Published online Aug 10, 2015. doi: 10.5317/wjog.v4.i3.68
Peer-review started: April 4, 2015
First decision: May 13, 2015
Revised: May 30, 2015
Accepted: June 18, 2015
Article in press: June 19, 2015
Published online: August 10, 2015
Processing time: 140 Days and 12.3 Hours
Pubovaginal slings have become the gold standard to treat stress urinary incontinence. Traditionally, the sling referred to a suspensory that was placed under the urethra and brought through the retropubic space and anchored on either side of the midline. Since this original concept, there have been many materials used for the sling, and there have been many different anchoring approaches. Most agree that one of the best materials is polypropylene mesh. However, the means of anchoring the device and where best to have this anchorage placed is debatable. The options for anchoring simply include using darts vs not to hold the sling in place. The location of this anchorage, on the other hand, is much more controversial. The main locations are retropubic, transobturator, and via a single incision. The obturator and retropubic slings have become the standard of care over time. The single incision sling, on the other hand, is starting to be more acceptable which has resulted in it being used more frequently. The single incision relies on mainly anchoring the sling through the obturator internus muscle with possible inclusion of the obturator membrane. The purpose of this review article is to present the data that exists for the use of the single incision sling.
Core tip: Polypropylene slings have become the mainstay of therapy for treating stress urinary incontinence in women. Historically, these slings have worked well, but there was always the concern of morbidity. The goal of the single incision sling (SIS) is to provide high efficacy with minimal side effects. The initial use of the SIS was mottled by confusion with the techniques for deployment. The most recent data has shown that when the SIS is used appropriately the success rates are similar to standard mid-urethral slings with minimal risk of bladder, vascular, or nerve injury as well as chronic pain.
- Citation: Serels S. Single incision slings: Past, present, and future. World J Obstet Gynecol 2015; 4(3): 68-71
- URL: https://www.wjgnet.com/2218-6220/full/v4/i3/68.htm
- DOI: https://dx.doi.org/10.5317/wjog.v4.i3.68
Pubovaginal slings have been used for decades. However, it wasn’t until the mid to late 1990’s that the use expanded. This expansion was due in part to the use of polypropylene mesh. It was Ulmsten et al[1] who proved to the medical community that one could correct stress urinary incontinence (SUI) by using a piece of polypropylene mesh. Additionally, at the same time the synthetic sling became available, there was an enormous push by the device companies to educate the physicians. This education did not only include Urologists who were the main surgeon providing slings to their patients but it included gynecologists. This initially involved using transvaginal tape through the retropubic space. Although this worked well, there still was the potential for adverse events involving the bowel, bladder, and vascular structures[2,3]. Most of these complications were due to the use of trocars in the retropubic space. The transobturator sling was an evolutionary advancement, which attempted to preserve the high success rates of retropubic polypropylene slings while minimizing the chance of surgical complications. This sling in theory eliminated the chance of bowel injury and significantly reduced the chance of bladder injury. However, it still proved to possibly cause vascular injury to the obturator vessels or nerve injury to the obturator nerve. These patients were also at risk of groin pain either from muscular or tendon injury or perhaps neurologic irritation. Also, the medical community was looking for a sling that was the least invasive with high success rates and minimal chance of complications. In response to these desires, a polypropylene sling using a single vaginal incision was created.
The single incision sling (SIS) technique enables the user to place a piece of polypropylene mesh through a single vaginal incision. The idea of a SIS was first used approximately 7 years ago. The sling material varied in lengths from 8-9 cm. Some of these slings used fixation anchors while others relied more on scaring to provide fixation. Throughout the years, there were even variable length slings developed. The techniques for placement of many of the previous SISs were not consistently uniform. As a result, the early data for the SISs were not always comparable to those seen with transobturator and retropubic slings. However, the most recent retrospective and prospective studies on the use of second-generation SIS systems have demonstrated relatively high success rates with minimal morbidity. This review will provide evidence in support of the SIS.
To enhance the understanding of the SIS, it is important to understand how it is placed. The description below provides the generalized technique for the placement of the SIS.
Prior to the surgery, IV antibiotics are administered. The patient is then given either local, general, or regional anesthesia at the discretion of the surgeon in combination with the anesthesiologist. A dorsal lithotomy position is then achieved to facilitate surgery. A foley is inserted to empty the bladder. A 1-2 cm anterior vaginal wall incision is made at the level of the midurethra. The dissection is than carried out laterally to the level of the inferior pubic rami on either side using blunt and sharp dissection. This surgical preparation provides a pathway for the delivery of the sling arms. The polypropylene mesh tip is placed onto an introducer, which is inserted into the dissected pathway and used to pass the distal arm anchors through the obturator internus muscle behind the pubic ramus. The sling is advanced using the introducer until the midline of the sling reaches the patient’s midline under the urethra. This placement of the sling tip is repeated similarly on the opposite side. The polypropylene mesh sling is then brought to rest under the midurethra in a tensionless fashion. The anchors of the sling are resting in the obturator internus muscle. The goal of the surgeon is to visually see the periurethral tissue “pillowing” through the mesh material with a potential space existing between the sling and urethra such that a small instrument could easily be inserted. Cystoscopy is performed to ensure the bladder, urethra, and ureters are not compromised. The vaginal incision is then closed with a running absorbable suture.
There have been a tremendous number of articles written on the Single Incision technology. The early articles using SIS were mixed, and most early findings pertaining to their efficacy did not show equivalence to the results of the transobturator and retropubic slings[4]. Walsh[5] showed in 2011 that the use of the TVTsecur sling resulted in cure rates of 76% both subjectively and objectively. He described using both a “U” approach and a hammock approach. He concluded that more studies are needed before TVT secure could be routinely used. There were other slings such as the Ajust sling by C.R. Bard, Inc., New Providence, NJ United States, that conceptually made sense and, if used in the appropriate hands, yielded high success rates. In Jiang et al[6] paper, he showed that using the AJust sling resulted in subjective and objective sure rates of 82.3% and 91.2% in a 12-mo follow-up respectively. This was a single site study where there were no cases of bladder perforation or major bleeding. There were also no reported cases of groin pain at 6 and 12 mo[6].
This study exemplifies the importance of technique when placing the SISs. Although this group of researchers was able to achieve high success rates with this sling, the sling was not universally deployed successfully, and, as a result, this sling even with its high success rates is no longer being marketed by C.R. Bard Inc.
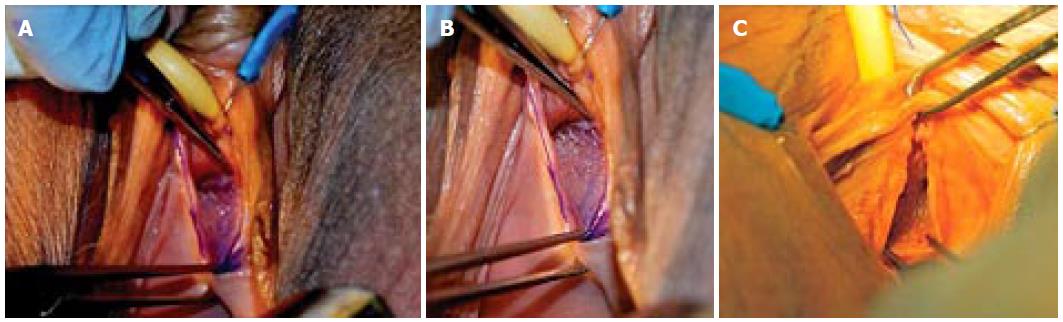
Initially, the SIS was thought to work differently than other slings and its placement and tensioning were not standardized. Surgeons were using it to go in the retropubic direction as well as the obturator location. It then became accepted by most that the placement was to be in the obturator internus muscle. The tension could be set in many different ways, but the end result would be a sling that was up against the urethra with the periurethral tissues “puckering or pillowing” through the mesh openings such that a potential space existed to insinuate a small medical instrument between the urethra and the sling (Figure 1).
In the article entitled “Cadaveric Assessment of Synthetic Mid-Urethral Sling Placement”, the placement of the SIS was compared to the obturator and retropubic sling[7]. It was determined that the SIS was similar to the others in appearance and furthermore was most likely at the midurethra and had the most correct tension. It is studies like this that show what is being done by the three sling approaches have different means of achieving the same endpoint.
There are presently around 26 randomized controlled trials, which are using 7 different types of SISs. In these studies approximately 3300 patients were evaluated[8].
Many of the studies have been performed comparing the SIS to the standard mid-urethral slings, which are considered to be either obturator slings or retropubic slings. The majority of these studies support the use of the SIS[9-25]. Lee et al[25] recently published a randomized trial comparing single incision vs outside-in transobturator mid-urethral sling. This paper studied the MiniArc SIS and showed an objective cure rate of 94.4% and a patient reported cure of 92.2% at 12 mo. The Monarc sling was the comparator to the MiniArc and it showed statistically similar results with a 96.7% objective sure and a 94.2% subjective cure. The operative time was reduced by 0.5 min in the SIS group. The Monarc group required more analgesia in the first 24 h and reported more short-term groin pain. The quality of life questionnaires and sexual function questionnaires revealed similar results in both groups. The patients undergoing repeat incontinence surgery were 2.7% in the MiniArc group compared to 1.8% in the Monarc group while 6.2% of the Monarc group had groin pain beyond 6 mo compared to 0% in the MiniArc group. For both patient groups, BMI and age were associated with higher failure rates[25].
Similar data was shown by Enzelsberger et al[26] who also looked at the MiniArc SIS and compared it to the Monarc. In this study, there was an objective cure rate of 82%. They also had shorter OR times and less groin pain. In our long-term study using the Solyx SIS, we also saw subjective success rates of 93% over a mean follow up of 43 mo[27]. There was, however, one recent article by Basu et al[28] that showed a lower success rate with the SIS than an obturator sling. This study also had a higher erosion rate with the SIS, which possibly implies a technical issue with using the single incision technology[28].
In the Mostafa et al[8] metaanalysis, he primarily looked at the MiniArc sling as compared to either retropubic or obturator slings. This study shows an aggregate objective cure rate of 88% with a subjective cure rate of 76% for the SISs. Additionally, the SIS had shorter operative times, lower incidence of groin pain, earlier return to work, and lower pain scores. There were no significant differences in subjective or objective cure rates for the SIS vs the standard mid-urethral slings. Also, the impact on quality of life and sexual function were similar. The TVT secur was not included in this analysis due to its poor early data and that it is now off the market as of 2012.
There are many SISs currently available. Each is different in its design and applicator as well as technique for placement. They all hope to provide the same endpoint, which is a backboard for the urethra to use with increases in abdominal pressure. Current data does suggest that if the SIS is used appropriately there would be an enhanced safety profile with less postoperative discomfort and high success rates. It is the responsibility of the medical community to provide guidelines for the use of these slings and to standardize their placement to assure reproducibility of the success rates. The correct use of SISs will ultimately lead to a treatment, which provides high success rates with low morbidity for our patients who suffer with SUI.
P- Reviewer: Cosmi E, Tsikouras P, Yokoyama Y S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Ulmsten U, Johnson P, Rezapour M. A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol. 1999;106:345-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 407] [Cited by in RCA: 353] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 2. | Boustead GB. The tension-free vaginal tape for treating female stress urinary incontinence. BJU Int. 2002;89:687-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Kuuva N, Nilsson CG. A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand. 2002;81:72-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 353] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 4. | Petros PE, Richardson PA. Midurethral Tissue Fixation System sling -- a ‘micromethod’ for cure of stress incontinence -- preliminary report. Aust N Z J Obstet Gynaecol. 2005;45:372-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Walsh CA. TVT-Secur mini-sling for stress urinary incontinence: a review of outcomes at 12 months. BJU Int. 2011;108:652-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Jiang T, Xia Z, Cheng D, Song Y, Guo Z, Hu Q, Zhao Y, Yin Y. Short-term outcomes of adjustable single-incision sling (Ajust™) procedure for stress urinary incontinence: a prospective single-center study. Eur J Obstet Gynecol Reprod Biol. 2015;186:59-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Serels S. Cadaveric Assessment of Synthetic Mid-Urethral Sling Placement. Open J Urol. 2011;1:19-24 Published Online May 2011. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Mostafa A, Lim CP, Hopper L, Madhuvrata P, Abdel-Fattah M. Single-incision mini-slings versus standard midurethral slings in surgical management of female stress urinary incontinence: an updated systematic review and meta-analysis of effectiveness and complications. Eur Urol. 2014;65:402-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 117] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 9. | Merali S, Dolhaniuk C, Unger T. Stress incontinence in women; a pilot study comparing the MiniArc single incision sling system to the Monarc transobturator sling system. J Minim Invasive Gynecol. 2012;19:S33-S34. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Schellart RP, Oude Rengerink K, Van der Aa F, Lucot JP, Kimpe B, de Ridder DJ, Dijkgraaf MG, Roovers JP. A randomized comparison of a single-incision midurethral sling and a transobturator midurethral sling in women with stress urinary incontinence: results of 12-mo follow-up. Eur Urol. 2014;66:1179-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Basu M, Duckett J. A randomised trial of a retropubic tension-free vaginal tape versus a mini-sling for stress incontinence. BJOG. 2010;117:730-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Oliveira R, Botelho F, Silva P, Resende A, Silva C, Dinis P, Cruz F. Exploratory study assessing efficacy and complications of TVT-O, TVT-Secur, and Mini-Arc: results at 12-month follow-up. Eur Urol. 2011;59:940-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Tutolo M, De Ridder D, Peeters E, Schillebeeckx C, Van Der Aa F. The impact of surgical volume on postoperative outcomes in patients treated with single incision sling: results from a tertiary referral center. Poster session presented at: ICS 2014, Rio de Janeiro; Oct 20-24 2014; . [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Kennelly MJ, Moore R, Nguyen JN, Lukban J, Siegel S. Miniarc single-incision sling for treatment of stress urinary incontinence: 2-year clinical outcomes. Int Urogynecol J. 2012;23:1285-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Madsen AM, El-Nashar SA, Woelk JL, Klingele CJ, Gebhart JB, Trabuco EC. A cohort study comparing a single-incision sling with a retropubic midurethral sling. Int Urogynecol J. 2014;25:351-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Martan A, Krhut J, Mašata J, Švabík K, Halaška M, Horčička L, Zachoval R. Prospective randomized study of MiniArc and Ajust single incision sling procedures [published online ahead of print October 27, 2013]. Low Urin Tract Symptoms. 2014;6:172-174. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Moore RD, De Ridder D, Kennelly MJ. Two-year evaluation of the MiniArc in obese versus non-obese patients for treatment of stress urinary incontinence. Int J Urol. 2013;20:434-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Presthus JB, Van Drie D, Graham C. MiniArc single-incision sling in the office setting. J Minim Invasive Gynecol. 2012;19:331-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Botros C, Lewis C, Culligan P, Salamon C. A prospective study of a single-incision sling at the time of robotic sacrocolpopexy. Int Urogynecol J. 2014;25:1541-1546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | De Ridder D, Berkers J, Deprest J, Verguts J, Ost D, Hamid D, Van der Aa F. Single incision mini-sling versus a transobutaror sling: a comparative study on MiniArc and Monarc slings. Int Urogynecol J. 2010;21:773-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Oliveira R, Silva A, Pinto R, Silva J, Silva C, Guimarães M, Dinis P, Cruz F. Short-term assessment of a tension-free vaginal tape for treating female stress urinary incontinence. BJU Int. 2009;104:225-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 22. | Pickens RB, Klein FA, Mobley JD, White WM. Single incision mid-urethral sling for treatment of female stress urinary incontinence. Urology. 2011;77:321-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Sun MJ, Sun R, Li YI. A comparative study of a single-incision sling and a transobturator sling: clinical efficacy and urodynamic changes. Int Urogynecol J. 2013;24:823-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Palomba S, Oppedisano R, Torella M, Falbo A, Maiorana A, Materazzo C, Tartaglia E, Tolino A, Mastrantonio P, Alio L. A randomized controlled trial comparing three vaginal kits of single-incision mini-slings for stress urinary incontinence: surgical data. Eur J Obstet Gynecol Reprod Biol. 2012;163:108-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Lee JK, Rosamilia A, Dwyer PL, Lim YN, Muller R. Randomized trial of a single incision versus an outside-in transobturator midurethral sling in women with stress urinary incontinence: 12 month results. Am J Obstet Gynecol. 2015;213:35.e1-35.e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Enzelsberger H, Cemer I, Enzelsberger S, Schalupny J. MiniArc versus Monarc - a prospective randomized study of the treatment of female stress urinary incontinence with a follow-up of 2 years. Obstet Gynecol. 2010;70:499-502. |
| 27. | Serels S, Duoso M. Long term follow up of the Solyx single-incision sling system in the treatment of female stress urinary incontinence. Open J Urol. 2014;4:13-17 Published Online February 2014. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Basu M, Duckett J. Three-year results from a randomised trial of a retropubic mid-urethral sling versus the Miniarc single incision sling for stress urinary incontinence. Int Urogynecol J. 2013;24:2059-2064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |