Published online Sep 30, 2021. doi: 10.5317/wjog.v10.i2.16
Peer-review started: February 25, 2021
First decision: May 14, 2021
Revised: May 16, 2021
Accepted: August 25, 2021
Article in press: August 25, 2021
Published online: September 30, 2021
Processing time: 214 Days and 18.9 Hours
Teenage pregnancy is a challenging issue worldwide. Yet, despite the increased health risk and socioeconomic impact of teenage pregnancy, the numbers remain high in Nepal.
To determine the prevalence and sociodemographic factors associated with teenage pregnancy in Nepal.
A hospital-based cross-sectional study was conducted in the Paropakar Maternity and Women’s Hospital from April to August 2017. A total of 1359 mothers were assessed and interviewed regarding their reproductive history and sociodemographic attributes. Ethical approval from the Nepal Health Research Council, permission from the concerned hospital, and consent from study subjects were obtained.
Of the 5526 deliveries, 679 (12.3%) were teenage pregnancy deliveries. The majority (85.1%) of mothers (out of 1359) were married at < 20 years of age, with a mean age of marriage of 17.57 years (± 1.994, range: 12-25 years). Marriage age was a significant determinant of teenage pregnancy (odds ratio [OR] 2.423 [2.262-2.596]; P < 0.001). Likewise, a love marriage (OR: 2.018 [1.585-2.570]; P < 0.001) and first teenage pregnancy (OR: 3.622 [3.265-4.017]; P < 0.001) were significant determinants for subsequent teen pregnancies. Knowledge of family planning methods (OR: 0.474; 0.288-0.779; P = 0.003) and use of any methods of family planning utilization (OR: 0.345; 0.248-0.479; P = 0.000) significantly lowered the chance of teenage pregnancy.
Teenage pregnancy occupies a substantial proportion of total deliveries in the Nepalese maternity hospital. In addition, early pregnancy was significantly associated with age and type of marriage, education level, knowledge, and practice of contraceptive methods.
Core Tip: This study evaluated the prevalence and sociodemographic factors associated with teenage pregnancy in Nepal. Teenage pregnancy carries a significant proportion of total deliveries in a Nepalese maternity hospital. Early pregnancy was significantly associated with age at marriage, education level, type of marriage, and contraceptive practice.
- Citation: Thapa P, Thapa P, Shrestha DB, Budhathoki P, Karki B, Mahat B. Teenage pregnancy and the sociodemographic attributes as a major contributor: Findings from an urban referral center in Nepal. World J Obstet Gynecol 2021; 10(2): 16-25
- URL: https://www.wjgnet.com/2218-6220/full/v10/i2/16.htm
- DOI: https://dx.doi.org/10.5317/wjog.v10.i2.16
The United Nations Childrens Fund defines teenage pregnancy as pregnancy in a girl aged 13-19 years[1]. This usually refers to pregnant girls who have not reached legal adulthood, which varies worldwide. Approximately 21 million girls aged 15 to 19 years and 2 million girls under 15-years-old become pregnant in developing regions every year[2]. About 16 million girls aged 15-19 years and 2.5 million girls under age 16 give birth in developing regions[3]. In South Asia, the early marriage of adolescents is common, and 25%–35% of adolescent girls in Pakistan, Bangladesh, India, and Nepal begin childbearing as early as 17 years[4]. About 90% of births to adolescents occur within marriage in developing countries, mainly due to customs and traditions and lack of education and information about reproductive and sexual health[5,6]. Various socioeconomic problems such as school dropout and unemployment and psychological issues such as depression are also common among teenage pregnancy[7,8]. In addition, multiple factors including rural residence, not attending school, low educational status of parents and lack of communication between teenagers and parents on sexual and reproductive health issues, and lack of knowledge about contraceptive methods are associated with teenage pregnancy[9].
Teenage pregnancy is a challenging issue for families and adolescent parents. It is associated with higher rates of morbidity and mortality for both the mother and infant. Teenage pregnancy is associated with an increased risk of neonatal complications like prematurity, low birth weight, intrauterine growth restriction, neonatal mortality, and stillbirth[5,6,10]. Maternal complications such as pregnancy-induced hypertension, preeclampsia, malnutrition and anemia in pregnancy, perineal tear, episiotomy, and cesarean delivery are also common among teenagers[11,12]. Risks for medical complications are more significant for girls ≤ 14 years of age, as an underdeveloped pelvis can lead to difficulties in childbirth[13]. In Nepal, where marriage is universal and occurs at young ages, early teenage pregnancy is of prime public health importance. This study was conducted to determine the burden of teenage pregnancy in an urban referral maternity hospital of Nepal and to analyze sociodemographic factors as determinants.
A hospital-based cross-sectional study was carried out from April to August 2017 to determine the proportion of teenage deliveries and factors associated with early pregnancy. Study samples were selected from the Paropakar Maternity and Women's Hospital, a tertiary level referral maternity hospital in Nepal and the only semi-government hospital providing maternity services to the general public. Mothers who attended the study hospital for the delivery during the study period were interviewed, and data on sociodemographic characteristics, reproductive history, and social behaviors were collected.
Cases consisted of all teenage women who came to the hospital for delivery. They were interviewed during the prenatal period and 1 or 2 d postpartum depending on the mother’s level of comfort and readiness. In addition, women who came to the same hospital for delivery and were aged ≥ 20 years were selected randomly in equal numbers within 24 h for comparison purposes, and constituted the controls.
A pretested semi-structured questionnaire in the Nepali language was used to interview 1359 patients. Female interviewers with health backgrounds were recruited and trained on sampling, interview techniques, and subjects’ rights and comfort. Information on sociodemographic characteristics, reproductive history, and knowledge and practice on contraceptive methods was obtained. The data collection sheet is attached as supplementary file.
Sociodemographic variables: Marital status (marriage age, type), ethnicity (Brahmin and Chhetri or others), religion (Hindu or others), family type (nuclear, joint or extended), age of first pregnancy, educational status (of the patient and her husband), occupation (of patient and husband), family planning (knowledge and practice of patient), parent's education and work.
Type of family: Nuclear meant parents and children only, joint meant grandparents, parents, and children while extended meant including families of brothers and grandparents and children.
Teenage pregnancy: A pregnant woman under 20 years of age was the dependent variable for this study.
Religion: Hindu was the most common religion. Other religions included Christian, Muslims, and Buddhists.
Educational status: We recorded the academic level of the patient, her mother, and her husband. Education was categorized into two categories: "educated" referred to people who studied to Grade 8 or above and "uneducated" referred to illiterate people or those who studied to less than Grade 8.
Occupation: Classified into two categories: "employed" referred to people working for governmental or non-governmental organizations or doing their own business or labor and "un-employed" referred to people with no formal job/work but doing something to sustain life.
Family planning knowledge: Classified into two categories: those who knew about the basics of family planning, including family planning methods, were classified as "Yes" and those with no information or insight about family planning were classified as "No."
Family planning practice: Classified into two categories: those who used any family planning device were recorded as "Yes" and those who had never used any method of family planning were recorded as "No."
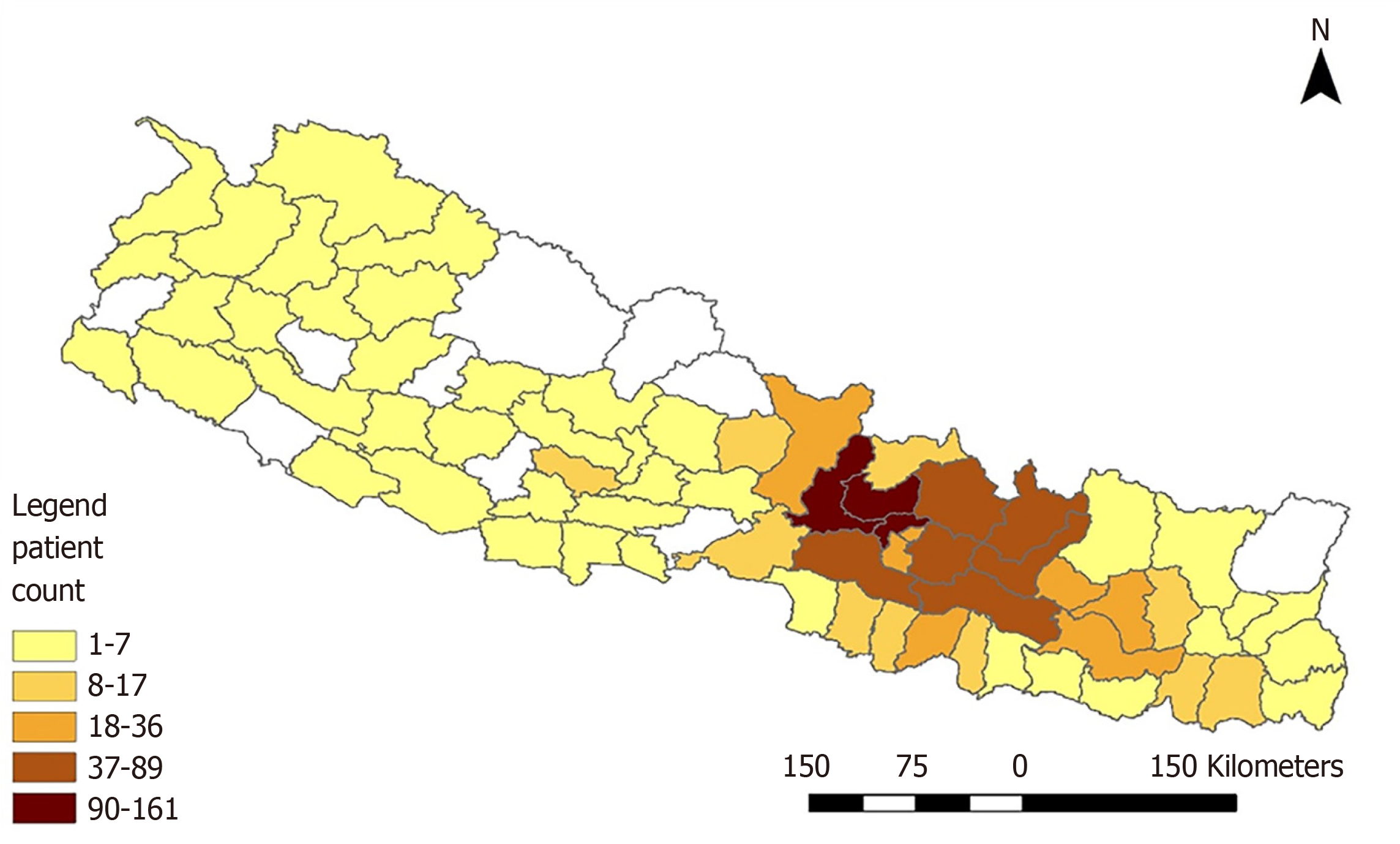
Data were entered in EPIDATA version 2.0 and imported and analyzed using SPSS version 22 (Statistical Package for Social Sciences, Chicago, IL, United States). Univariate analyses were conducted for all studied variables and presented as the frequency and percentage in the appropriate tables to evaluate the distribution of each sociodemographic variable. Later cross-tabulation analyses were done between teen and non-teenage pregnancy using the χ2 test and risk ratios. Finally, logistic regression analyses were run to estimate the odds ratios of relevant predicting variables to explore how predictor X (exposure variables) is related to Y (outcome variable) with a dichotomous response. We defined the response as Y = 0 or 1, where Y = 1 denotes our event of interest occurrence; here, it was non-teenage pregnancy = 0 and teen pregnancy = 1. The exposure variables were edited and made categorical for study convenience as appropriate. ArcGIS was used to evaluate the spatial distribution of patients enrolled in the study across Nepal based on their permanent residency address.
Teenage mothers were further divided into two groups for the analyses: age ≤ 17 years and age > 17 years.
Informed consent was provided from all respondents meeting the inclusion criteria before enrollment in the study. The study protocol was approved by the Ethical Review Board of Nepalese Health Research Council and conducted according to the protocol.
A total of 5526 deliveries occurred in Paropakar maternity hospital in the study period from April 14, 2017 to August 14, 2017. Of the 1359 women, 679 teenage mothers (12.28%) matched to 680 non-teen mothers, were enrolled. The menarche age of the included cohort was 13.55 ± 1.342 (range: 9-18) years. The majority of participants were married under age 20 with a mean age of marriage of 17.57 ± 1.994 (range: 12-25) years. Most married females were living with their husbands, and more than two-thirds were in love marriages. Most reported their first pregnancy as teenagers at a mean age of 18.50 ± 2.145 (range: 13-25) years. Nearly one-third of participants were from Brahmin and Chhetri ethnicity (upper caste), with the majority following Hinduism. In total, 58.9% of participants were living in a nuclear family, and 71.5% had above Grade 8 education. However, only 16.6% reported formal employment, and 79.8% said their pregnancy was planned (Table 1).
| Variables | n (%) | ||
| Type of pregnancy | Teen | 679 (50.0) | |
| Non teenage | 680 (50.0) | ||
| Age of marriage in yr | Teenage | 1156 (85.1) | |
| Non-teenage | 203 (14.9) | ||
| Living arrangement | Married and living with husband | 1261 (92.8) | |
| Marriage type | Love marriage | 972 (71.5) | |
| Teen | 938 (69.0) | ||
| Temporary address | In the Kathmandu valley | 1116 (82.1) | |
| Outside the valley | 243 (17.9) | ||
| Permanent address | In the Kathmandu valley | 169 (12.4) | |
| Outside the Valley | 1190 (87.6) | ||
| Ethnicity | Upper Caste | 398 (29.3) | |
| Others | 961 (70.7) | ||
| Religion | Hindu | 1046 (77.0) | |
| Family type | Nuclear | 800 (58.9) | |
| Education | Grade ≥ 8 | Patient | 972 (71.5) |
| Husband | 961 (70.7) | ||
| Mother | 71 (5.2) | ||
| Illiterate/< Grade 8 | Patient | 387 (28.5) | |
| Husband | 397 (29.2) | ||
| Mother | 1288 (94.8) | ||
| Employment | Formally employed | Patient | 225 (16.6) |
| Husband | 644 (47.4) | ||
| Unemployed | Patient | 1134 (83.4) | |
| Husband | 714 (52.5) | ||
| Knowledge of family planning | Yes | 1141 (84.0) | |
| Use of any family planning methods | No | 887 (65.3) | |
| Present pregnancy | Planned | 1085 (79.8) | |
Based on the permanent address of residency among the participants in the study, spatial distribution showed that the majority of participants were from province three. Still, overall, the different districts of Nepal were represented. Therefore, 1337 individuals with permanent residency in Nepal were plotted after excluding 22 Indian national Figure 1. Details of address and sociodemographic determinants are included in the supplementary files (Supplementary Table 1, Supplementary material and Table 1 ).
Table 2 depicts each sociodemographic determinant of pregnancy and its association with teenage and non-teenage pregnancy. Determinants of teenage pregnancy were: age at marriage (P ≤ 0.001), love marriage (P ≤ 0.001), and being a teenager at first pregnancy (P ≤ 0.001). In addition, belonging to the upper caste (P = 0.001), higher education of the patient (P ≤ 0.001) and husband (P = 0.002), knowledge of family planning (P ≤ 0.001), and use of family planning (P ≤ 0.001) were negatively associated with teenage pregnancy (Table 2).
| Variables | Present pregnancy type | Unadjusted OR (95%CI) | ||
| Non teenage, n (%) | Teen, n (%) | |||
| Age marriage | Below 20 | 477 (41.3) | 679 (58.7) | 2.423 (2.262-2.596)1 |
| Living arrangement | Married and living with husband | 631 (50.0) | 630 (50.0) | 0.998 (0.662-1.506) |
| Marriage type | Love marriage | 439 (45.2) | 533 (54.8) | 2.018 (1.585-2.570)1 |
| Age 1st pregnancy | Teen | 259 (27.6) | 679 (72.4) | 3.622 (3.265-4.017)1 |
| Temporary address | In the valley | 569 (51.0) | 547 (49.0) | 1.237 (0.936-1.634) |
| Permanent address | In the valley | 93 (55.0) | 76 (45.0) | 1.257 (0.909-1.737) |
| Ethnicity | Upper Caste | 227 (57.0) | 171 (43.0) | 1.489 (1.176-1.884)1 |
| Religion | Hindu | 536 (51.2) | 510 (48.8) | 0.811 (0.629-1.044) |
| Family Type | Nuclear | 404 (50.5) | 396 (49.5) | 0.956 (0.770-1.187) |
| Education-patient | Grade 8 or above | 519 (53.4) | 453 (46.6) | 1.608 (1.267-2.041)1 |
| Education-husband | Grade 8 or above | 507 (52.8) | 454 (47.2) | 1.446 (1.143-1.830)1 |
| Education-mother | Grade 8 or above | 34 (47.9) | 37 (52.1) | 1.095(0.679-1.767) |
| Employment-patient | Unemployed | 562 (49.6) | 572 (50.4) | 1.122 (0.843-1.495) |
| Employment-husband | Unemployed | 357 (50.0) | 357 (50.0) | 1.006 (0.813-1.245) |
| Knowledge of family planning | Yes | 626 (54.9) | 515 (45.1) | 3.692 (2.657-5.129)1 |
| Use of any family planning methods | Yes | 307 (65.0) | 165 (35.0) | 2.564 (2.034-3.232)1 |
| Present pregnancy | Planned | 548 (50.5) | 537 (49.5) | 0.911 (0.699-1.188) |
Arranged marriage has a 45% lower chance of teenage pregnancy compared to love marriage. Participants' education status of higher than Grade 8 showed a 33% lower chance of teen pregnancy as an outcome compared to education lower than Grade 8. Knowledge of family planning methods and use of any forms of family planning are associated with significantly lower teenage pregnancy rates (Table 3).
| Variables | Adjusted OR | 95%CI for OR | P value | ||
| Lower | Upper | ||||
| Marriage age | At or above 20 | 1.040 | 0.000 | . | 1.000 |
| Below 201 | |||||
| Marital state and living with | Husband abroad, separated or others | 0.902 | 0.477 | 1.708 | 0.752 |
| Married and living with husband1 | |||||
| Marriage type | Arrange marriage | 0.550 | 0.389 | 0.778 | 0.001b |
| Love marriage1 | |||||
| 1st pregnancy based on age | Non Teen | 0.000 | 0.000 | . | 0.993 |
| Teen1 | |||||
| Temporary address | In the Kathmandu valley | 1.093 | 0.699 | 1.710 | 0.696 |
| Outside the valley1 | |||||
| Permanent address | In the Kathmandu valley | 1.215 | 0.712 | 2.072 | 0.475 |
| Outside the valley1 | |||||
| Ethnicity | Upper caste | 0.884 | 0.619 | 1.260 | 0.495 |
| Others1 | |||||
| Religion | Others | 0.938 | 0.646 | 1.361 | 0.735 |
| Hindu1 | |||||
| Family type | Joint or extended | 1.192 | 0.826 | 1.722 | 0.348 |
| Nuclear1 | |||||
| Education status | Grade 8 or above | 0.670 | 0.522 | 0.861 | 0.002b |
| Illetrate or less than Grade 81 | |||||
| Husband Education status | Grade 8 or above | 0.783 | 0.611 | 1.003 | 0.053 |
| Illetrate or less than Grade 81 | |||||
| Education status of Mother | Grade 8 or above | 1.095 | 0.679 | 1.767 | 0.710 |
| Illiterate or less than Grade 81 | |||||
| Employment status | Formally employed | 0.988 | 0.646 | 1.511 | 0.956 |
| Unemployed1 | |||||
| Husband Employment status | Formally employed | 0.807 | 0.590 | 1.104 | 0.180 |
| Unemployed1 | |||||
| Knowledge of family planning | Yes | 0.474 | 0.288 | 0.779 | 0.003b |
| No1 | |||||
| Use of any family planning methods | Yes | 0.345 | 0.248 | 0.479 | 0.000c |
| No1 | |||||
| Present pregnancy | Unplanned | 0.911 | 0.635 | 1.307 | 0.612 |
| Planned1 | |||||
Our cross-sectional study evaluated different sociodemographic factors responsible for teenage pregnancy in Nepal. The prevalence of adolescent pregnancy in Africa is 18.8%[9]. The teenage pregnancy prevalence was found to be 12.28% in the tertiary center of Nepal in our study, which is lower than the national rate of 19.8% of Nepal but is higher than the rate of 4.5% in South-Eastern Asia[14]. We found that early age at marriage is a significant factor associated with teenage pregnancy. In Nepal, early marriage occurs due to societal norms in which families marry their daughter at an early age, believing it will cut the expense[15]. Those married at an early age have decreased knowledge about reproductive health and contraception, leading to unwanted pregnancy. Similar findings of teenage pregnancy association with earlier marriage age have also been found in Africa[14]. A retrospective study showed the increased role of parents in early marriage without the daughter's consent[16]; however, most marriages in our research were love marriages. This might be explained because most of the study population lived in Kathmandu, although they were from outside the valley. Due to migration to Kathmandu, many teenage females gain independence and might have indulged in sexual relationships leading to marriage. Another significant finding of our study was that girls with higher education more than Grade 8 have significantly decreased chances of pregnancy compared to illiterate or low education girls. This is in agreement with the Nepalese Demographic and Health Survey (NDHS), which showed that girls with an education of Grade 10 or more get pregnant 4 years later than uneducated ones, and about 44.1% of teenage pregnancies occur in uneducated or girls with education level of primary[3]. The pooled analyses of the data from three national NDHS surveys showed that teenage pregnancy is associated with a low level of education, similar to our study[7].
Similarly, a cross-sectional study done in another tertiary center of Nepal showed that teenage pregnancies were seen in females who dropped out of school for various reasons[8]. Also, the studies done by Sharma et al[15] and Shrestha[16] showed an increased association of teenage pregnancies with lower education levels[15,16]. There is a similar scenario of low education being associated with teenage pregnancy in Africa and South Asia because the lack of education prevents the empowerment of teenagers with the necessary skills and knowledge to prevent pregnancy[14,17].
The lack of knowledge of family planning and use of family planning methods were significantly associated with teenage pregnancies in our study. Social stigma prohibits discussion and education about reproductive health in Nepal, leading to unsafe sex. The retrospective study done by Shrestha[16] found that a minimal number of teenage girls used any form of contraception[16]. Although various studies have suggested that teenage girls know about contraception all over South Asia, the lack of proper contraception in teenagers is the main problem. Our study found that teenage girls lack this knowledge, which contributes to teenage pregnancy[17]. Similar findings of lack of sexual knowledge have been reported in Africa, as well as a lack of access to contraceptives and unfavorable attitude of the community towards contraception[14]. Our study found no association of teenage pregnancy with employment status, in contrast with the pooled analysis done by Poudel et al[7], who showed lower teenage pregnancy rates among skilled professional women[7].
Similarly, we did not find an effect of upper caste on teenage pregnancy while doing multivariate logistic regression, unlike a prior study that showed a lower rate of teenage pregnancy in upper-caste like Brahmin and Chettri[10]. Our study found no association between religion and teenage pregnancy. However, a study done by Shrestha[16] found that Hindu teenagers are more likely to be pregnant than Buddhist teenagers[16]. There was no association between type of family and teenage pregnancy in our study.
Although our study had an adequate sample size and good statistics, there were several limitations. First, our study was done in a tertiary center in the developed city of Kathmandu; hence it cannot be generalized to the entire population. Second, we did not evaluate the role of economic status in teenage pregnancy, a factor that is a strong determinant in teenage pregnancies[7,17].
Teenage pregnancy constituted a significant proportion of deliveries at the urban referral center of Nepal. There was a significant association between teenage pregnancies and early age at marriage. Love marriages, low level of education, lack of knowledge of family planning and contraception were substantial determinants of teenage pregnancy.
Teenage pregnancy is a global problem with increased prevalence in developing nations. It is associated with various maternal and neonatal complications. Multiple factors including rural residence, low level of education, and lack of contraceptive knowledge are believed to play a role in teenage pregnancy.
Studies regarding the prevalence of teenage pregnancy and various associated factors associated are rare in Nepal. Therefore, our goal was to study the status of teenage pregnancy among patients visiting a tertiary center in the capital city of Nepal.
The study’s objective was to determine the proportion of teenage pregnancy and the effects of various sociodemographic factors on pregnant women visiting the tertiary center of Nepal.
We conducted a hospital-based cross-sectional study in a tertiary center from April to August 2017. Pregnant women were interviewed regarding their reproductive history and sociodemographic variables. Before the interview, informed consent was provided, and ethical approval was given from Nepal Health Research Council.
The prevalence of teenage pregnancy was 12.3%. More than four-fifths of the mothers were married under 20-years-old. Love marriage and first teenage pregnancy increased the odds for subsequent teenage pregnancies. On the other hand, knowledge of family planning methods and first teenage pregnancy lowered the odds of teenage pregnancy.
Teenage pregnancy was highly present at the tertiary center of Nepal. Teenage pregnancy was associated with marriage at an early age. Increased odds of teenage pregnancy were seen among mothers with low education, lack of knowledge of family planning, and use of contraception.
Developing nations like Nepal should focus on raising awareness of contraception and improving people's education and awareness to better tackle the adverse maternal and neonatal effects caused by teenage pregnancy.
We express our sincere gratitude to Professor Dr. Narbada Thapa and Late. Professor Dr.Babill Stray-Pedersen for their valuable guidance and technical support throughout the study period. We are thankful to the field supervisors, enumerators, and data entry operators for contributing to the study. Finally, we sincerely acknowledge the study participants for their valuable participation.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Nepal Medical Association, No. 6859/L-6319; Nepal Medical Council, No. 21732.
Specialty type: Obstetrics and gynecology
Country/Territory of origin: United States
Peer-review report's scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gbolade BA, Usta I S-Editor: Fan JR L-Editor: Filipodia P-Editor: Yu HG
| 1. | Dato' P, Aziah N, Awal M, Al M, Samuri A. Child Marriage in Malaysia. 2018. [cited 13 November 2020]. Available from: http://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=117&bul_id=MDMxdHZjWTk1SjFzTzNkRXY. |
| 2. | WHO. MPS Notes: adolescent pregnancy. WHO World Health Organization; 2019. [cited 13 November 2020]. Available from: https://www.who.int/home/cms-decommissioning. |
| 3. | Kathmandu E. Nepal Demographic and Health Survey 2011 Population Division Ministry of Health and Population Government of Nepal Kathmandu, Nepal. 2012. [cited 13 November 2020]. Available from: https://dhsprogram.com/. |
| 4. | Teenage Pregnancies: Growing Challenge. New Spotlight Magazine. [cited 13 November 2020]. Available from: https://www.spotlightnepal.com/2013/11/10/teenage-pregnancies-growing-challenge/. |
| 5. | Chen XK, Wen SW, Fleming N, Demissie K, Rhoads GG, Walker M. Teenage pregnancy and adverse birth outcomes: a large population based retrospective cohort study. Int J Epidemiol. 2007;36:368-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 509] [Cited by in RCA: 514] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 6. | Smith GC, Pell JP. Teenage pregnancy and risk of adverse perinatal outcomes associated with first and second births: population based retrospective cohort study. BMJ. 2001;323:476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 148] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 7. | Poudel S, Upadhaya N, Khatri RB, Ghimire PR. Trends and factors associated with pregnancies among adolescent women in Nepal: Pooled analysis of Nepal Demographic and Health Surveys (2006, 2011 and 2016). PLoS One. 2018;13:e0202107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Nepal S, Atreya A, Kanchhan T. Teenage pregnancies in Nepal - The problem status and socio-legal concerns. J Nepal Med Assoc. 2018;56:678-682. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Trading economics. Nepal-Teenage Pregnancy And Motherhood (% Of Women Ages 15-19 Who Have Had Children Or Are Currently Pregnant): Q2 - 2006-2016 Data|2020 Forecast. [cited 29 December 2020]. Available from: https://tradingeconomics.com/nepal/teenage-pregnancy-and-motherhood-percent-of-women-ages-15-19-who-have-had-children-or-are-currently-pregnant-q2-wb-data.html. |
| 10. | Kongnyuy EJ, Nana PN, Fomulu N, Wiysonge SC, Kouam L, Doh AS. Adverse perinatal outcomes of adolescent pregnancies in Cameroon. Matern Child Health J. 2008;12:149-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Canbaz S, Sunter AT, Cetinoglu CE, Peksen Y. Obstetric outcomes of adolescent pregnancies in Turkey. Adv Ther. 2005;22:636-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Keskinoglu P, Bilgic N, Picakciefe M, Giray H, Karakus N, Gunay T. Perinatal outcomes and risk factors of Turkish adolescent mothers. J Pediatr Adolesc Gynecol. 2007;20:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Watcharaseranee N, Pinchantra P, Piyaman S. The incidence and complications of teenage pregnancy at Chonburi Hospital. J Med Assoc Thai. 2006;89 Suppl 4:S118-S123. [PubMed] |
| 14. | Kassa GM, Arowojolu AO, Odukogbe AA, Yalew AW. Prevalence and determinants of adolescent pregnancy in Africa: a systematic review and Meta-analysis. Reprod Health. 2018;15:195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 216] [Cited by in RCA: 239] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 15. | Sharma AK, Verma K, Khatri S, Kannan AT. Determinants of pregnancy in adolescents in Nepal. Indian J Pediatr. 2002;69:19-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Shrestha S. Socio-cultural factors influencing adolescent pregnancy in rural Nepal. Int J Adolesc Med Health. 2002;14:101-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Dev Raj A, Rabi B, Amudha P, Teijlingen Edwin van R, Glyn C. Factors associated with teenage pregnancy in South Asia: a systematic review. Health Sci J. 2010;. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |