Published online Jan 20, 2023. doi: 10.5317/wjog.v12.i1.1
Peer-review started: June 24, 2022
First decision: September 5, 2022
Revised: September 15, 2022
Accepted: December 13, 2022
Article in press: December 13, 2022
Published online: January 20, 2023
Processing time: 223 Days and 21.4 Hours
Any non-cephalic presentation in a fetus is regarded as malpresentation. The most common malpresentation, breech, contributes to 3%-5% of term pregnancies and is a leading indication for cesarean delivery. Identification of risk factors and a proper physical examination are beneficial; however, ultrasound is the gold standard for the diagnosis of malpresentations. External cephalic version (ECV) refers to a procedure aimed to convert a non-cephalic presenting fetus to cephalic presentation. This procedure is performed manually through the mother’s abdomen by a trained health care provider, to reduce the likelihood of a cesarean section. Studies have reported a version success rate of above 50% by ECV. The main objective of this review is to present a broad perspective on fetal mal
Core Tip: Breech presentation is a leading indication for cesarean surgery. However, external cephalic version (ECV), with a success chance of above 50%, can be performed at 36 wk of gestation or at 39 wk of gestation in order to convert a non-cephalic presenting fetus to a cephalic presenting. A trial of labor or cesarean delivery can be planned after an unsuccessful ECV. Fetus breech can be delivered by vaginal breech delivery or cesarean delivery. The main objective of this review is to present a broad perspective on fetal malpresentation, ECV, and delivery of a breech fetus.
- Citation: Azimirad A. What to do when it is breech? A state-of-the-art review on management of breech presentation. World J Obstet Gynecol 2023; 12(1): 1-10
- URL: https://www.wjgnet.com/2218-6220/full/v12/i1/1.htm
- DOI: https://dx.doi.org/10.5317/wjog.v12.i1.1
The nearest anatomical part of the fetal body to the maternal pelvic inlet is defined as fetal presentation. The most desired presentation, with the lowest maternal and fetal risk, is the cephalic presentation[1,2].
Any non-cephalic presentation in a fetus is regarded as malpresentation. The most common mal
A literature search on the platforms Medline (via PubMed), Google Scholar, Scopus, and Web of Science, and Cochrane Database of Systematic Reviews was performed to find the published articles on the subject of this narrative review. The search time period was set to January 1995 to March 2022. The search terms are included in Table 1. The inclusion criteria included full texts, any article type, and English literature. This narrative review followed the steps proposed in SANRA tool-a scale for the quality assessment of narrative review articles[7].
| Search terms | ||
| Fetal malpresentation | External cephalic version | Fetal presentation, breech |
| Fetal presentation | Fetal version | Frank breech presentation |
| Presentation, fetal | Version, external cephalic | Incomplete breech |
| Version, fetal | Breech presentation | Labor presentation |
| Presentation, breech | Complete breech | Breech |
| Labor presentation | ||
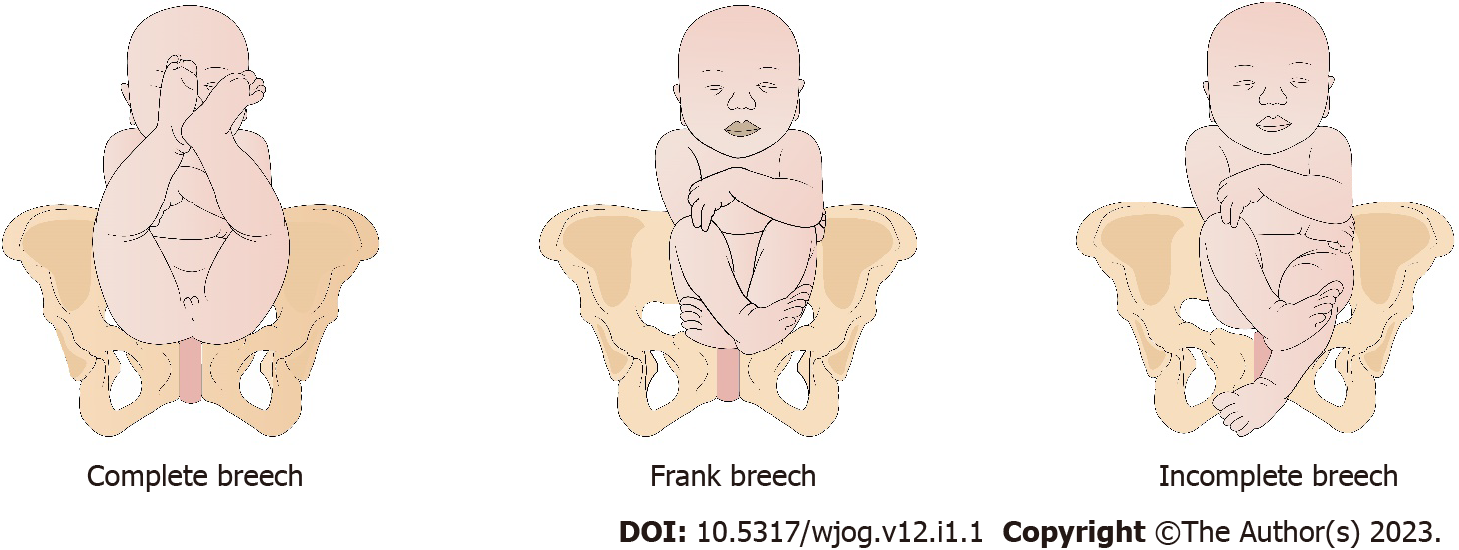
Breech is when the fetal buttocks or feet are the presenting parts. Breech can happen as frank (hips flexed, knees extended), complete (hips and knees flexed), and incomplete (not fully flexed hip; one-sided or both-sided). Most breech fetuses present as frank breech. Rarely, the foot advances into the birth canal, which is known as a footling breech presentation[4,6,8,9]. Please refer to Figure 1.
Breech complicates around 3%-5% of at-term pregnancies. However, earlier in pregnancy, as the fetus is floating in the intrauterine cavity, it is more common. The prevalence of breech at 28 and 32 wk of gestation decreases from 20%-25% to 8%-16%. Naturally, as pregnancy advances, the fetus tends to rotate inside the uterus to present with the head in the maternal pelvis. The reason for this is not clear; however, 3%-5% of term fetuses fail to do so[10,11].
The etiopathogenesis of breech is not very well understood. Many physicians regard it as an accidental phenomenon. Nonetheless, breech is more common when there is a concurrent fetal, uterine, or placental abnormality.
Almost one-quarter of fetuses at 28 wk of gestation are in the breech presentation, while only 4% are at-term. The transitional non-cephalic presentation is expected, especially earlier in pregnancy as a smaller fetus can easily rotate within a relatively large volume of amniotic fluid. However, as time goes forward, this becomes less plausible. The reasons why most fetuses assume cephalic presentation and why few do not are still disputed. However, the clinical implication here, when a fetal malpresentation is diagnosed at term in a singleton pregnancy, is to assess for underlying anomalies[3,12,13].
Various risk factors have been attributed to breech presentation. They can be categorized into three main groups: (1) Maternal (a history of breech in a previous pregnancy, multiparity as it results in a lax abdominal wall, primiparity, hypothyroidism, gestational diabetes, smoking, older or younger maternal age, delivery before term, and a personal history of being in breech); (2) Fetal (fetal neurologic deficit, anencephaly, hydrocephaly, macrosomia, fetal asphyxia, fetal growth restriction, multiple gestation, and female gender); and (3) Uteroplacental (oligohydramnios, polyhydramnios, uterine anomalies, bicornuate and unicornuate uterus, uterine didelphys, fibroids, and placenta previa) (Table 2)[14-17].
| Maternal | Fetal | Uteroplacental |
| A history of breech in a previous pregnancy | Fetal neurologic deficit | Oligohydramnios |
| Multiparity | Anencephaly | Polyhydramnios |
| Primiparity | Hydrocephaly | Uterine anomalies (bicornuate and unicornuate uterus, uterine didelphys) |
| Hypothyroidism | Macrosomia | Uterine fibroids |
| Gestational diabetes | Fetal asphyxia | Placenta previa |
| Smoking | ||
| Older or younger maternal age | ||
| Delivery before term | ||
| A personal history of being in breech |
Some women, in the third trimester, may complain of subcostal discomfort (fetal head in the fundus) or pain in the lower abdomen or groins (as the fetus kicks the cervix). However, these happen in normal pregnancies too, and are not considered specific or pathognomonic[8].
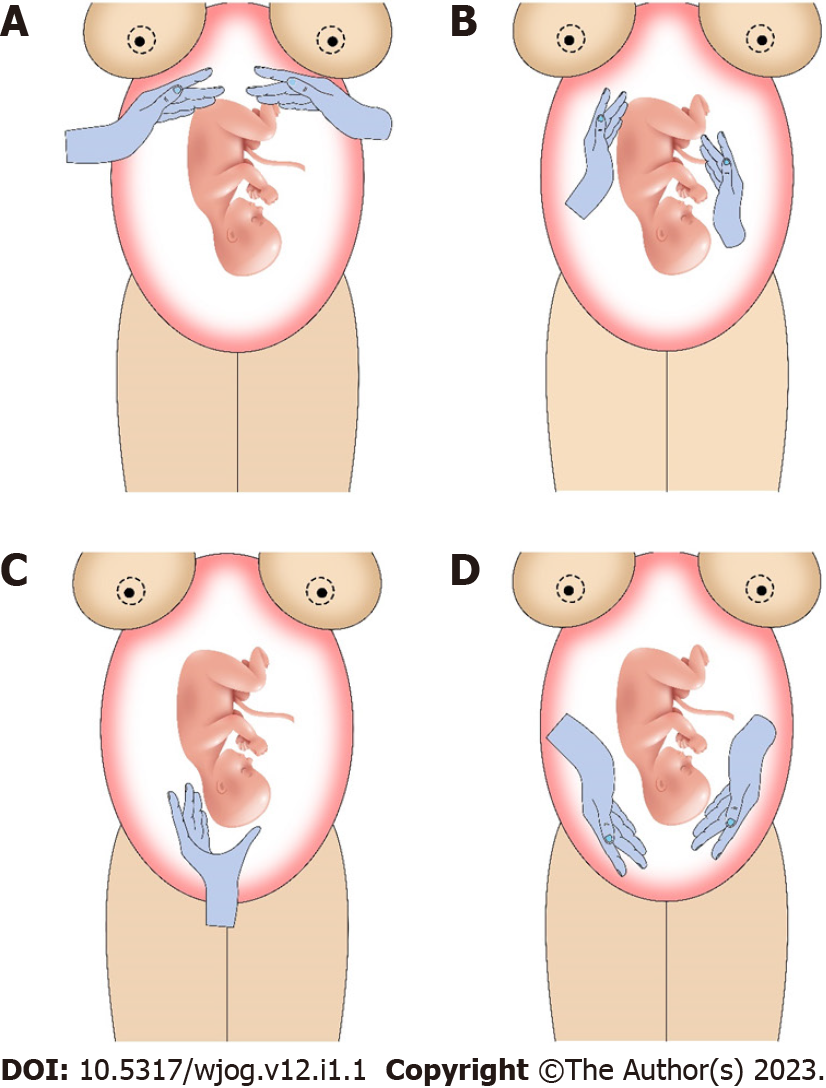
The physical examination includes inspection and transabdominal palpation of the fetus. The abdominal examination is performed through the Leopold maneuvers (Figure 2). The purpose of Leopold maneuvers is to determine the fetal lie, presentation, and engagement.
The physician should be at the right side of the patient, while she is placed in the dorsal recumbent position. The first step is a full inspection of the abdomen regarding its shape and size. The first maneuver is to measure the fundal height. Of note, the uterus, due to the pressure from the sigmoid colon, tends to rotate to its right. The dextrorotation of the uterus should be corrected before measuring the fundal height, which is an indicator of gestational age. The second maneuver is to determine the fetal lie (longitudinal, oblique, or transverse). The examiner assesses both lateral sides of the abdomen for that. Assessment of the upper and lower parts of the abdomen is the third maneuver or the Pawlik’s grip. The goal is to locate the fetal head. The last step is to assess if the fetal leading part is engaged in the pelvis. The provider must stand near the mother’s head, facing her feet, and with both hands assess the space between the fetus and maternal pelvis[18,19].
For assessment of the station, position, and attitude, a vaginal examination of the fetus is performed. The station is the location of the fetal leading part regarding the midpoint of the maternal pelvis (the ischial spines). The position or orientation is how the fetal leading part is situated in the anteroposterior axis of the maternal pelvis. For cephalic presentations, usually the occiput, and for breech presentations, the sacrum is a landmark to describe the position. The attitude describes the fetal head’s flexion or extension status.
The clinically valuable point for the care provider is not to misidentify the fetal buttocks (palpating the ischial tuberosities, anus, genitalia, sacrum, or lower limbs) with fetal head, face, and facial features and orifices. This is clinically very important as cephalic and breech presentations have different plans. Although, history and physical examination are crucial parts of any clinical encounter. However, relying solely on them and not utilizing imaging techniques can lead to misdiagnosis or under-diagnosis of malpresentations[6,19,20].
The gold standard for the diagnosis of fetal malpresentation is transabdominal ultrasonography. The fetal presentation and flexion or extension of the hips and knees (types of breech) can be easily evaluated through ultrasound. It also enables the care provider to assess for other structures and factors, such as placenta, umbilical cord, amniotic fluid volume, and estimated fetal weight. The fetal or uterine contraindications of vaginal delivery such as hyperextension of fetal head or very large uterine fibroids can be visualized too. Other advantages of ultrasonography include its low cost, acceptability, accessibility, and no major adverse effects.
Abdominal χ-ray, Computed Topography scan, and Magnetic Resonance Imaging are other modalities that can visualize a non-cephalic presenting fetus; however, are not recommended for routine clinical use[16,20-22].
Most guidelines recommend cesarean section as the desired approach for singleton breech pregnancies with gestational age at or after 39 wk. Two major studies, Term Breech Trial (TBT) in 2000 and Premoda in 2006, provided clinical evidence in favor of cesarean section.
TBT, a randomized controlled clinical trial in a multi-national setting, aimed to determine whether planned cesarean delivery or planned vaginal delivery benefits the breech-presenting fetuses more. This major study studied more than 200 singleton pregnancies in 26 countries. Perinatal and neonatal mortality and serious neonatal morbidity were the primary outcomes. Maternal mortality and serious maternal morbidity were regarded as secondary outcomes. The breech pregnancies undergoing cesarean section had significantly lower perinatal or neonatal mortality and serious neonatal morbidity, compared to the other cohort (risk ratio [RR] = 0.23, 95% confidence interval [CI]: 0.07–0.81, P = 0.01 and RR = 0.36, 95%CI: 0.19–0.65, P = 0.0003, respectively)[22,23].
Premoda, a prospective observational study of more than 800 term breech pregnancies, aimed to determine whether planned cesarean delivery or planned vaginal delivery benefits the breech-presenting fetuses more. The primary outcomes in Premoda included fetal or neonatal mortality and severe neonatal morbidity. This study assessed the babies up to one year after birth and based on its finding of no difference between the two groups, concluded that planned vaginal delivery is a safe approach for delivery of at-term breech pregnancies[24].
Providing all the information to the mother and educating her on the advantages and risks of both vaginal and cesarean deliveries is an essential duty for any health care provider. The physician should stay away from biases, ambiguity, and coercing the mother or himself/herself to any plans against anyone’s wishes, values, capabilities, or clinical judgment[25-29].
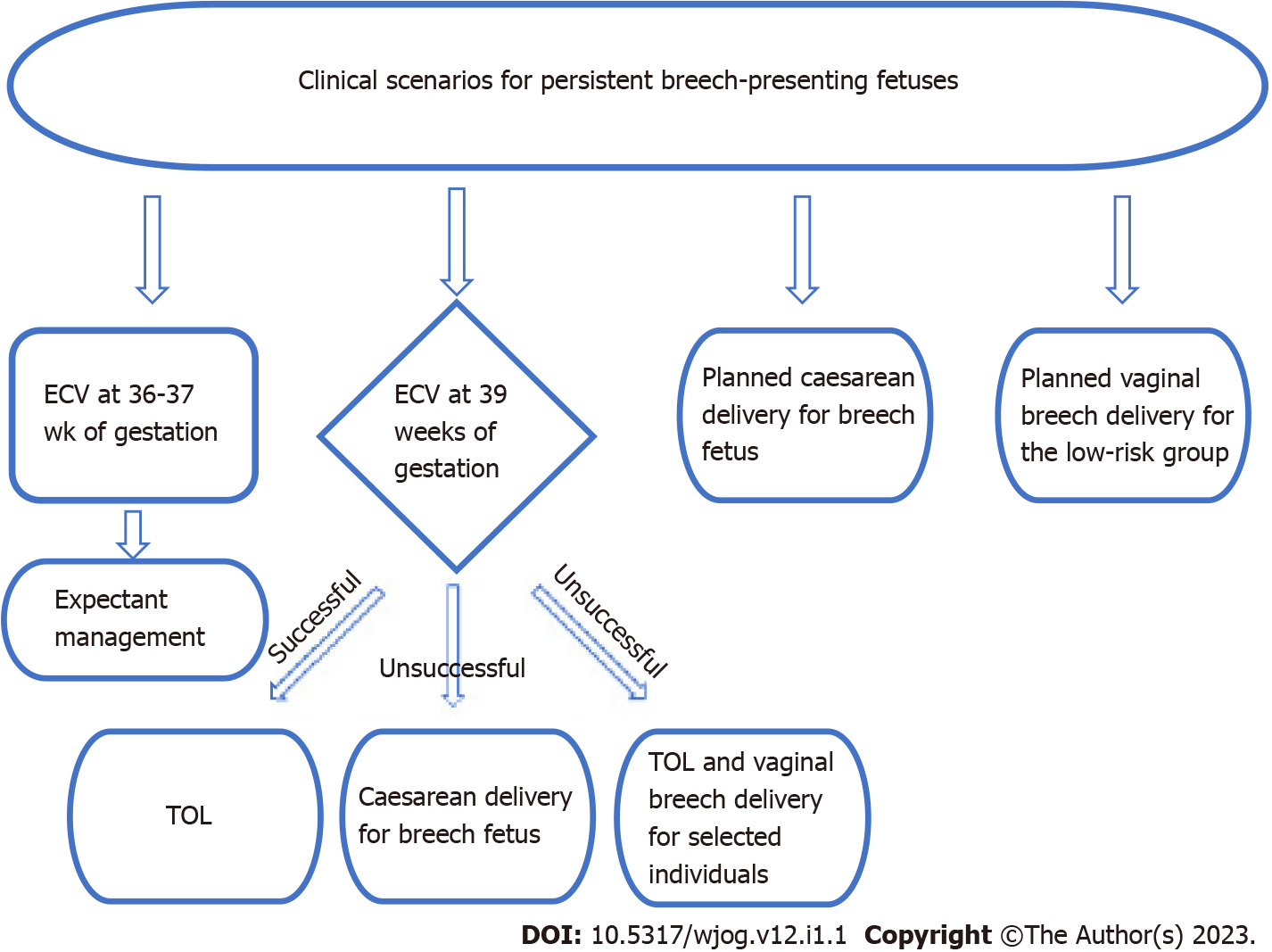
In general, six plans can be anticipated for persistent breech-presenting fetuses: (1) ECV at 36-37 wk of gestation and expectant management; (2) ECV at 39 wk of gestation and if successful, followed by a trial of labor; (3) ECV at 39 wk of gestation and if unsuccessful, followed by cesarean delivery for breech fetus; (4) ECV at 39 wk of gestation and if unsuccessful, followed by a trial of labor and vaginal breech delivery for selected individuals; (5) Planned cesarean delivery for breech fetus; and (6) Planned vaginal breech delivery for the low-risk group (Figure 3)[23,25-27,29].
Before any further elaboration on managing the scenarios, ECV shall be explained here.
ECV refers to a procedure aimed to convert a non-cephalic presenting fetus to a cephalic presenting. This procedure is performed manually through the mother’s abdomen by a trained health care provider, to reduce the likelihood of a cesarean section.
ECV is considered an elective manipulation when the labor process has not been initiated yet and should be indicated after a comprehensive evaluation of risks and contraindications, for both mother and fetus.
Overall, it is important to keep in mind that currently in the United States, a previous uterine surgery is the leading cause of cesarean-section, and non-cephalic pregnancies stand as the second[23,25-30].
Indications for ECV: ECV is indicated in any non-cephalic presenting singleton pregnancies in their late third trimester when there is no contraindication[23,26,27].
Contraindications for ECV: Any contraindication for labor or vaginal delivery is a contraindication for ECV. In addition to those regarded as the absolute contraindications for ECV, there are relative contraindications for ECV too. The contraindications can be due to maternal, uteroplacental, or fetal factors, including rupture of membranes, placental anomalies (placenta praevia, placenta accreta/ increta/percreta, and vasa praevia), placental abruption, maternal cardiac disease, a history of classical (high vertical) hysterotomy, two or more cesarean sections, antepartum bleeding, cephalopelvic disproportion, abnormal cardiotocography, fetal descent, and multiple gestation. Relative contraindications for ECV include fetal growth restriction, oligohydramnios, preeclampsia/hypertension, fetal growth restriction, fetal macrosomia > 4000 g, maternal obesity, and hyperextended fetal head[23,26,27,29,31]. Table 3 provides an overview of this information.
| Absolute contraindications (any contraindication for labor or a vaginal delivery) | Relative contraindications | ||
| Maternal | Fetal | Uteroplacental | Fetal growth restriction |
| Maternal cardiac disease | Abnormal cardiotocography (indeterminate fetal heart rate) | Rupture of membranes | Oligohydramnios |
| A history of classical (high vertical) hysterotomy | Fetal descent | Placental anomalies (placenta praevia, placenta accreta/increta/percreta, vasa praevia) | Preeclampsia/hypertension |
| A history of two or more Caeserean sections | Multiple gestation | Placental abruption | Fetal growth restriction |
| Cephalopelvic disproportion | Fetal macrosomia > 4000 g | ||
| Antepartum bleeding | Hyperextended fetal head | ||
| Maternal obesity | |||
Adverse events of ECV: Adverse events occur in < 1% of cases[23,25-27,29-30]. However, educating individuals on the risks of ECV is essential. Placental abruption, non-reassuring fetal tests, rupture of membranes, isoimmunization due to feto-maternal hemorrhage, and stillbirth are the most serious ones. Moreover, some subjects report it as uncomfortable[2,29,30].
Of note, ECV should be only performed in centers capable of performing emergency cesarean deliveries. After ECV fetus might experience tachycardia, bradycardia, decelerations, or instability in heart rate patterns, which may require an emergency cesarean delivery[23,25-27,29-30].
Success rates of ECV: A meta-analysis revealed a success rate of 58% for ECV. However, many factors are associated with ECV success. These include earlier gestational age, higher parity, trained health care provider, higher body mass index in mother, tocolytics, and epidural analgesia[29,30].
Acceptability of ECV: Various studies report that one-third to two-thirds of eligible individuals rejected ECV. Young age and lower parity are associated with a more negative attitude toward ECV[32].
Technical considerations for ECV: The first step is to reconfirm that the fetus is still assuming a non-cephalic presentation.
Obtaining informed consent is the next step. The facility should be fully set up for an emergency cesarean delivery in case it is needed[25,29]. After a satisfactory biophysical profile or a reactive fetal heart rate documented by a cardiotocography was noticed, tocolytics might be administered. Most commonly, β2 agonists are administered: Subcutaneous terbutaline 250 μg, or intravenous salbutamol 250 μg/20 mL normal saline. Neuraxial blockade or regional analgesia both are accepted methods that increase the chances of a successful ECV[29]. However, the advantages of administration of systemic opioids, abdominal lubricants, and amnioinfusion are still a matter of research, according to a 2015 Cochrane systematic review[33].
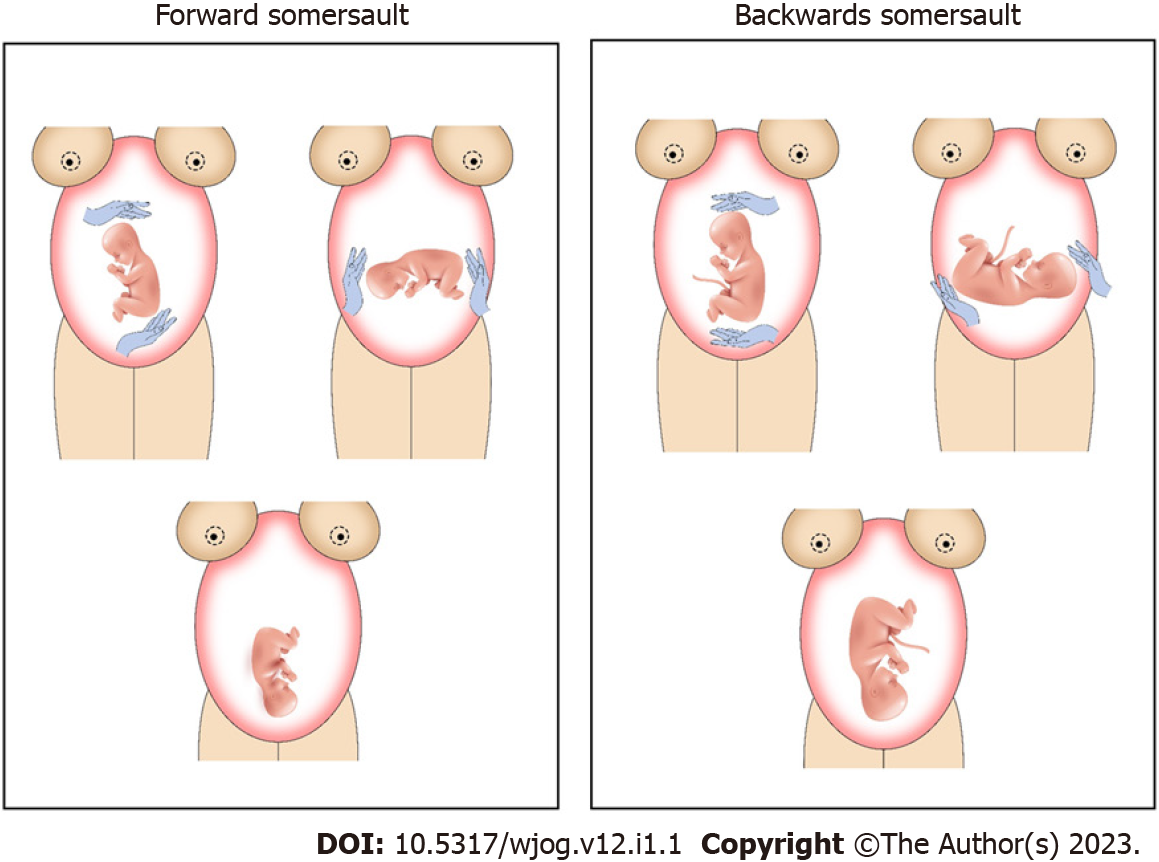
Applying either lubricant gel or cornstarch powder to the abdomen will facilitate the process. First, above the maternal symphysis pubis should be examined to know how deep the fetus has been engaged into the maternal pelvis. To successfully convert, the breech should be disengaged using the non-dominant hand. Thereafter, there are two techniques to perform ECV: Forward somersault, and backward. To perform the forward, using the dominant hand, the fetal head may be pushed forward toward the maternal symphysis pubis. If this maneuver yields no success after a few tries, the backward somersault shall be attempted. While the fetal head is being pushed back towards the symphysis pubis, the breech, with the dominant hand, is pushed forward to the uterine fundus. The recommended time for ECV is 10 min.
Monitoring the fetal heart rate for at least 30 min afterward, and isoimmunization of Rh(D)-negative individuals is recommended[29,30]. Please refer to Figure 4.
Alternatives to ECV: There are three proposed alternatives for ECV: (1) Watchful waiting: There is a chance for a natural conversion of the fetus as gestational age advances; (2) Postural techniques: The knee-chest position and elevated pelvis in supine are the postures that have been proposed as alternatives for ECV. However, systematic reviews have not found sufficient evidence to support the idea[29,34,35]; and (3) Moxibustion: Moxibustion is a traditional Chinese therapy consisting of burning mugwort on specific parts of the body coupled with acupuncture. It is hypothesized that the inhaled medicinal herb increases fetal movements, resulting in conversion. A Cochrane systematic review, however, found that the state-of-the-art body of evidence is not sufficient to recommend[35].
Even though the findings of the TBT trials effectively disfavored breech vaginal delivery, low-risk individuals may benefit from vaginal deliveries in well-equipped centers[23]. Of note, the relative risk of perinatal morbidity and mortality is two to five times more for vaginal breech delivery than cesarean delivery. According to a 2015 Cochrane systematic review, planned vaginal breech delivery enhances both the perinatal/neonatal mortality rates and serious neonatal morbidity rates. Nevertheless, this study emphasized the importance of the mother’s authority and individual risk-assessment of each case. Notably, after a breech vaginal delivery, about 90% of women stated that they would again consider breech vaginal delivery, according to an international survey[36,37].
The first fetal parts that show up in the birth canal are lower limbs; however, traction of these parts is highly discouraged. This might result in fetal head extending or enhancing the risk of nuchal arms. Fetal lower limbs and buttocks usually are delivered without any traction or pressure from the accoucheur. Current guidelines mostly discourage performing episiotomy for vaginal breech delivery. Facilitation of delivery of hips may lower the risk of neonatal developmental dysplasia of the hip (odds ratio [OR] = 5.7, 95%CI: 4.4-7.4)[38-43]. The accoucheur, holding the bony pelvis in hands, should rotate the fetus to the sacrum anterior position, after hips are delivered. To deliver the rest of the body, persistent, smooth traction and 180 degrees clockwise and counterclockwise rotation, should be applied several times. This maneuver is called Løvset maneuver, which may reduce risk of nuchal arms. To deliver the arms the accoucheur may grasp them cross the body as soon as the scapulae appear[38-42].
Delivery of the head in vaginal breech delivery requires lots of experience. A popular maneuver for this is the Mauriceau-Smellie-Veit maneuver. Before that, the fetal head needs to be flexed, not extended. When arms are almost delivered, the body should be elevated. As soon as the face is approachable, the mouth should be suctioned to clear the airway. The maneuver includes insertions of two or three fingers inside the birth canal and putting them on the fetal face to support and flex the head. The other hand, also inside the birth canal, should be put on the fetal neck and occiput, and flexion of the head smoothened. Moreover, an assistant can facilitate the vaginal breech delivery by applying pressure external on the maternal abdomen. However, if with all these techniques, the head is not delivered, no traction should be applied. In this case, utilization of piper forceps is recommended. Therefore, the fetal body is elevated while covered in a towel. The two blades are placed on the lateral sides of the head while applying pressure to flex the fetal head, and it will be delivered[38-42].
A not common position that might occur is the sacrum posterior position. This position can be complicated when the fetal chin cannot pass through the maternal symphysis pubis. In this case, the clinician should perform the modified Prague maneuver. This includes holding the fetal body with one hand and elevating fetal lower limbs with another hand and rotating the baby around the maternal symphysis pubis[38-42].
Entrapment of fetal arms and head are the most serious complications in breech. To reduce the risk of the “nuchal arm”, the Løvset maneuver (discussed earlier) should be performed.
Head entrapment is an obstetric emergency, as it can lead to asphyxia. The fetus will not get oxygenated through the umbilical cord, and the head trapped in the cervical canal cannot perfuse the brain. Pharmacologic therapy includes administration of β2 agonists, such as terbutaline or salbutamol, or nitroglycerine. The surgical approach includes making three incisions on the cervix, at 6, 2, and 10 o’clock. This approach is called Dührssen incisions. It especially benefits the preterm breech deliveries, as the fetus has a relatively larger head to the body, and the cervix is effaced while not dilated yet. First, the clinician should put two fingers inside the maternal cervix. This will help to separate the fetal body from the cervix. Then, they may incise the cervix at the three aforementioned points, utilizing bandage scissors. However, management of the incisions is challenging. Other less common approaches include general anesthesia and endotracheal intubation, the Zavanelli maneuver (reversing the delivery of fetal body and limbs and performing a cesarean section), and symphysiotomy on the mother[38-42].
It has been suggested that planned cesarean delivery, compared to vaginal delivery, is associated with lower perinatal morbidity and mortality (adjusted OR = 0.77, 95%CI: 0.63–0.93), lower neonatal mortality (30.2% vs 56.8%; P = 0.017), and higher maternal morbidity (anemia: 15.29% vs 10.04%, P = 0.005; wound infection: 0.001% vs 0.41%, P = 0.026)[44,45].
Cesarean delivery is considered the acceptable approach for delivery of the preterm breech fetus. In some specific cases, vaginal delivery is preferred, such as the delivery of a pre-viable fetus (earlier than 23 wk of gestation), a fetus with a non-compatible-with-life condition, and delivery of the breech twin B[25].
A higher rate of mortality and morbidity is observed in breech-presenting neonates. However, the causality relationship between the breech presentation and this phenomenon is not proven yet[46,47]. Sometimes there might be an underlying risk factor or condition that can develop both. Congenital anomalies, mild deformations, torticollis, and developmental dysplasia of the hip, without regard to the route of delivery, are more likely to present in neonates who were in breech[47,48].
Breech is a leading indication for cesarean surgery. ECV has a success chance of above 50%. ECV can be performed at 36 wk of gestation or at 39 wk of gestation. A trial of labor or cesarean delivery can be planned after an unsuccessful ECV. Fetus breech can be delivered by vaginal breech delivery or cesarean delivery. This review is proposing state-of-the-Art management for breech presentation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: international society of Prenatal Diagnosis.
Specialty type: Obstetrics and gynecology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: He Z, China; Ye W, China S-Editor: Liu XF L-Editor: Wang TQ P-Editor: Liu XF
| 1. | Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2015;CD000084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2015;CD000083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Mostello D, Chang JJ, Bai F, Wang J, Guild C, Stamps K, Leet TL. Breech presentation at delivery: a marker for congenital anomaly? J Perinatol. 2014;34:11-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Simm A. Fetal malpresentation. Obstet Gynaecol Reprod Med. 2007;17:283-288. |
| 5. | Pilliod RA, Caughey AB. Fetal Malpresentation and Malposition: Diagnosis and Management. Obstet Gynecol Clin North Am. 2017;44:631-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Bellussi F, Ghi T, Youssef A, Salsi G, Giorgetta F, Parma D, Simonazzi G, Pilu G. The use of intrapartum ultrasound to diagnose malpositions and cephalic malpresentations. Am J Obstet Gynecol. 2017;217:633-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 7. | Baethge C, Goldbeck-Wood S, Mertens S. SANRA-a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019;4:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 248] [Cited by in RCA: 892] [Article Influence: 148.7] [Reference Citation Analysis (0)] |
| 8. | Azimirad A, Norwitz ER. Fetal Malpresentation in Pregnancy. In: Norwitz Errol R, editor. Obstetrics and Gynecology. Toronto: Decker Medicine; 2020 April. [DOI] [Full Text] |
| 9. | Ghesquière L, Demetz J, Dufour P, Depret S, Garabedian C, Subtil D. Type of breech presentation and prognosis for delivery. J Gynecol Obstet Hum Reprod. 2020;49:101832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Hardy JR. Intergenerational recurrence of breech delivery. BMJ. 2008;336:843-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Maskey S, Dwa Y. Predisposing factors and outcome of malpresentations in an institute. J Nepal Med Assoc. 2018;56:674-677. |
| 12. | Fox AJ, Chapman MG. Longitudinal ultrasound assessment of fetal presentation: a review of 1010 consecutive cases. Aust N Z J Obstet Gynaecol. 2006;46:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Skupski DW. Association is not causation! Am J Obstet Gynecol. 2016;214:133-134. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Cui H, Chen Y, Li Q, Chen J, Liu C, Zhang W. Cesarean rate and risk factors for singleton breech presentation in China. J Reprod Med. 2016;61:270-274. |
| 15. | Macharey G, Gissler M, Rahkonen L, Ulander VM, Väisänen-Tommiska M, Nuutila M, Heinonen S. Breech presentation at term and associated obstetric risks factors-a nationwide population based cohort study. Arch Gynecol Obstet. 2017;295:833-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Sharshiner R, Silver RM. Management of fetal malpresentation. Clin Obstet Gynecol. 2015;58:246-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Witkop CT, Zhang J, Sun W, Troendle J. Natural history of fetal position during pregnancy and risk of nonvertex delivery. Obstet Gynecol. 2008;111:875-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Watson WJ, Welter S, Day D. Antepartum identification of breech presentation. J Reprod Med. 2004;49:294-296. |
| 19. | Nassar N, Roberts CL, Cameron CA, Olive EC. Diagnostic accuracy of clinical examination for detection of non-cephalic presentation in late pregnancy: cross sectional analytic study. BMJ. 2006;333:578-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Ressl B, O'Beirne M. Detecting breech presentation before labour: lessons from a low-risk maternity clinic. J Obstet Gynaecol Can. 2015;37:702-706. |
| 21. | Wastlund D, Moraitis AA, Dacey A, Sovio U, Wilson ECF, Smith GCS. Screening for breech presentation using universal late-pregnancy ultrasonography: A prospective cohort study and cost effectiveness analysis. PLoS Med. 2019;16:e1002778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 22. | Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR. Planned caesarean section vs planned vaginal birth for breech presentation at term: A randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet. 2000;356:1375-1383. |
| 23. | ACOG Committee Opinion No. 745: Mode of Term Singleton Breech Delivery. Obstet Gynecol. 2018;132:e60-e63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 24. | Goffinet F, Carayol M, Foidart JM, Alexander S, Uzan S, Subtil D, Bréart G; PREMODA Study Group. Is planned vaginal delivery for breech presentation at term still an option? Am J Obstet Gynecol. 2006;194:1002-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 309] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 25. | Management of Breech Presentation: Green-top Guideline No. 20b. BJOG. 2017;124:e151-e177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 90] [Article Influence: 11.3] [Reference Citation Analysis (1)] |
| 26. | Kotaska A, Menticoglou S. No. 384-Management of Breech Presentation at Term. J Obstet Gynaecol Can. 2019;41:1193-1205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 27. | ACOG Committee Opinion No. 745 Summary: Mode of Term Singleton Breech Delivery. Obstet Gynecol. 2018;132:531-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 28. | Morton R, Burton AE, Kumar P, Hyett JA, Phipps H, McGeechan K, de Vries BS. Cesarean delivery: Trend in indications over three decades within a major city hospital network. Acta Obstet Gynecol Scand. 2020;99:909-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 29. | External Cephalic Version and Reducing the Incidence of Term Breech Presentation: Green-top Guideline No. 20a. BJOG. 2017;124:e178-e192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 30. | American College of Obstetricians and Gynecologists' Committee on Practice Bulletins--Obstetrics. Practice Bulletin No. 161: External Cephalic Version. Obstet Gynecol. 2016;127:e54-e61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 31. | Weill Y, Pollack RN. The efficacy and safety of external cephalic version after a previous caesarean delivery. Aust N Z J Obstet Gynaecol. 2017;57:323-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 32. | Nassar N, Roberts CL, Cameron CA, Peat B. Outcomes of external cephalic version and breech presentation at term, an audit of deliveries at a Sydney tertiary obstetric hospital, 1997-2004. Acta Obstet Gynecol Scand. 2006;85:1231-1238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Cluver C, Gyte GM, Sinclair M, Dowswell T, Hofmeyr GJ. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015;CD000184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 34. | Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012;10:CD000051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 35. | Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev. 2012;CD003928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015;CD000166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 37. | Petrovska K, Watts NP, Catling C, Bisits A, Homer CS. Supporting Women Planning a Vaginal Breech Birth: An International Survey. Birth. 2016;43:353-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 38. | Hofmeyr GJ, Kulier R, West HM. Expedited versus conservative approaches for vaginal delivery in breech presentation. Cochrane Database Syst Rev. 2015;CD000082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 39. | Tunde-Byass MO, Hannah ME. Breech vaginal delivery at or near term. Semin Perinatol. 2003;27:34-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 40. | Mukhopadhyay S, Arulkumaran S. Breech delivery. Best Pract Res Clin Obstet Gynaecol. 2002;16:31-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | Barbash-Hazan S, Nattiv N, Salzer-Sheelo L, Bergel R, Hadar E, Osovsky M, Shmueli A. Induction of labor versus expectant management after successful external cephalic version. Birth. 2019;46:623-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 42. | Kotaska A, Menticoglou S, Gagnon R, Farine D, Basso M, Bos H, Delisle MF, Grabowska K, Hudon L, Mundle W, Murphy-Kaulbeck L, Ouellet A, Pressey T, Roggensack A; Society of Obstetricians and Gynaecologists of Canada. SOGC clinical practice guideline: Vaginal delivery of breech presentation: no. 226, June 2009. Int J Gynaecol Obstet. 2009;107:169-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 68] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 43. | de Hundt M, Vlemmix F, Bais JM, Hutton EK, de Groot CJ, Mol BW, Kok M. Risk factors for developmental dysplasia of the hip: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2012;165:8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 115] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 44. | Bergenhenegouwen L, Vlemmix F, Ensing S, Schaaf J, van der Post J, Abu-Hanna A, Ravelli ACJ, Mol BW, Kok M. Preterm Breech Presentation: A Comparison of Intended Vaginal and Intended Cesarean Delivery. Obstet Gynecol. 2015;126:1223-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Demirci O, Tuğrul AS, Turgut A, Ceylan S, Eren S. Pregnancy outcomes by mode of delivery among breech births. Arch Gynecol Obstet. 2012;285:297-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 46. | Azria E, Kayem G, Langer B, Marchand-Martin L, Marret S, Fresson J, Pierrat V, Arnaud C, Goffinet F, Kaminski M, Ancel PY; EPIPAGE study group. Neonatal Mortality and Long-Term Outcome of Infants Born between 27 and 32 Weeks of Gestational Age in Breech Presentation: The EPIPAGE Cohort Study. PLoS One. 2016;11:e0145768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 47. | Macharey G, Gissler M, Toijonen A, Heinonen S, Seikku L. Congenital anomalies in breech presentation: A nationwide record linkage study. Congenit Anom (Kyoto). 2021;61:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 48. | Humphry S, Hall T, Hall-Craggs MA, Roposch A. Predictors of Hip Dysplasia at 4 Years in Children with Perinatal Risk Factors. JB JS Open Access. 2021;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |