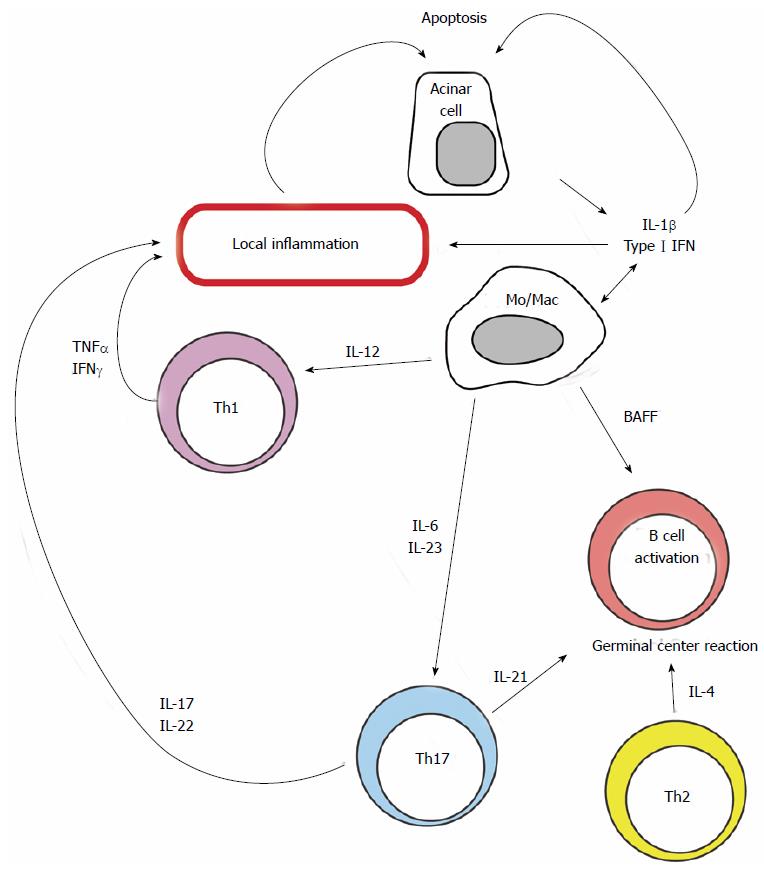
Figure 2 T cells and B cells are recruited into exocrine glands where they mount a chronic inflammatory response.
Local production of IL-1β and type I interferons (IFN) by epithelial cells and innate immune cells contributes to local inflammation and promotes apoptosis of acinar cells. Clones of activated T cells with varied effector differentiation support local inflammation and contribute to acinar destruction. IL: Interleukin; BAFF: B cell activating factor.
- Citation: Crispín JC, Rosetti F, Hernández-Molina G. Lessons from Sjögren’s syndrome etiopathogenesis: Novel cellular and molecular targets. World J Immunol 2015; 5(3): 152-159
- URL: https://www.wjgnet.com/2219-2824/full/v5/i3/152.htm
- DOI: https://dx.doi.org/10.5411/wji.v5.i3.152