Published online May 8, 2015. doi: 10.5409/wjcp.v4.i2.30
Peer-review started: November 26, 2014
First decision: January 8, 2015
Revised: January 27, 2015
Accepted: March 30, 2015
Article in press: April 2, 2015
Published online: May 8, 2015
Processing time: 173 Days and 12.9 Hours
We are reporting 3 cases of pediatric endobronchial tumors presented with recurrent pneumonia. The median age of patients, at time of presentation, was 10.6 years. All patients presented with recurrent pneumonia with a mean time to occurrence, after onset of symptoms, of 14 mo. Bronchoscopy was early performed as part of diagnostic work-up and it revealed an endobronchial mass in every case. Complete surgical resection was performed in all cases, with lung preservation in two of them. Neither post-operative chemotherapy nor radiotherapy was required. The mean duration of follow-up was 7 years and all patients are still alive and disease-free. Recurrent pneumonia, in pediatrics, should raise the suspicion of an obstructing lesion, congenital malformation or systemic disease. A systematic approach is useful for organize the clinicians initial workup. Prompt diagnosis allows parenchymal-sparing surgery, which offers the best chance of cure and reduces clinical and functional complications in these patients.
Core tip: The role of a systematic diagnostic work up in determining the risk of rare conditions in pediatric recurrent pneumonia has been delineated. This case series not only present 3 cases of rare pediatric endobronchial tumors, but also applies early bronchoscopy as a tool to rule out the presence of tumors of the respiratory tree in case of recurrent pneumonia. Prompt diagnosis allows parenchymal-preserving surgery, which offer the best chance of cure and reduce clinical and functional complications in these patients.
- Citation: Madafferi S, Catania VD, Accinni A, Boldrini R, Inserra A. Endobronchial tumor in children: Unusual finding in recurrent pneumonia, report of three cases. World J Clin Pediatr 2015; 4(2): 30-34
- URL: https://www.wjgnet.com/2219-2808/full/v4/i2/30.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v4.i2.30
Bronchial adenomas account for 5% of all primary pulmonary neoplasms in children and include both carcinoid and mucoepidermoid tumors[1-4]. These are considered as low-grade and slow growing malignant neoplasm and their evolutions are usually favorable after surgery[1,5,6]. Pathologic findings of endobronchial tumors can represent a wide array of symptoms as atelectasis or recurrent pneumonia, as the consequence of bronchial obstruction[3,5,7,8]. We describe 3 pediatric cases of endobronchial adenomas, occurring over a 10-year period at our hospital. All patients had history of recurrent pneumonia meaning more than 1 episode of pneumonia in 1 year or more than 3 episodes in a lifetime. We discuss their diagnostic work-up and clinical outcome. We suggest, for patients with recurrent pneumonia, early referral for bronchoscopic evaluation for accurate differential diagnosis. A delay in diagnosis of endobronchial tumor may lead to local and distant spread and permanent lung damage as consequence of radical surgery.
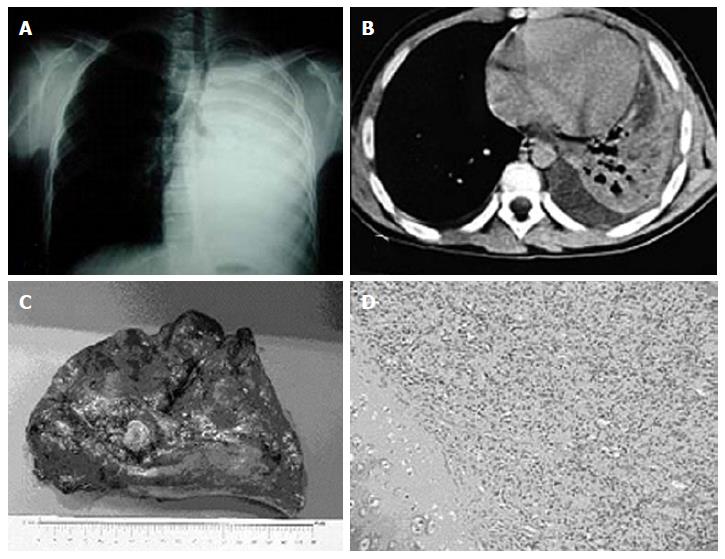
A 14-year-old boy presented with a history of recurrent bronchopneumonia, 5 episodes in the last 18 mo, unresponsive to antibiotic therapy. On clinical examination, he showed no breathing sounds on left hemithorax with thump bluntness. A chest X-ray showed a collapsed left lung with tracheal deviation (Figure 1A). A computer tomography (CT) scan showed a left endobronchial mass arising from the main bronchus with omolateral collapse of the lung and consensual pleural effusion (Figure 1B). Bronchoscopy revealed a polypoid, obstructive mass in the left main bronchus. The biopsy yielded positive result for typical endobronchial carcinoid. At surgery, a wide and infiltrating polypoid mass on main left bronchus was found so left pneumonectomy was performed (Figure 1C). The final histologic examination showed a 1.5-cm polypoid mass that was made up of monomorphic cellular proliferation with a low mitotic proliferative rate. Immunohistochemistry was strongly positive for chromogranin and weak for synaptophysin (Figure 1D). The adjacent pulmonary parenchyma was suggestive of consensual pneumonia. Octeotride scintigraphy showed a physiological tracer without metastasis. At 10 years follow up the patient had neither clinical nor radiological evidence of recurrence of the tumor.
A 10-year-old girl was admitted for evaluation and treatment of 1-year history of left pneumonia with 3 consecutive episodes. On examination she was afebrile, dullness to percussion and decreased breath sounds over the left upper lobe of the left lung. A chest X-ray showed a left pulmonary collapse with pleural effusion and an image suspected of left bronchial obstruction. CT scan demonstrated solid and lobulated mass with calcification and atelectasis in the posterior segment of the left upper lobe. Bronchoscopy revealed a polypoid tumor in the left main bronchus. Biopsy resulted in low-grade mucoepidermoid carcinoma. A left superior sleeve lobectomy, with end-to-end anastomosis between the main and inferior lobar bronchus, was performed. The post-operative course was uneventful. Follow up at 7 years was good and spirometric assessments showed forced expiratory volume in 1 s and forced vital capacity within normal range.
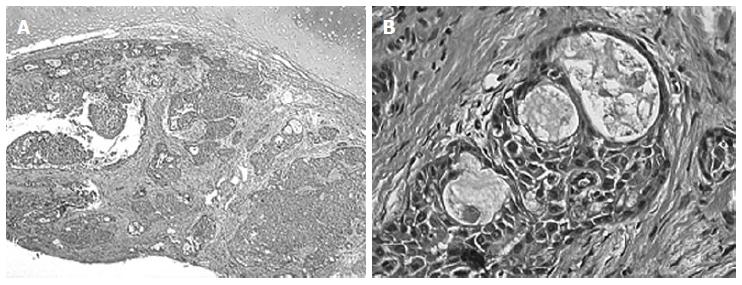
An 8-year-old boy presented with a 1-year history of bronchospasm and recurrent pneumonia, 4 episodes, unresponsive to corticosteroids, bronchodilators and antibiotic therapy. He was afebrile and his chest examination was unremarkable. Chest X-ray and CT revealed left bronchiectasis and left upper lobe consolidation as for pneumonia. Bronchoscopy revealed a polypoid mass arising from the left main bronchus. Histologic examination showed low-grade mucoepidermoid carcinoma (Figure 2). A left bronchial resection, with end-to-end anastomosis of the left main bronchus, was performed. Post-operative course was uneventful. The patient has remained disease-free at 5-year clinical and radiological follow-up.
Recurrent pneumonia is defined as more than 1 episode of pneumonia in 1 year or more than 3 episodes in a lifetime, with radiographically documented clearing episodes[4,7,9]. The number of host defects that can predispose to recurrent pneumonia is high, and differential diagnosis is often challenging. The first step is to confirm the diagnosis of recurrent pneumonia; it should be made by chest X-ray (2 projections) that reveals pulmonary consolidation on more than one occasion[7]. The presence of a persistent infiltrate in the same area, in the interval between pneumonias, could represent treatment failure or localized obstruction[7]. In these cases both CT scan and fiber optic bronchoscopy should be performed to make differential diagnosis between congenital lung defects (congenital adenomatoid cystic malformation, pulmonary sequestration, congenital emphysema), external compression of conducting airways, intraluminal foreign bodies or endobronchial masses[3,4,7,9,10]. Primary endobronchial tumors are rarely considered as predisposing factors for recurrent atelectasis or respiratory tract infection[2,3]. The symptoms are related to airway obstruction and include: recurrent pneumonia, persistent cough, sometimes associated with hemoptysis, wheezing and chest pain[1,11]. The lack of specificity of these symptoms may account for a median diagnostic delay of 5.85 ± 5 mo[5]. We describe 3 cases of recurrent pneumonia with mean time to presentation after onset of symptoms of 14 mo. In childhood, the most common primary lung tumors are malignant, with only approximately one-third benign[4]. The rarity of primary lung tumors is emphasized by the findings of an extensive review of the literature, in which the ratio of primary tumors to metastatic tumors to non-neoplastic lesion of the lung is 1:5:60[3,4]. Endobronchial tumors include benign lesions such as hemangiomas, papillomas, inflammatory pseudotumors (plasma cell granulomas), leiomyomas and mucus gland tumors. The malignant ones include: bronchial adenomas (an obvious misnomer), carcinoids, mucoepidermoid carcinomas, and adenoid cystic carcinoma[3,4].
Bronchial carcinoid is the most common primary endobronchial neoplasm; it makes up about 80% of malignant pulmonary neoplasm in children[3,8]. The tumor arises from the Kulchitsky cell of the respiratory epithelium. Carcinoid tumors can be divided in typical and atypical forms with the latter exhibiting histologically malignant features and aggressive clinical behavior. This histological and clinical distinction is not clear in pediatric population due to the rarity of this pathology[3]. Our case although showed typical histology with benign behavior. In the literature, the median age at diagnosis in children in 10.5 ± 3 years, but we described the case of a patient who came to our attention at 14 years of age[5]. This neoplasm can arise in the lobar bronchi (75%), in the mainstream bronchi (10%), causing atelectasis, or in lung periphery (15%), and the right lung is more often involved then the left one[8,11,12]. These tumors are described as endobronchial polypoid masses with intraluminal, mural and extra bronchial components, which could completely obstruct the bronchus and interfere with distal ventilations giving reason of respiratory symptoms as dyspnea and wheezing or further complications as pneumonia and atelectasis[5,8]. Rarely, patients with tracheobronchial carcinoid tumors present with carcinoid syndrome, such as: Cushing’s syndrome, acromegaly, or the inappropriate antidiuretic hormone secretion[12]. Distant metastasis or local recurrences are rarely reported, especially in cases with atypical histology. As in our cases, the chest X-ray may show findings of partial or total bronchial obstruction as atelectasis, although it is reported as normal in about 10% of patients[8,11]. CT scan is the most sensitive noninvasive imaging method for bronchial abnormalities. It allows the best resolutions of a pulmonary mass, defining: the relationship with the tracheobronchial tree, the presence of calcification, reported in 4%-26% of the cases, concomitant lymphadenopathies, and the grade of contrast enhancement[8,11]. However, bronchoscopy is considered as the gold standard for diagnosis and, despite the risk of hemorrhage, endobronchial biopsy has been shown to give the highest yield of positive diagnosis[5]. Sleeve or bronchoplastic resections are preferred to more extensive resection of centrally located carcinoids, even if atypical carcinoid requires a more extensive resection with lymph node dissection[3,8,13]. Our patient underwent pneumonectomy due to the extensive infiltration of the lesion as consequence of late in diagnosis. Techniques for bronchoscopic resection include eletrocautery, NdYAG laser and piecemeal removal with biopsy forceps, but they are considered inadequate and may lead to tumor recurrence[14]. The recurrence rate is estimated at 8.2%, with overall survival of 92% at 10 years[13]. Systematic monitoring after the surgical intervention is recommended with clinical examination and chest X-ray. We followed up our patients for 10 years without evidence of recurrence. Early bronchoscopy should be performed if clinical symptoms, as recurrent pneumonia, and radiological findings are suggestive of tumor recurrence.
Bronchial mucoepidermoid carcinoma is a slow-growing, malignant glandular epithelial neoplasm that origins from excretory duct reserve cells of serous and mucous glands. It, particularly, involve the respiratory mucosa[1,15]. These tumors are rare in children, accounting for 2.5% to 7.3% of endobronchial adenomas and representing 0.1% to 0.2% of primary lung cancers[1,3,16]. Although the age range of patients is extensive, cases involving patients < 10 years old are rarely observed[2]. Our patients had respectively 10 and 8 years of age. The clinical symptoms are mainly related to airway obstruction and include pneumonia or recurrent pneumonias up to 48%[2,11]. Both our patients presented with a clinical history of recurrent pneumonia, respectively 3 and 4 episodes. Common radiological findings, on CT scan, are bronchial nodular mass with or without post-obstructive pneumonia, atelectasis, or a solitary nodule and lymphadenopathies should be always checked[8,15]. Treatment consists of a careful surgical removal of the tumor, the lymphnodes and vascular and perineural infiltration should be evaluated. When technically feasible, a sleeve resection of the involved bronchus is recommended[5]. The prognosis is good in up of 95% of the cases and low and intermediate grade carcinomas, with complete resection, do not require chemotherapy or radiotherapy[1,12]. In the present study lobectomy was performed in one-case and sleeve resections in other one; thus allowed a considerable portion of the lung parenchyma to be preserved. The risk of recurrence justifies a long-term clinical follow-up, indeed bronchoscopy should be performed only in case of severe respiratory symptoms[5]. Our patients had no clinical or radiological evidence of disease recurrence during a 10 and 5 years follow-up period.
Endobronchial tumors are rare in the pediatric population; these tumors most often present with symptoms of recurrent pneumonia or wheezing. In case of respiratory symptoms that do not improve with standard treatment (antibiotics, bronchodilators), further work up with CT scan and bronchoscopy is advisable to rule out the presence of an obstructive process as endobronchial tumors. Early diagnosis may help in determining optimal treatment plan that can increase the possibility of implementing a selective procedure, avoiding the pulmonary functional impairment and chest wall deformity that can result from extensive lung resection and improve outcome.
A series of 3 pediatric patients with a median age at presentation of 10.6 years, all presented with recurrent pneumonia, non-responsive to medical standard therapy.
Case 1: No breathing sounds with thump bluntness and dullness to percussion on left hemithorax; Case 2: Dullness to percussion and decreased breath sounds over the left upper lobe of the left lung; Case 3: No pathological findings on thoracic objective examination.
Cystic congenital adenomatoid malformation, congenital emphysema, lung mass, lung abscess, pneumonia.
Blood count cell and metabolic panel tests shows, only, elevated white cells blood count.
Case 1: An endobronchial mass arising from the left main bronchus with omolateral collapse of the lung and consensual pleural effusion; Case 2: A solid and lobulated mass with internal calcification and atelectasis in the posterior segment of the left upper lobe; Case 3: Left bronchiectasis and left upper lobe consolidation.
Case 1: Bronchoscopy and biopsy revealed typical endobronchial carcinoid; Case 2: Bronchoscopy and biopsy revealed low-grade mucoepidermoid carcinoma; Case 3: Bronchoscopy and biopsy revealed low-grade mucoepidermoid carcinoma.
Case 1: The patient was treated with a left pneumonectomy; Case 2: The patient was treated with a left superior sleeve lobectomy, with end-to-end anastomosis between the main and inferior lobar bronchus; Case 3: The patient was treated with a left bronchial resection, with end-to-end anastomosis of the left main bronchus.
Endobronchial tumors are rare in childhood and are not often considered in the differential diagnosis of recurrent pneumonia and bronchoscopy is not usually considered as first diagnostic approach.
Bronchial carcinoid is a tumor that arises from the Kulchitsky cell of the respiratory epithelium. It is divided in typical and atypical forms. Bronchial mucoepidermoid carcinoma is a slow-growing, malignant glandular epithelial neoplasm that origins from excretory duct reserve cells of serous and mucous glands, in particular that find within the submucosal of the respiratory mucosa
This case series not only represents 3 rare cases of pediatric endobronchial tumors, but also underline the need of systematic diagnostic work-up, which should consider bronchoscopy, to prevent delayed diagnosis of potential malignant lesions.
The authors have described three rare cases of pediatric endobronchial tumors that presented with recurrent pneumonia. The article highlights the need of systematic approach to recurrent pneumonia by clinicians to prevent complications due to rare conditions. Prompt diagnosis allows parenchymal-preserving surgery, which offer the best chance of cure and reduce clinical and functional complications in these patients.
P- Reviewer: Abdel-Aziz M, Aydogdu O S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Welsh JH, Maxson T, Jaksic T, Shahab I, Hicks J. Tracheobronchial mucoepidermoid carcinoma in childhood and adolescence: case report and review of the literature. Int J Pediatr Otorhinolaryngol. 1998;45:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Qian X, Sun Z, Pan W, Ye Q, Tang J, Cao Z. Childhood bronchial mucoepidermoid tumors: A case report and literature review. Oncol Lett. 2013;6:1409-1412. [PubMed] |
| 3. | Al-Qahtani AR, Di Lorenzo M, Yazbeck S. Endobronchial tumors in children: Institutional experience and literature review. J Pediatr Surg. 2003;38:733-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Cohen MC, Kaschula RO. Primary pulmonary tumors in childhood: a review of 31 years’ experience and the literature. Pediatr Pulmonol. 1992;14:222-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 91] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Fauroux B, Aynie V, Larroquet M, Boccon-Gibod L, Ducou le Pointe H, Tamalet A, Clément A. Carcinoid and mucoepidermoid bronchial tumours in children. Eur J Pediatr. 2005;164:748-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Roby BB, Drehner D, Sidman JD. Pediatric tracheal and endobronchial tumors: an institutional experience. Arch Otolaryngol Head Neck Surg. 2011;137:925-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Kaplan KA, Beierle EA, Faro A, Eskin TA, Flotte TR. Recurrent pneumonia in children: a case report and approach to diagnosis. Clin Pediatr (Phila). 2006;45:15-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Curtis JM, Lacey D, Smyth R, Carty H. Endobronchial tumours in childhood. Eur J Radiol. 1998;29:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Wald ER. Recurrent and nonresolving pneumonia in children. Semin Respir Infect. 1993;8:46-58. [PubMed] |
| 10. | Andersen JB, Mortensen J, Damgaard K, Skov M, Sparup J, Petersen BL, Rechnitzer C, Borgwardt L. Fourteen-year-old girl with endobronchial carcinoid tumour presenting with asthma and lobar emphysema. Clin Respir J. 2010;4:120-124. [PubMed] |
| 11. | Granata C, Battistini E, Toma P, Balducci T, Mattioli G, Fregonese B, Gambini C, Rossi GA. Mucoepidermoid carcinoma of the bronchus: a case report and review of the literature. Pediatr Pulmonol. 1997;23:226-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Dewan RK, Kesieme EB, Ramchandani R. Surgical treatment for tracheobronchial carcinoid tumors: a 16-year experience. Asian Cardiovasc Thorac Ann. 2012;20:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Gustafsson BI, Kidd M, Chan A, Malfertheiner MV, Modlin IM. Bronchopulmonary neuroendocrine tumors. Cancer. 2008;113:5-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 330] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 14. | Luckraz H, Amer K, Thomas L, Gibbs A, Butchart EG. Long-term outcome of bronchoscopically resected endobronchial typical carcinoid tumors. J Thorac Cardiovasc Surg. 2006;132:113-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Giusti RJ, Flores RM. Mucoepidermoid carcinoma of the bronchus presenting with a negative chest X-ray and normal pulmonary function in two teenagers: two case reports and review of the literature. Pediatr Pulmonol. 2004;37:81-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Tsuchiya H, Nagashima K, Ohashi S, Takase Y. Childhood bronchial mucoepidermoid tumors. J Pediatr Surg. 1997;32:106-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |