Published online Aug 8, 2016. doi: 10.5409/wjcp.v5.i3.262
Peer-review started: January 30, 2016
First decision: February 29, 2016
Revised: April 26, 2016
Accepted: May 17, 2016
Article in press: May 27, 2016
Published online: August 8, 2016
Intracranial incidental findings on magnetic resonance imaging (MRI) of the brain continue to generate interest in healthy control, research, and clinical subjects. However, in clinical practice, the discovery of incidental findings acts as a “distractor”. This review is based on existing heterogeneous reports, their clinical implications, and how the results of incidental findings influence clinical management. This draws attention to the followings: (1) the prevalence of clinically significant incidental findings is low; (2) there is a lack of a systematic approach to classification; and discusses (3) how to deal with the detected incidental findings based a proposed common clinical profile. Individualized neurological care requires an active discussion regarding the need for neuroimaging. Clinical significance of incidental findings should be decided based on lesion’s neuroradiologic characteristics in the given clinical context. Available evidence suggests that the outcome of an incidentally found “serious lesion in children” is excellent. Future studies of intracranial incidental findings on pediatric brain MRI should be focused on a homogeneous population. The study should address this clinical knowledge based review powered by the statistical analyses.
Core tip: The magnetic resonance imaging of the brain in children frequently reveals incidental findings. There is paucity in the literature, how to deal with such findings in clinical practice. This review based on existing heterogeneous reports reveals that the prevalence of clinically significant incidental findings is low and discusses options in the management of incidental findings in children.
- Citation: Gupta SN, Gupta VS, White AC. Spectrum of intracranial incidental findings on pediatric brain magnetic resonance imaging: What clinician should know? World J Clin Pediatr 2016; 5(3): 262-272
- URL: https://www.wjgnet.com/2219-2808/full/v5/i3/262.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v5.i3.262
Magnetic resonance imaging (MRI) of the brain is the most commonly performed investigation in the practice of pediatric neurology. During a clinical evaluation, an unexpected finding on brain MRI is a common occurrence. This heightens parental anxiety and generates explanatory discrepancies amongst physicians. Discovery of such findings on neuroimaging is not unique or limited to pediatric brain MRI. Rather, it has been reported in several other conditions such as abdominal and pelvic computerized tomography (CT) and MRI[1] or in asymptomatic ankles[2]. Additionally, these findings have been described in asymptomatic healthy volunteer adults[3], young adults in the community, and in clinic-based subjects[4].
In clinical practice, MRI of the brain is performed for a variety of indications. Infrequently, findings like pituitary adenoma, lesions of the pineal gland, or central nervous system malignancy are discovered, which have serious implications.
Authors present the evidence-based reports of the current body of knowledge regarding such findings, their clinical implications, and how these findings translate to neurologic management, and discuss a common profile to aid in the clinical management of incidental finding.
In November 2014, we searched Ovid MEDLINE and PubMed databases for reports on the use of brain MRI in children aged 18 years and under. We supplemented the electronic searches with surveillance of electronic tables of contents in neurological journals and by hand searching the bibliographies of pertinent articles. Two authors (Gupta SN and White AC) read the title and abstract of every study identified by the electronic searches. We critically appraised the full text of potentially eligible studies. Two authors extracted data on study design, population characteristics, and MRI parameters from each study.
Several prospective and retrospective studies have reported incidental findings in pediatric patients. The MRIs of the brain were carried out as an investigatory step in children presenting within various disciplines of pediatric medicine. The summary of identified studies is provided in the Table 1[5-22].
| Ref. | Country | Study objective /conclusion |
| Yilmaz et al[5] | Turkey | To evaluate clinical significance of MRI abnormality in children with headache/ |
| Despite the high rate of IFs, the yield is non-contributory to diagnosis and therapy | ||
| Bayram et al[6] | Turkey | To describe the prevalence of WML detected on MRI in children with headaches/ Non-specific WML may be seen in children with headache. In the absence of benefit, repeated MRI studies are unwarranted. It should be tailored according to clinical course |
| Graf et al[7] | United States | Studied the frequency and consequences of IFs on non-acute pediatric headache/ |
| The frequency and types of all IFs were generally comparable to previous studies | ||
| Schwedt et al[8] | United States | To study the frequency of “benign” abnormalities in children with headache, compare it with the frequency of MRI findings that dictate a change in patient management/ |
| About 20% children with headache have benign findings that do not result in a change in management which rarely occurred in 1.2% of children in this study | ||
| Koirala[9] | Nepal | To evaluate the yield of MRI findings in patients with seizure/ |
| The majority of abnormalities on MRI included hippocampal sclerosis and T2 hyperintensity | ||
| Kalnin et al[10] | United States | To characterize IFs association with seizure onset and to standardize a classification system/ |
| The MRI and a standardized scoring system demonstrated a higher rate of IFs than previously reported. MRI parameters need to expand the definition of significant IFs | ||
| Gupta et al[11] | United States | To test the hypothesis that children with developmental delay are more likely to have incidental findings than are the children with normal development status/ |
| Authors reported a higher prevalence of IFs in children with developmental delay as compared with those with normal development status | ||
| Seki et al[12] | Japan | To report prevalence of IFs in healthy children and to suggest an ethical and practical management protocol/ |
| The prevalence of IFs was high but those requiring further MRI was low. Evaluating equivocal findings was the most difficult part of IFs management | ||
| Gupta et al[13] | United States | To elucidate the prevalence of incidental findings in a general pediatric neurology practice/ |
| Authors reported a high prevalence of and a low rate of referrals in comparison to previous studies. This study may help guide management decisions and discussions | ||
| Potchen et al[14] | Malawi | To collect normative magnetic resonance imaging data for clinical and research applications/ |
| Incidental brain magnetic resonance abnormalities are common in Malawian children | ||
| Kim et al[15] | United States | To elucidate the prevalence of incidental findings in a healthy pediatric population/ |
| Frequency of important IFs was not high. But, awareness of neurologic status, the presence and variety of IFs are of vital importance for research and welfare of the child | ||
| Incidental findings in pediatric specialty clinic other than neurology | ||
| Oh et al[16] | South Korea | To investigated the clinical characteristics of children in whom Rathke’s cleft cysts were incidentally discovered and the treatment response with endocrinopathy/ |
| Rathke’s cleft cysts less than 20 mm expressing cystic intensity can be treated medically | ||
| Rachmiel et al[17] | Canada | To assess IFs in children with congenital hypothyroidism compared to 38 healthy controls/ |
| Both groups had a similar incidence of structural abnormalities. There was no association between those findings and neurocognitive function | ||
| Whitehead et al[18] | United States | The prevalence of pineal cysts in children who have had high-resolution 3T brain MRI/ |
| Characteristic-appearing pineal cysts are benign findings. In lack of no referable comprehensive symptoms, no follow-up is required | ||
| Mogensen et al[19] | Denmark | To evaluate the outcome of brain MRI in girls referred with early signs of puberty/ |
| Girls with central precocious puberty should have a brain MRI | ||
| Perret et al[20] | Switzerland | The prevalence and management options of incidentally found mass lesions at pediatric clinic/ |
| A subgroup of lesions such as tectal glioma and dysembryoplastic neuroepithelial tumor can be monitored conservatively | ||
| Jordan et al[21] | United States | The prevalence of incidental findings on brain MRI in children with sickle cell disease/ |
| IFs were present in 6.6% patients and a potentially serious or urgent finding was 0.6% | ||
The word “incidental or unexpected” generally applies when an identified brain lesion on neuroimaging would have not been predicated by clinicians. This definition can be questioned by some in specific clinical situation. Because the discovery of such lesions in the majority of children does not alter the management, some authors have described them as “benign findings”, Schwedt et al[8], 2006.
Multiple terminology have been used to indicate white matter lesions such as periventricular malacia, periventricular white matter changes, white-matter hyperintensity, non-specific white matter abnormalities, white matter signal abnormality, and focal white matter lesion. In the exception to periventricular malacia, the question is if the rest of these terms are the same or of different pathologies. Clinicians have been charged with the task of determining whether or not these definitions are synonymous.
Intracranial incidental findings are inconsistently classified. The most findings being classified based upon their clinical significance, the type of lesion, normal variant vs abnormal finding, and the urgency for the referral.
Jordan et al[21], 2010, based on the need for referral, classified incidental finding into four categories: No referral, routine referral, urgent referral, or immediate referral. Graf et al[7], 2010 categorized neuroimaging results as normal, remarkable without clinical action, remarkable with clinical follow-up action, and abnormal. Bryan et al[23], 1994 used a very different classification, but a similar method which is used to classify the Cardiovascular Health Study in adults.
Yilmaz et al[5], 2014 classified incidental findings in five categories as follows: (1) cerebral abnormalities relevant to headache such as a growing tumor or hydrocephalus; (2) incidental cerebral abnormalities with potential clinical significance such as Chiari type I malformations, arachnoid cysts, cysts of pineal gland, and inflammatory lesions; (3) incidental cerebral abnormalities without clinical significance such as white matter hyperintensity, periventricular leukomalacia, subtle gliosis, silent brain infarcts or lacune, and brain microbleeds; (4) extra-cerebral abnormalities relevant to headache such as sinusitis, which was considered as the cause of headache if an otolaryngologist made the diagnosis of sinusitis; and (5) incidental extra-cerebral abnormalities such as mucosal thickening or fluid retention in sinuses or mastoid cells.
The inclusion of “normal-variants” is confusing. For example, commonly occurring pineal cysts are an asymptomatic finding. Thus, this could be considered a normal finding[24]. But in a symptomatic patient with the same pineal cyst, there may be a true clinical implication[25,26]. In some patients, a particular finding in the context of clinical presentation after all may not be incidental. Occasionally, certain findings such as arachnoid cyst may be predicted in specific clinical situations[27,28].
Some of these findings are classified arbitrarily. This practice has resulted in a variety of classification systems which lack clarity. There is an obvious need for a uniform classification system.
MRI acquisition modalities and the parameters utilized in these studies are variable.
The conventional MRI was usually performed by using 1.5 Tesla magnetic field strengths scanner. MRI parameters varied but conventional short-TR and short-TE, T1-weighted, long-TR and long-TE, T2-weighted, and fast fluid-attenuated inversion recovery-weighted images were performed in majority of patients. Diffusion and perfusion diffusions images were routinely available in North American Practice of Pediatric Neurology/Neuroradiology.
Diffusion tensor imaging is an application of diffusion weighted imaging which quantifies water diffusion by measuring molecular motion of water within the brain parenchyma. Lately, this modality has been increasingly used in studying the neuroanatomy of the brain[29]. This technique is useful particularly in the investigation of white matter abnormalities.
Official interpretations are provided by different levels of trained and Board Certified Radiologists. A very limited number of MRI studies were reviewed by Board Certified Pediatric Neuroradiologists. The reporting procedure remains subjective.
The reports should distinguish cerebellar ectopia (downward displacement of cerebellar tonsil/s less than 1 cm through foramen magnum) from Chiari type I malformation. In the face of recent genetic and phenotypic correlation, there has been a retreat from the Dandy Walker “variant”, thus it may be useful to just describe the posterior fossa abnormality. Most importantly, in case of serious lesions, the radiologic characteristics particularly the integrity of the blood-brain barrier should be described in detail.
Future studies may reveal the association between a patient’s clinical status and the type of finding, while advances in neuroimaging may reveal their significance. Radiologists should report all such findings within the body of the text, in addition to their subjective interpretation.
The clinical demography of intracranial incidental findings is shown in Tables 2 and 3.
| Ref. | Clinical demographics | Girls n (%) with MRI | ||||
| Study- setting | Reason for MRI | No. ofsubject | No. ofMRI (%) | Mean age(range) year | ||
| Yilmaz et al[5] | Pediatric neurology | Head pain | 449 | 288 (64)1 | 11.2 (NA) | 189 (58) |
| Bayram et al[6] | 941 | 527 (61)2 | 12.1 (4-16) | NA | ||
| Graf et al[7] | 400 | 91 (23)2 | 10.8 (3-18) | NA | ||
| Schwedt et al[8] | 681 | 218 (32)2 | 12.1 (2-18)3 | 126 (52) | ||
| Koirala[9] | Pediatric and adult neurology | Seizure | 36c | 36 (100)3 | NA (1-16) | NA |
| Kalnin et al[10] | Radiology | 349 | 281 (81) | 9.7 (6-14) | 143 (51) | |
| Gupta et al[11] | Pediatric neurology | Developmental delay | 2185 | 771 (35) | 7.6 (NA ) | 433 (56) |
| Gupta et al[13] | General | 1618 | 666 (41) | 9.8 (0-21) | 280 (42) | |
| Seki et al[12] | Research Institute | Healthy children | 395 | 89 (25)1 | NA (5-8) | 53 (44) |
| Kim et al[15] | Radiology | 225 | 198 (88)1 | 11.2 (1 mo-18) | 126 (56) | |
| Research | ||||||
| Potchen et al[14] | Community-based | 102 | 68 (71)1 | 12.1 (9-14) | 54 (55) | |
| Ref. | Study-setting | Reason for MRI | No. of subject | No. of MRI (%) | Clinical demographics | |
| Mean age(range) year | Girls n (%) with MRI | |||||
| Oh et al[16] | Endocrinology | Rathke’s cleft cysts | 341 | 26 (76) | NA (4-18) | 17 (65) |
| Rachmiel et al[17] | Endocrinology | Congenital hypothyroidism | 682 | 30 (100) | 12.5 (10-15) | 16 (55) |
| Whitehead et al[18] | Radiology | Pineal cyst | 100 | 100 (100) | 6.8 (1 mo-17) | 52 (52) |
| Mogensen et al[19] | Endocrinology | Early puberty | 229 | 207 (100)3 | NA (6-9) | 207 (100) |
| Perret et al[20] | Oncology | Primary brain tumor4 | 335 | 335 (100) | 7.6 (0-18) | 132 (39) |
| Jordan et al[21] | Neurology research | Sickle cell disease | 953 | 953 (100) | 9.2 (5-15) | 460 (48) |
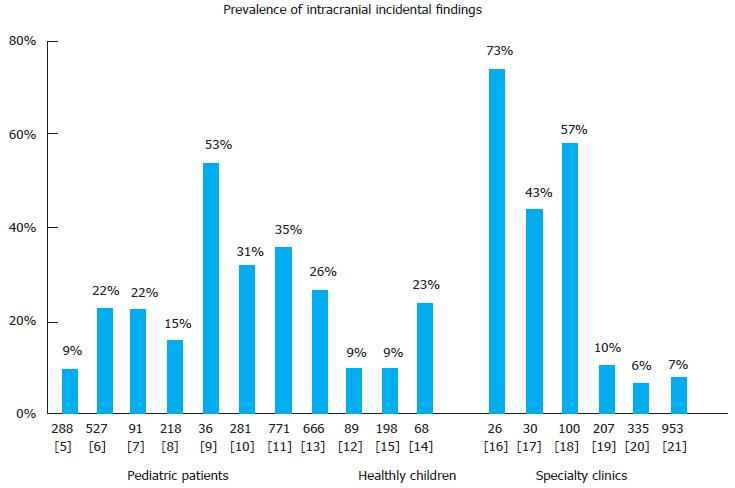
The prevalence of intracranial incidental findings is shown in Figure 1.
Variability in prevalence, lowest in healthy children (8%) and the highest in a specific neurologic condition can be explained by an increasing burden of a disorder on the brain. This is probably highest in an elderly brain secondary to ischemic injury particularly to white matter. Arguably, some of the white matter changes are expected findings in neurofibromatosis type I.
Despite suggestions that prevalence rate of incidental findings have increased with frequent use of neuroimaging, during the past decade, it has remained stable in children referred for non-acute headache, Graf et al[30], 2008. Of note, an increasing proportion of neuroimaging studies are being ordered by primary care providers.
The three most commonly reported intracranial incidental findings on brain MRI in various pediatric settings are shown in Table 4. The types of incidental findings on MRI outside of a neurology-setting were generally comparable in these studies.
| Ref. | Three most common intracranial IFs, n (%) | Comment or serious finding |
| Yilmaz et al[5] | White-matter hyperintensity 14 (4.3) Old infarcts 4 (1.2), and CM I 3 (0.9) | 2 (0.6%) malignant tumor and 1 hydrocephalus, 0.3% IFs were relevant to headache |
| Bayram et al[6] | Supratentorial non-specific WMC 23 (4.4) | All patients with IFs had normal development and no seizures or head trauma |
| Graf et al[7] | CM I 6 (15), arachnid cysts 6 (15), brain stem parenchymal abnormality, 4 (10) | Brain stem IFs included Dandy-Walker variant, cerebellar calcification, and tectal plate hyperintensity |
| Schwedt et al[8] | CM I 11 (4.6), nonspecific white matter abnormalities 7 (2.9), venous angiomas and arachnoid cyst each 5 (2.5) | Discovery of 4 tumors, 4 old infarcts, 3 CM I, and 2 moyamoya required a change in management |
| Koirala[9] | Hippocampal sclerosis, T2 hyperintense foci in various distributions, both 4 (21) each, cortical atrophy 3 (16) | Study focus was IFs in patient with seizure. The lesions were better detected by MRI than computerized tomography |
| Kalnin et al[10] | Ventricular enlargement 143 (51), leukomalacia/gliosis 64 (23), heterotopias and cortical dysplasia 33 (12) | Temporal lobe lesions were detected 15%, a higher frequency than in previous studies |
| Gupta et al[11] | Variant signal intensity 30 (18), WMC changes 23 (13), and PVL, 10 (6) | IFs were reported in children with developmental delay as to those with normal development status |
| Seki et al[12] | Cavum septi pellucid 6 (15) and Pineal cyst 2 (5 ), Enlarged perivascular spaces 1 (2.5) | Focus of the study was reporting of extracranial IFs in healthy children |
| Gupta et al[13] | CM I and cerebellar ectopia, 16 (3.5), Arachnoid cysts, 12 (1.8) | White matter changes were the most common IFs classified under normal-variants |
| Potchen et al[14] | PVW matter changes/gliosis 6 (6), mild diffuse atrophy 4 (4), and Empty sella 3 (3) | Incidental findings were unassociated with age, sex, antenatal problems, or febrile seizures |
| Kim et al[15] | Focal white matter lesion 3 (1.3), arachnoid cyst, frontal venous angioma, and mega cisterna magna, all three 2 (0.9) each | IFs were detected on 225 conventional research in a cohort of neurologically healthy children |
| IFs in pediatric specialty clinics other than neurology | ||
| Oh et al[16] | Low signal intensities on T1-WI and high signal intensities on T2-WI 26 (73) | Incidence of hypointensity on T1-WI was higher in patients with Rathke’s cleft cysts |
| Rachmiel et al[17] | Prominent VR perivascular spaces, cerebellar ectopia, and abnormalities in sella region all 3 (7.9) each | The comparative study found no IFs association with clinical and cognitive abnormalities |
| Mogensen et al[19] | Arachnoid cysts 5 (9.2), of which one patient had hydrocephalus | Incidental findings were unrelated to early puberty |
It should be noted that community or general pediatric neurology based studies in healthy subjects have not reported serious or progressively worsening incidentally identified lesions. Nonetheless, serious lesions have been reported by a few studies which are shown in the Table 5[31].
| Ref. | The context in which brain MRI was ordered | Worsening course | Outcome/comment | |
| Known | Potential | |||
| Yilmaz et al[5] | Children mean age 11.2 yr presented for headache evaluation | Malignant brain tumor and hydrocephalus | Chiari I malformation I; Relevant to headache | Tissue type of tumor in study was unspecified |
| Schwedt et al[8] | Children mean age 12.1 yr presented for headache evaluation | Tumors, moyamoya disease, and demyelinating disease | Arteriovenous malformation and intracerebral hemorrhage | Study focus was “benign” imaging abnormalities, no further information for serious lesion other than pineal tumor was available |
| Kalnin et al[10] | Children mean age 9.7 yr presented for the first onset seizure | None | Temporal lobe lesions | Various Epileptic abnormalities1 have been associated with pediatric brain MRI |
| Potchen et al[14] | Community-based children mean age 12.1 yr | Granulomas with gliosis | Empty sella and vermian atrophy | Calcified granulomas caused by neurocysticercosis or tuberculosis occurs in the endemic part of the world |
| Mogensen et al[19] | All girls, mean age unavailable, presented for early puberty evaluation to endocrine clinic | Pontine and pineal tumor, and hypothalamic pilocytic astrocytoma | Hydrocephalus, cortical dysplasia, and chiari II malformation | A high frequency a pathological brain findings occurred in 6-8 yr old girls with precocious puberty |
| 2Perret et al[20] | Incidentally found mass lesions management in children mean age 7.6 yr in oncology | Low-grade glioma, craniopharyngioma, ependymoma, and CPP | Medulloblastoma and fibrillary astrocytoma | Dysembryoplastic neuroepithelial tumor and tectal glioma can be monitored conservatively |
| Jordan, et al[21] | Children mean age 9.2 yr with sickle cell disease in neurology research | Chiari I malformation with large spinal cord syrinx3 | Possible tectal glioma, Possible tumor vs dysplasia | Amongst 6.6% incidental findings identified, 0.6% children with sickle cell disease had potentially serious or urgent finding |
Morris et al[32] published a meta-analysis, which reviewed 16 studies of subjects within the age range of 1 to 97 years, all of whom had no neurological symptoms. All subjects had brain MRI performed for the purpose of research and for occupational or commercial screening. The authors reported 135 (0.70%) of 19559 subjects with a neoplastic incidental finding. No age specific prevalence of neoplastic lesion was available for children aged 1 to 9 years. After omitting 34 adults aged 90 to 99, only four 20 year age bands were left for analysis[32].
Serious lesions can be divided into two groups: (1) ones that are known to get worse, such as a tumor; and (2) those that have the potential for worsening over time, such as pituitary lesions, pineal cysts, or vascular malformations. Such lesions typically manifest with compressive symptoms localized to the adjacent neuroanatomical structure.
Incidental vascular malformations, although uncommon, are frequently asymptomatic, which can greatly complicate the clinical management. It should be noted that none of the prospective studies reported any malignant findings as incidental. Potchen et al[14], 2013 prospectively reported granulomas with gliosis as a serious lesion.
Not surprisingly, a significant number of brain tumors were reported from pediatric oncologic-setting, Perret et al[20], 2011. The incidental serious findings in this study included low-grade glioma, craniopharyngioma, ependymoma, choroid plexus papilloma, medulloblastoma, and dysembryoplastic neuroepithelial tumor.
The common clinical profile of intracranial incidental findings on pediatric brain MRI is shown in the Table 6.
| Clinical implication | |
| Discovery of the unexpected incidental findings | Revealing during investigation enhances the patients or parents anxiety. The evidence-based knowledge will provide an additional confidence for the practicing physicians |
| Type of the incidental findings | Varieties of white matter changes are reported. However, these usually do not initiate a neurologic consultation. Chiari type I malformation, arachnoid cyst, and pineal cyst, all continued to be a common source of concern for some physicians |
| Distribution of incidental findings | Attention to the distribution of findings is a useful tool in deciding the clinical importance of such findings. A midline lesion particularly in the posterior fossa and hippocampal location is likely to have a serious clinical implication |
| The clinical context in which MRI was performed | This is probably the single most important step in understating the clinical implication of incidental findings (Table 6). This is particularly important when the child was referred to neurology after revealing the incidental finding on brain MRI |
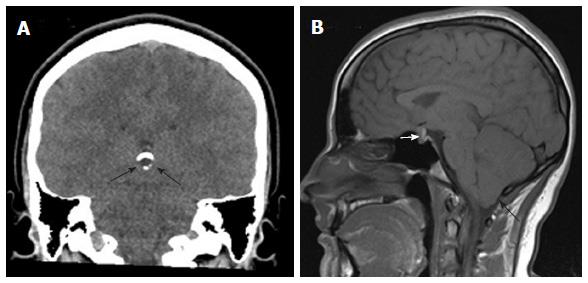
A 16-year-old girl presented with right facial nerve palsy. She had an unremarkable past medical history. A CT scan of the brain performed due to tingling feeling on the right side of her tongue revealed a partially calcified pineal cyst (Figure 2A). An MRI revealed an enhancing pituitary lesion measuring 13 mm × 10 mm × 10 mm, cerebellar ectopia (Figure 2B), and left maxillary sinusitis, which is not shown. She had no headaches, visual field defect, hearing difficulty or upper respiratory infection. The question is if her facial nerve palsy is related in any way to neuroimaging findings. The significance of more than one incidental finding is largely unknown.
More than one incidental finding is not uncommon. In the lack of any known implication some of these findings go unreported.
Four out of 18 (22%) studies listed in Table 1 reported more than one incidental finding. An average prevalence of more than one incidental finding in three studies (11, 13, and 17) was 3.8%. The forth study by Bayram et al[6], 2013 reported a very high prevalence (52%) of more than one white matter lesion in children with migraine. In fact the number of patients with more than one lesion exceeded the total number of the patients in this study. Authors’ indicated that these were migraine associated changes in the brain[33].
Incidentally discovered findings should always be considered in the context of the overall clinical impression. One should bear in mind the reason for performing the MRI of the brain. The answer to this question can often provide the direction for the next step of clinical management.
The MRI results are best managed at the time of planning for neuroimaging by considering the possibility of an incidental finding. Such preemptive action serves to alleviate parental concern, reduce additional medical care cost, and save physicians’ time[34]. After all, incidental findings are the most common insignificant abnormal findings revealed on pediatric brain MRI.
The parental perceived importance for MRI procedure is significantly higher than those of physicians. This disassociation of perception may lead to confrontation. This could be avoided by considering the parental concern. The physician’s explanation should be based upon the clinical context and what is known about the particular finding. It is only rarely that these findings perpetuate more concerns than the relief[35].
How did we manage the results of our case? The patient’s right facial nerve palsy has no neuroanatomical relation with pituitary lesion, cerebellar ectopia, pineal cyst, and the left maxillary sinusitis. Of note; sinusitis is the most common extracranial incidental finding on brain MRI. Our patient with facial nerve palsy was treated with a 5 d course of oral steroid. She was referred to an endocrinologist for further evaluation of the pituitary lesion.
An MRI revealing serious incidental findings requires close attention. These findings in a pediatric neurology practice remain low (0.3%-3.4%). Presently, there is no consensus regarding the optimal strategy on how to deal with these findings in practice or research[36].
In general, a midline located lesion with or without surrounding edema or contrast - enhancement needs to be further investigated. Depending upon the nature of the lesion or clinical impression, endocrinological, oncological, or neurosurgical evaluation should be considered.
Author (Gupta SN) preference is to first discuss with the interpreting radiologist and have a plan before delivery of the results to the parents. The necessity and results of such a discussion may vary depending upon the expertise of the clinician or radiologist. To characterize such a lesion systemically, the neuroradiologic differential diagnosis based on the MRI characteristics should be discussed. The presence or absence of perfusion-and diffusion-weighted MRI revealing changes in the diffusion coefficient should be documented[37]. With the use of intravenous contrast, the status of a blood-brain barrier should be evaluated. In case of non-enhancing lesions such as benign tumors, magnetic resonance spectroscopy[38] or diffuse tensor imaging may be additional use.
At times an equivocal finding may be perplexing in regards of the management strategy. In such a situation the patient should be followed clinically. Unless neurosurgical intervention is thought to be a realistic probability, the patient with incidental findings of this nature should not receive neurosurgical referral. This will prevent escalating parental anxiety.
The majority of children with intracranial incidental findings do not require clinical or neuroimaging follow-up. Scheduling further appointments merely for incidentally found findings or neuroimaging is likely to increase parental anxiety. Some parents may seek another neurologic consultation. Pituitary lesions, vascular malformations, or tumors have a true future clinical[39,40] or medico-legal implications. Fortunately, serious lesions in children remain extremely low as compared with adults or the elderly[41]. Occasionally, they require emergent medical attention and/or subsequent neurosurgical intervention.
A very limited number of incidentally found serious lesions include various tumors, which neurosurgical intervention. Non-tumor serious lesions includes Chiari I malformations, syrinx of the cervical spinal cord, and Rathke’s cleft cysts. Incidentally discovered lesions requiring neurosurgical interventions and their outcomes are shown in Table 7.
| Ref. | Incidentally found serious findings | No. ofpatients | Surgical procedure performed | Outcome |
| Schwedt et al[8] | Chiari type I malformation | 3 | Surgical decompression | Headache relieved in 2 patients after surgery |
| Jordan et al[21] | Chiari I malformation with spinal cord syrinx | 2 | Surgical decompression | Neurologic stable |
| Perret et al[20] | Pilocystic astrocytoma | 2 | Primary subtotal resection | Stable disease |
| Craniopharyngioma | 1 | Primary total resection | Complete remission | |
| Anaplastic ependymoma | 1 | Primary total resection, radio-chemotherapy | Complete remission | |
| Choroid plexus papilloma | 1 | Primary total resection | Complete remission | |
| Medulloblastoma | 1 | Delayed subtotal resection, radio-chemotherapy | Neurologic stable | |
| Fibrillary astrocytoma | 1 | Delayed total resection | Complete remission | |
| Mature teratoma | 1 | Delayed subtotal resection | Neurologic stable | |
| Desmoplastic ganglioglioma | 1 | Primary total resection | Complete remission | |
| Mogensen et al[19] | Pilocytic astrocytoma | 1 | Hypophysectomy | Patients developed pan hypopituitarism after surgery |
| Yilmaz et al[5] | Medulloblastoma | 1 | Urgent surgery for space occupying lesion | Headache relieved after surgery |
Perret et al[20], 2011, studied 335 children age < 18 years in an oncologic-setting. They reported 19 patients (5.67%) with an incidentally discovered primary brain tumor. Seven patients (2%) underwent immediate surgery; four patients had a low-grade glioma. Craniopharyngioma, ependymoma, and choroid plexus papilloma occurred one in each individual patient. The rest of the 12 (3.5%) children were treated conservatively. Of these 12 conservatively followed, 10 patients (83%) remained stable. The other 2 (17%) underwent surgery because of medulloblastoma and fibrillary astrocytoma progression. The authors of the study concluded that a subgroup of lesions such as tectal glioma and dysembryoplastic neuroepithelial tumor can be monitored conservatively.
Bredlau et al[42] reviewed the clinical course of 244 children over a 10 year period. The study reported 21 (8.6%) incidental brain lesions on MRI. Twelve (4.9%) patients underwent surgical resection of their lesions. Nine out of 10 patients (90%) had a posterior fossa lesion, and three out of 11 (27%) had supratentorial lesions. Authors of the study concluded that incidentally detected serious CNS lesions are small. The outcome for children with such lesions is excellent. They recommended close monitoring with serial MRIs as a safe alternative to immediate biopsy and/or resection for select patients[42]. Of note; the data from adult patients demonstrate that most Rathke’s cleft cysts the response to surgery tends to vary based on the endocrinopathology[43].
Dissatisfaction is an inciting event of litigation in the medical setting. Unlike research or healthy volunteer subjects, no consensus exists on how to handle incidental findings in clinical practice[44,45].
Claims of inappropriate management, ignorance, or discovery of a serious incidental finding on a later date, all have the potential to result in litigation. The discovery of incidental findings on brain MRI have led to its familiarity and a burden to clinical practice. Clinicians have an obligation of addressing the incidental finding revealed on MRI during the course of clinical evaluation. It is best prevented by pursuing before the availability of actual reports of MRI.
Based on the individual radiologist’s perception, the reports of incidental findings on MRI are variable. Hence, many incidental findings might, therefore, remain unreported. Rarely, inconsistencies in reporting may be a cause for litigation.
Neuroimaging with diffuse tensor imaging is likely to unfold the nature of the incidental findings particularly white matter changes. In the future, they are likely to be identified with the use of a high resolution MRI sequences. Use of a standardized scoring system by radiologists will eliminate the individual variability in reporting. This will also be useful in expanding our understating of the incidental findings.
Future review should address the reason for variable prevalence and answer the question if the pattern of incidental finding relates to a specific condition such as headache, seizure, development delay, or any other neurologic condition. Most importantly, this investigation should be addressed by an adequately powered statistical analysis of retrospective or prospective studies in homogeneous populations.
The detection of intracranial incidental findings on pediatric brain MRI is of immense importance to daily radiological or clinical practice. The Radiologist should report each and every incidentally discovered finding. Individual variability in reporting of brain MRI findings can be minimized by using unified terminology, describing radiologic characteristics, and by developing a standard radiologic classification system. Because significance of these findings remains unclear, it is important to report them as they are observed, rather than a subjective description.
Intracranial incidental findings are common in both healthy children and children presenting for neurologic evaluation. Prevalence increases with disorders affecting the brain.
Whether or not a reported “incidental finding” should be assigned as clinically significant, is the clinician’s prerogative. In uncertainty, the clinical context and course of the problem in question should take precedence. The spectrum of intracranial incidental findings on pediatric brain MRI presented in this review should be the basis for an evidence-based discussion. In addition, the proposed common profile will aid the clinical management of incidentally discovered findings. Most importantly, the management of an incidentally found serious lesion demands constant surveillance in clinical practice.
The author (Gupta SN) thanks Emeritus Professor Dr. Leonard J Graziani, MD, for his guidance and support.
Manuscript source: Invited manuscript
Specialty type: Pediatrics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Classen CF, Sangkhathat S S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Sebastian S, Araujo C, Neitlich JD, Berland LL. Managing incidental findings on abdominal and pelvic CT and MRI, Part 4: white paper of the ACR Incidental Findings Committee II on gallbladder and biliary findings. J Am Coll Radiol. 2013;10:953-956. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Saxena A, Luhadiya A, Ewen B, Goumas C. Magnetic resonance imaging and incidental findings of lateral ankle pathologic features with asymptomatic ankles. J Foot Ankle Surg. 2011;50:413-415. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Katzman GL, Dagher AP, Patronas NJ. Incidental findings on brain magnetic resonance imaging from 1000 asymptomatic volunteers. JAMA. 1999;282:36-39. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Weber F, Knopf H. Incidental findings in magnetic resonance imaging of the brains of healthy young men. J Neurol Sci. 2006;240:81-84. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Yılmaz Ü, Çeleğen M, Yılmaz TS, Gürçınar M, Ünalp A. Childhood headaches and brain magnetic resonance imaging findings. Eur J Paediatr Neurol. 2014;18:163-170. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Bayram E, Topcu Y, Karaoglu P, Yis U, Cakmakci Guleryuz H, Kurul SH. Incidental white matter lesions in children presentıng with headache. Headache. 2013;53:970-976. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Graf WD, Kayyali HR, Abdelmoity AT, Womelduff GL, Williams AR, Morriss MC. Incidental neuroimaging findings in nonacute headache. J Child Neurol. 2010;25:1182-1187. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Schwedt TJ, Guo Y, Rothner AD. “Benign” imaging abnormalities in children and adolescents with headache. Headache. 2006;46:387-398. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Koirala K. Magnetic resonance neuroimaging in patient with complain of seizure. J Nepal Health Res Counc. 2011;9:56-60. [PubMed] [Cited in This Article: ] |
| 10. | Kalnin AJ, Fastenau PS, deGrauw TJ, Musick BS, Perkins SM, Johnson CS, Mathews VP, Egelhoff JC, Dunn DW, Austin JK. Magnetic resonance imaging findings in children with a first recognized seizure. Pediatr Neurol. 2008;39:404-414. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Gupta S, Kanamalla U, Gupta V. Are incidental findings on brain magnetic resonance images in children merely incidental? J Child Neurol. 2010;25:1511-1516. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Seki A, Uchiyama H, Fukushi T, Sakura O, Tatsuya K. Incidental findings of brain magnetic resonance imaging study in a pediatric cohort in Japan and recommendation for a model management protocol. J Epidemiol. 2010;20 Suppl 2:S498-S504. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Gupta SN, Belay B. Intracranial incidental findings on brain MR images in a pediatric neurology practice: a retrospective study. J Neurol Sci. 2008;264:34-37. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Potchen MJ, Kampondeni SD, Mallewa M, Taylor TE, Birbeck GL. Brain imaging in normal kids: a community-based MRI study in Malawian children. Trop Med Int Health. 2013;18:398-402. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Kim BS, Illes J, Kaplan RT, Reiss A, Atlas SW. Incidental findings on pediatric MR images of the brain. AJNR Am J Neuroradiol. 2002;23:1674-1677. [PubMed] [Cited in This Article: ] |
| 16. | Oh YJ, Park HK, Yang S, Song JH, Hwang IT. Clinical and radiological findings of incidental Rathke’s cleft cysts in children and adolescents. Ann Pediatr Endocrinol Metab. 2014;19:20-26. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Rachmiel M, Blaser S, Widjaja E, Rovet J. Children with congenital hypothyroidism have similar neuroradiological abnormal findings as healthy ones. ScientificWorldJournal. 2013;2013:194918. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Whitehead MT, Oh CC, Choudhri AF. Incidental pineal cysts in children who undergo 3-T MRI. Pediatr Radiol. 2013;43:1577-1583. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Mogensen SS, Aksglaede L, Mouritsen A, Sørensen K, Main KM, Gideon P, Juul A. Pathological and incidental findings on brain MRI in a single-center study of 229 consecutive girls with early or precocious puberty. PLoS One. 2012;7:e29829. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Perret C, Boltshauser E, Scheer I, Kellenberger CJ, Grotzer MA. Incidental findings of mass lesions on neuroimages in children. Neurosurg Focus. 2011;31:E20. [PubMed] [DOI] [Cited in This Article: ] |
| 21. | Jordan LC, McKinstry RC, Kraut MA, Ball WS, Vendt BA, Casella JF, DeBaun MR, Strouse JJ. Incidental findings on brain magnetic resonance imaging of children with sickle cell disease. Pediatrics. 2010;126:53-61. [PubMed] [DOI] [Cited in This Article: ] |
| 22. | Itoh T, Magnaldi S, White RM, Denckla MB, Hofman K, Naidu S, Bryan RN. Neurofibromatosis type 1: the evolution of deep gray and white matter MR abnormalities. AJNR Am J Neuroradiol. 1994;15:1513-1519. [PubMed] [Cited in This Article: ] |
| 23. | Bryan RN, Manolio TA, Schertz LD, Jungreis C, Poirier VC, Elster AD, Kronmal RA. A method for using MR to evaluate the effects of cardiovascular disease on the brain: the cardiovascular health study. AJNR Am J Neuroradiol. 1994;15:1625-1633. [PubMed] [Cited in This Article: ] |
| 24. | Sawamura Y, Ikeda J, Ozawa M, Minoshima Y, Saito H, Abe H. Magnetic resonance images reveal a high incidence of asymptomatic pineal cysts in young women. Neurosurgery. 1995;37:11-15; discussion 15-16. [PubMed] [DOI] [Cited in This Article: ] |
| 25. | Peres MF, Zukerman E, Porto PP, Brandt RA. Headaches and pineal cyst: a (more than) coincidental relationship? Headache. 2004;44:929-930. [PubMed] [DOI] [Cited in This Article: ] |
| 26. | Mandera M, Marcol W, Bierzyńska-Macyszyn G, Kluczewska E. Pineal cysts in childhood. Childs Nerv Syst. 2003;19:750-755. [PubMed] [DOI] [Cited in This Article: ] |
| 27. | Zuketto C, van Gijn J. [Severe reversible dysphagia caused by herniation of the cerebellar ectopia]. Ned Tijdschr Geneeskd. 2002;146:771-773. [PubMed] [Cited in This Article: ] |
| 28. | Gosalakkal JA. Intracranial arachnoid cysts in children: a review of pathogenesis, clinical features, and management. Pediatr Neurol. 2002;26:93-98. [PubMed] [DOI] [Cited in This Article: ] |
| 29. | Chokshi FH, Poretti A, Meoded A, Huisman TA. Normal and abnormal development of the cerebellum and brainstem as depicted by diffusion tensor imaging. Semin Ultrasound CT MR. 2011;32:539-554. [PubMed] [DOI] [Cited in This Article: ] |
| 30. | Graf WD, Kayyali HR, Alexander JJ, Simon SD, Morriss MC. Neuroimaging-use trends in nonacute pediatric headache before and after clinical practice parameters. Pediatrics. 2008;122:e1001-e1005. [PubMed] [DOI] [Cited in This Article: ] |
| 31. | Chuang NA, Otsubo H, Chuang SH. Magnetic resonance imaging in pediatric epilepsy. Top Magn Reson Imaging. 2002;13:39-60. [PubMed] [DOI] [Cited in This Article: ] |
| 32. | Morris Z, Whiteley WN, Longstreth WT, Weber F, Lee YC, Tsushima Y, Alphs H, Ladd SC, Warlow C, Wardlaw JM. Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2009;339:b3016. [PubMed] [DOI] [Cited in This Article: ] |
| 33. | De Benedittis G, Lorenzetti A, Sina C, Bernasconi V. Magnetic resonance imaging in migraine and tension-type headache. Headache. 1995;35:264-268. [PubMed] [DOI] [Cited in This Article: ] |
| 34. | Grossman RI, Bernat JL. Incidental research imaging findings: Pandora’s costly box. Neurology. 2004;62:849-850. [PubMed] [DOI] [Cited in This Article: ] |
| 35. | Mold JW, Stein HF. The cascade effect in the clinical care of patients. N Engl J Med. 1986;314:512-514. [PubMed] [DOI] [Cited in This Article: ] |
| 36. | Borra RJ, Sorensen AG. Incidental findings in brain MRI research: what do we owe our subjects? J Am Coll Radiol. 2011;8:848-852. [PubMed] [DOI] [Cited in This Article: ] |
| 37. | Gajewicz W, Papierz W, Szymczak W, Goraj B. The use of proton MRS in the differential diagnosis of brain tumors and tumor-like processes. Med Sci Monit. 2003;9:MT97-M105. [PubMed] [Cited in This Article: ] |
| 38. | Ambrosetto P, Bacci A. In re: Basilar artery migraine and reversible imaging abnormalities. AJNR Am J Neuroradiol. 2000;21:234-235. [PubMed] [Cited in This Article: ] |
| 39. | Arnett BC. Tonsillar ectopia and headaches. Neurol Clin. 2004;22:229-236. [PubMed] [DOI] [Cited in This Article: ] |
| 40. | Bertrand RA, Martinez SN, Robert F. Vestibular manifestations of cerebellar ectopia. (Sub-group of Chiari I). Adv Otorhinolaryngol. 1973;19:355-366. [PubMed] [DOI] [Cited in This Article: ] |
| 41. | Yue NC, Longstreth WT, Elster AD, Jungreis CA, O’Leary DH, Poirier VC. Clinically serious abnormalities found incidentally at MR imaging of the brain: data from the Cardiovascular Health Study. Radiology. 1997;202:41-46. [PubMed] [DOI] [Cited in This Article: ] |
| 42. | Bredlau AL, Constine LS, Silberstein HJ, Milano MT, Korones DN. Incidental brain lesions in children: to treat or not to treat? J Neurooncol. 2012;106:589-594. [PubMed] [DOI] [Cited in This Article: ] |
| 43. | Kim JE, Kim JH, Kim OL, Paek SH, Kim DG, Chi JG, Jung HW. Surgical treatment of symptomatic Rathke cleft cysts: clinical features and results with special attention to recurrence. J Neurosurg. 2004;100:33-40. [PubMed] [DOI] [Cited in This Article: ] |
| 44. | Wolf SM, Lawrenz FP, Nelson CA, Kahn JP, Cho MK, Clayton EW, Fletcher JG, Georgieff MK, Hammerschmidt D, Hudson K. Managing incidental findings in human subjects research: analysis and recommendations. J Law Med Ethics. 2008;36:219-248, 211. [PubMed] [DOI] [Cited in This Article: ] |
| 45. | Booth TC, Jackson A, Wardlaw JM, Taylor SA, Waldman AD. Incidental findings found in “healthy” volunteers during imaging performed for research: current legal and ethical implications. Br J Radiol. 2010;83:456-465. [PubMed] [DOI] [Cited in This Article: ] |