Copyright
©The Author(s) 2015.
Figure 1 Dameshek 1900-1969.
Description of trilinear PV in 1950. “Photo courtesy of the American Society of Hematology (ASH) 2012.” Louis Wasserman 1912-1999. Founder of the polycythemia vera study group 1967. Photo by Jerry Soalt. “Courtesy of the ASH” 2012. William Vainchenker discoverer of the JAK2V617F mutation in 2005 as the cause of the trilinear MPNs ET, PV and MF. MF: Myelofibrosis; PV: Polycythemia vera; ET: Essential thrombocythemia; MPN: Myeloproliferative neoplasms.
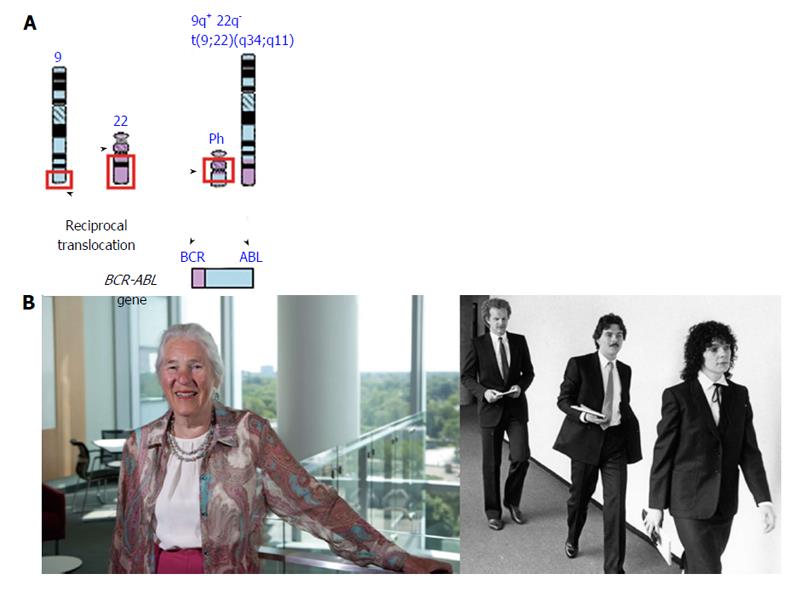
Figure 2 Reciprocal translocation t(9;22)(q34;q11) creates a novel breakpoint cluster region/ABL fusion gene with high tyrosinase activity as the cause of chronic myeloid leukemia.
A: Dr. Janet Rowley, discoverer of t(9;22)(q34;q11) in Ph1chromosome positive chronic myeloid leukemia (CML)[19,20], and winner the Beutler Prize 2011, American Society of Hematology (ASH). Photo courtesy of ASH 2012; B: The discoverers of BCR/ABL fusion gene as the cause of Ph+ CML[21-24]. From left behind to right Gerard Grosveld, John Groffen and Nora Heisterkamp.
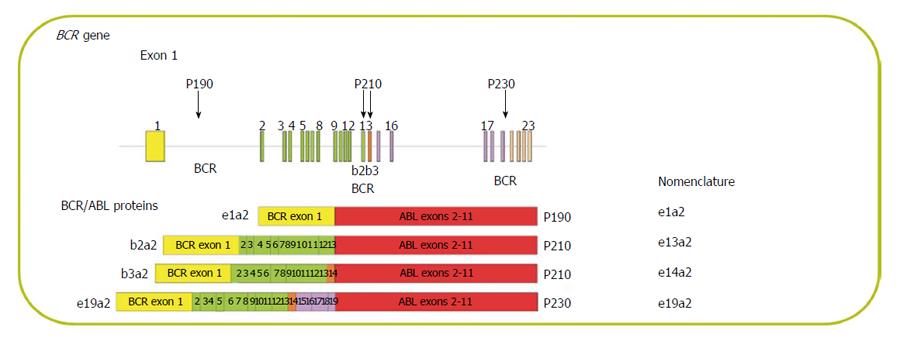
Figure 3 Locations of the breakpoint regions in the BCR gene and nomenclature of breakpoint cluster region/ABL proteins.
BCR: Breakpoint cluster region.
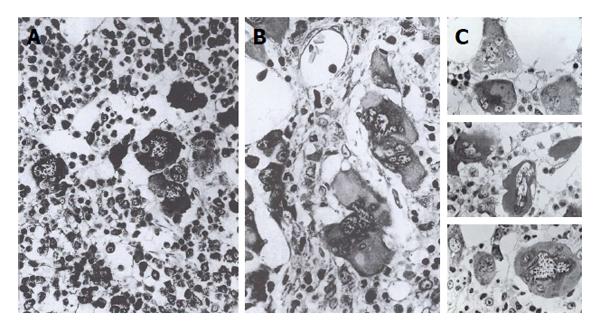
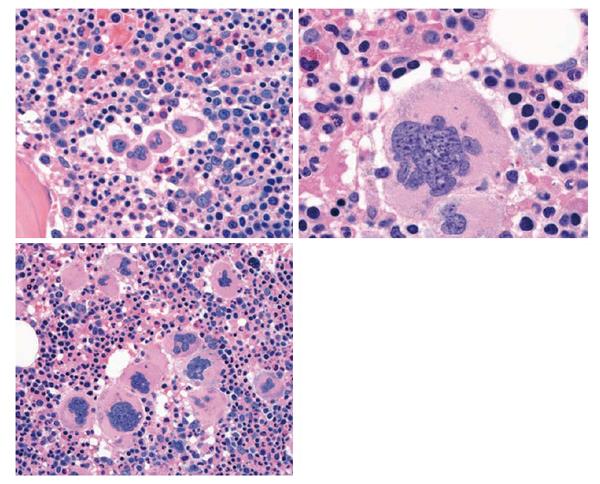
Figure 4 Cluster of medium and large immature megakaryocytes (350 × left) and large megakaryocytes with immature cytoplasm and immature clumpsy cloudlike nuclei (pseudolobulation) (right 900 ×) and very slight reticulin fibrosis in chronic megakaryocytic granulocytic myeloproliferation, and characteristics of megakaryocytes in prefibrotic myeloproliferative disorders: myeloproliferaive disease, 900 × plastic embedding.
A: Small and large and immature cloud-like nuclei in chronic megakaryocytic granulocytic myelosis or primary megakaryocytic granulocytic myeloproliferatio; B: Pleomorp large megakaryocytes in Polycythemia Vera; C: Deep hyperlobulated nuclei in essential thrombocythemia. Georgii et al[35,36].
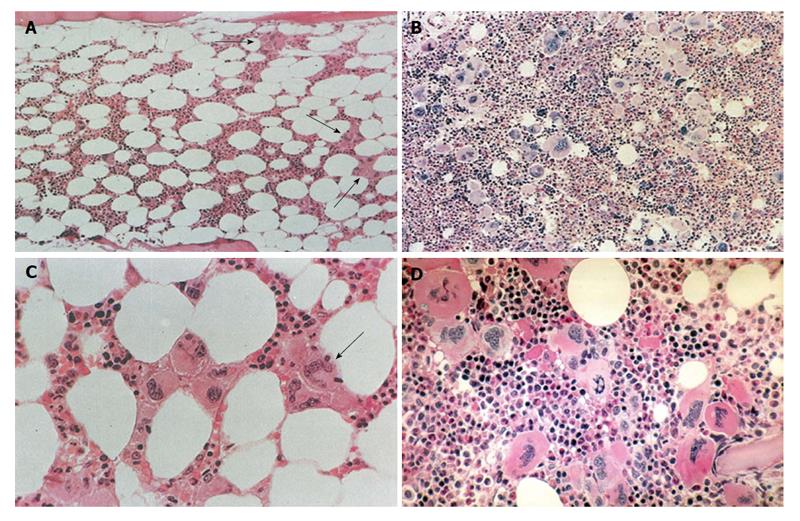
Figure 5 Spectrum of essential thrombocythemia and polycythemia vera bone marrow features in 155 bone marrow biopsies with clustered large pleomorphic megakaryocytes in polycythemia vera patients from the polycythemia vera study group 01 study.
ET bone marrow histology (A and C): arrows indicate clustered pleiomorphic megakaryocytes. PV (B) with trilinear megakaryo/eryhtro/granulocytic hyperplasia. Source Ellis et al[41] polycythemia vera study group 1975 and Wasserman et al[49]. An ET picture was observed in 10 PV. An ET/PV bone marrow picture with increased cellularity (60%-80%, D) was detected in 45 PV. A hypercellular (80%-100%, B) PV picture was recorded in 90 bone marrow biopsies of 155 PV patients the PVSG 01 study. PV: Polycythemia vera; ET: Essential thrombocythemia.
Figure 6 Presence of large platelets in peripheral blood smear (left top), increase of clustered enlarged megakaryocytes in a normocelluar essential thrombocythemia bone marrow with stainable iron (left bottom).
Local increase of erythropiesis (long arrow) in areas of loose clustered pleiomorphic megakaryoctyes in patients with normocellular essential thrombocythemia: essential thrombocythemia bone marrow histology.
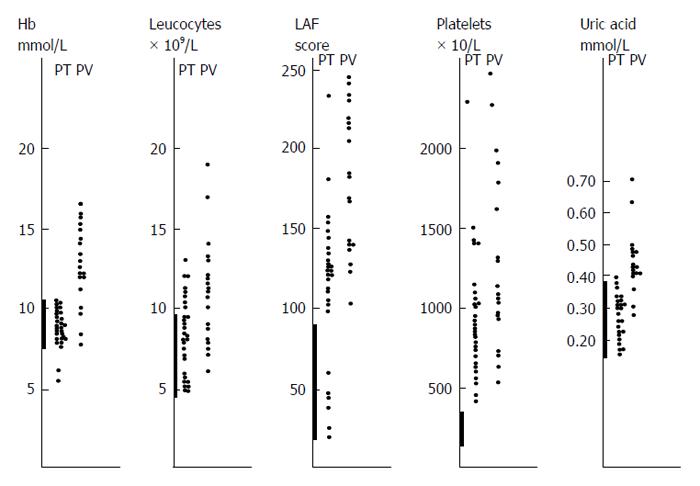
Figure 7 Laboratory findings at time of presentation in symptomatic with thrombocythemia subdivided in 30 primary thrombocythemia (= essential thrombocythemia) and 20 polycythemia vera patients seen between 1975 and 1985.
Hb levels are normal in PT and elevated in PV[16]. Leukocytes were normal or elevated in PT and PV. Leukocyte alkaline phosphatase score was much more elevated in PV than in PT with normal values in 6 PT patients. Platelet counts were were between 400 and 1000 × 10/L in the majority of the 30 PT patients. Serum uric acid levels were normal in PT and usually elevated in PV. PT: Primary thrombocythemia; LAP: Leukocyte alkaline phosphatase; PV: Polycythemia vera.
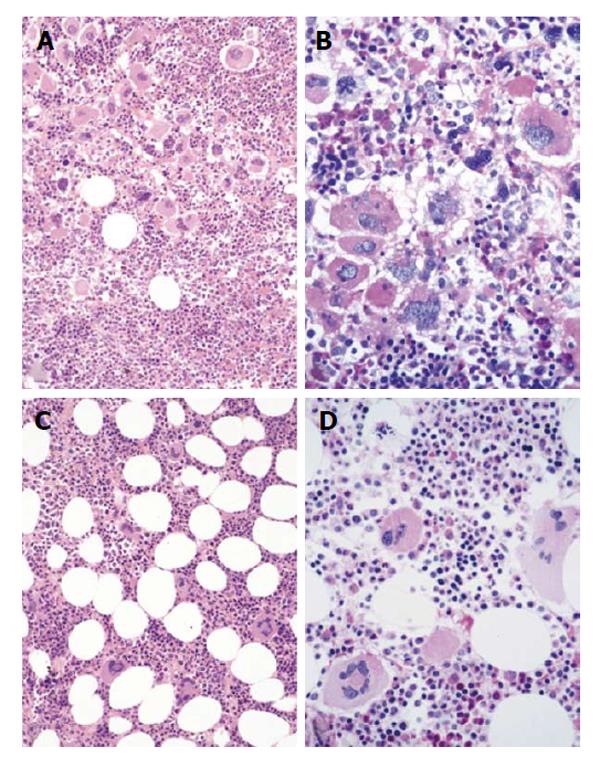
Figure 8 Hypercellular false and normocellular true essential thrombocythemia.
A and B: Hypercellular false ET or prefibrotic PMF according to Thiele (Table 6) consistent with CMGM according to Georgii et al[35] (1990), or primary megakaryocytic granulocytic myeloproliferation (PMGM122) featured by dense clustered immature megakaryopoiesis and the predominance of immature cloud-like nuclei (Kvasnicka), which are not seen in JAK2V617F positive ET and PV; C and D: Normocellular True ET (World Health Organization-ET, Table 5) according to Thiele and Michiels 1988-2006[59,62,107] with the presence of large to giant megakaryocytes larger than in JAK2V617F positive ET and PV. True ET as defined by Thiele seems to our experience most consistent with normocellular JAK2 wild type ET carrying the MPL515 mutation featured by clustered large and giant megakaryocytes in a normocellular bone marrow, which usually runs a very benign course. ET: Essential thrombocythemia; PV: Polycythemia vera; CMGM: Chronic megakaryocytic granulocytic myeloproliferation.
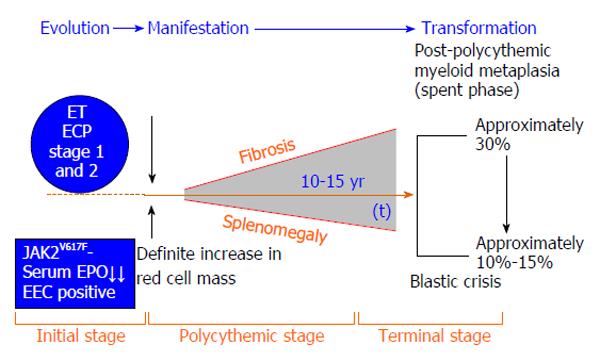
Figure 9 Prodromal polycythemia vera with normal red cell mass (red cell mass, Tables 3 and 7) and erythrocytes (< 6 × 1012/L, Tables 8 and 9), prefibrotic idiopathic erythrocythemia and polycythemia vera with increased erythrocytes (> 6 × 1012/L) and red cell mass, and evolution into masked PV with splenoegaly, spent phase polycythemia vera with myelofibrosis (Table 12) and post-polycythemia vera-myelofibrosis according to European Clinical and Pathological criteria defined by Michiels and Thiele (http://www.mpn-stichting.nl/doctors_brochure_2004.pdf) and according to the 2006-2007 World Health Organization-European Clinical Molecular and Pathological criteria for JAK2 mutated stages of prodromal overt and advanced polycythemia vera[71-73].
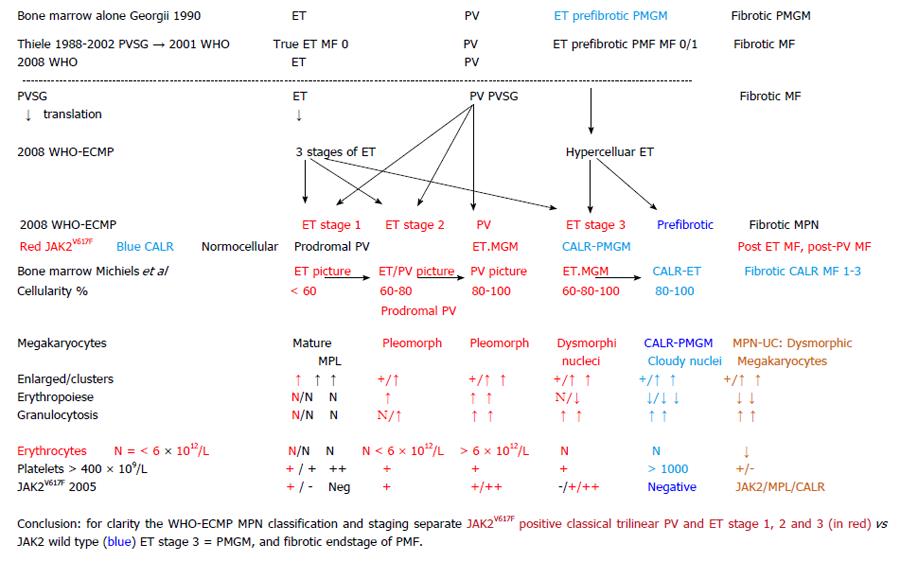
Figure 10 Charaterization of polycythemia vera study group defined essential thrombocythemia and polycythemia vera by applying the 2006 European Clinical Molecular and Pathological criteria and 2001 World Health Organization bone marrow features; JAK2V617F mutated normocellular essential thrombocythemia, prodromal polycythemia vera, classical polycythemia vera and myelofibrosis vs JAK2 wild type normocelluar essential thrombocythemia and chronic idiopathic myelofibrosis or Primary megakaryocytic granulocytic myeloproliferation.
WHO: World Health Organization; PV: Polycythemia vera; ECMP: European clinical molecular and pathological; MF: Myelofibrosis; ET: Essential thrombocythemia; MPN: Myeloproliferative neoplasm; PMGM: Primary megakaryocytic granulocytic myeloproliferation; PVSG: Polycythemia vera study group; CALR: Calreticulin.
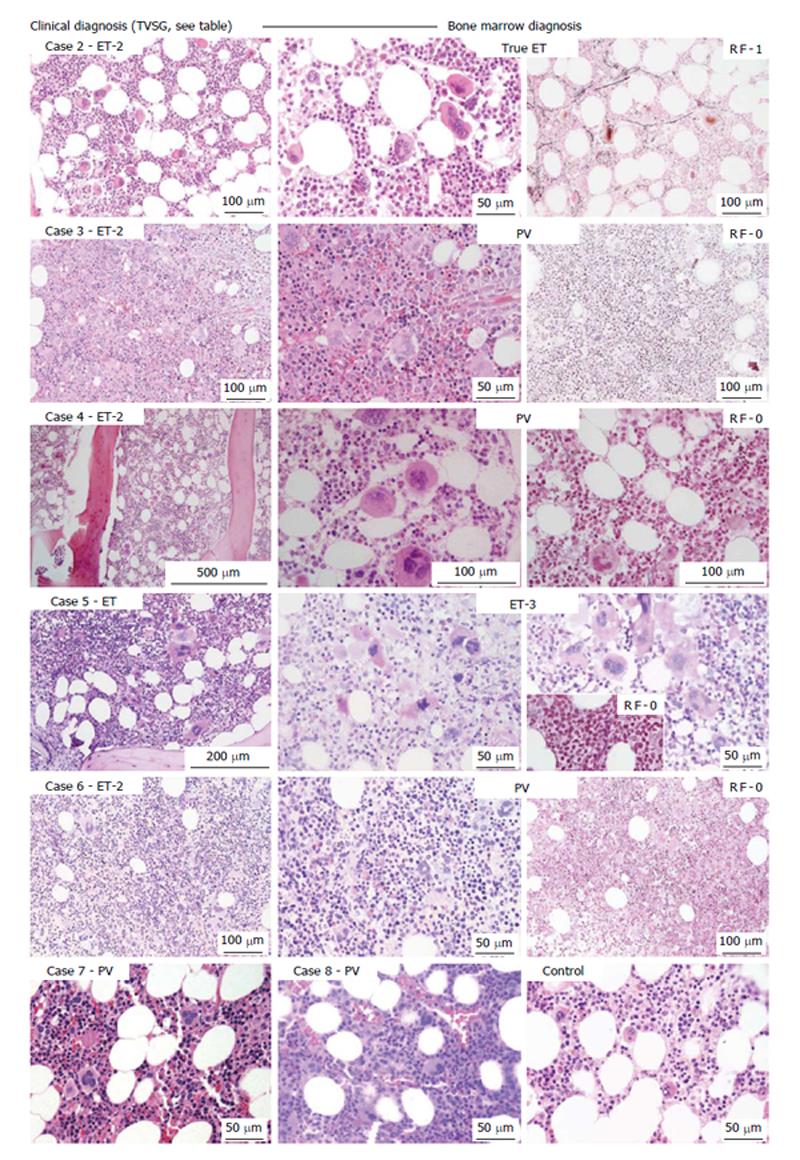
Figure 11 The clinical features of four JAK2V617F+ essential thrombocythemia and two JAK2V617F+ polycythemia vera cases refer to the numbering of cases in Figure 10.
Case 2: Clinically JAK2V617F ET 2 (low serum erythropoetin) and a normocellular ET [World Health Organization (WHO)-ET] bone marrow wit pleomorph small and large megakaryocytes and reticulin fibers (RF) grade 1; Case 3 and 4: Clinically JAK2V617F ET 2 with a trilinear hypercellular PV bone marrow and RF 0 in case 3: ET 2 with increased cellularity due to increased erythropoiesis RF grade 0 in case 4; Case 5: Clinically JAK2V617F ET with moderate splenomegaly and a hypercellular megakaryocytic granulocytic myeloproliferation (ET.MGM = ET 3), with dysmorphic megakaryocytes (not cloud-like) and RF grade 0 in case 5; Case 6: Clinically JAK2V617F ET 2 with a trilinear PV bone marrow picture1 and RF grade 0; Case 7: Clinically JAK2V617F PV with a 65% hypercellular ET/PV bone marrow picture in between “normocellular ET” (WHO-ET) and trilinear hypercellular (90%-100%) PV picture in case 7 and 8 with PV with increased RCM and erythrocytes above 6 × 1012/L. In 2007, we concluded that bone histology alone does not differentiate between JAK2 mutated ET and PV, as compared to control, morphology of pleiomorph megakaryocytes in JAK2V617F mutated ET and PV are similar Source Poster P-0025. Fourth International Congress on myeloproliferaive disease/myelodysplatic syndrome New York, 2007. ET: Essential thrombocythemia; PV: Polycythemia vera.
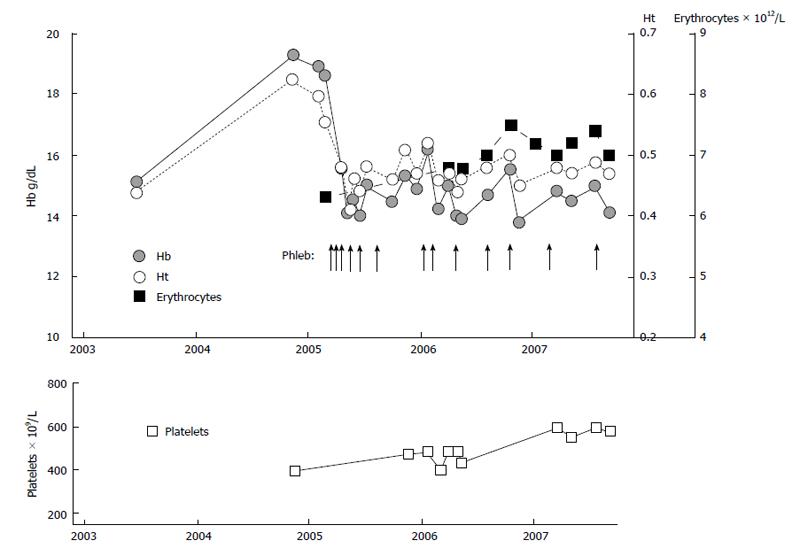
Figure 12 Sequential stages of essential thrombocythemia 1995-2004, prodromal polycythemia vera 2004-2005 and overt polycythemia vera 2006, with a complete hematological response (complete hematological responses, case 6, Table 9, Figure 11) and subsequent complete hematological responses of interferon for 6 years at age of 72 years anno 2013.
Figure 13 Clinical course in case 8 (Table 9, Figure 11) with erythrocythemic polycythemia vera treated with venesections (arrows).
The development of microcytic hypochromic erythrocytes due to iron deficiency was associated with persistent increased red cell count (> 6 × 1012/L), which is diagnostic for polycythemia vera. The iron deficient state and the low normal values for haemoglobin (Hb) and hematocrit (Ht) was associated with relief of hypervolumic symptoms with phlebotomy on top of low dose aspirin.
Figure 14 Genotype of individual BFU-E in polycythemia vera and essential thrombocythemia with granulocytes heterozygous for the JAK2V617F mutation (less than 50% JAK2V617F mutation load) show that polycythemia vera patients are heterozygous/homozygous and essential thrombocythemia patients heterozygous for the JAK2V617F somatic mutation.
ET: Essential thrombocythemia; PV: Polycythemia vera; WT: Wild type; BFU-e: Burst forming units erythropoiesis.
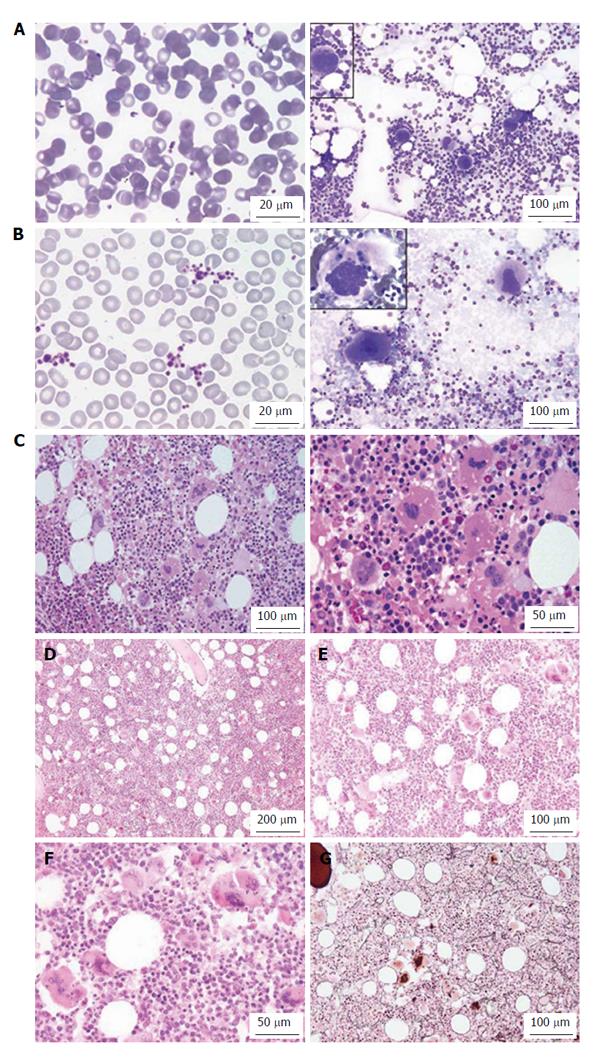
Figure 15 Bone marrow histology in JAK2 exon 12 polycythemia vera.
Figure 16 JAK2V617F positive hypercellular essential thrombocythemia (platelets 453 × 109/L) in a case of portal vein thrombosis[94].
Large platelets in peripheral blood smear (B left) as compared to control (A left), bone marrow smear with large megakaryocytes with multilobulated nuclei (B right) as compared to control (A right) and hypercellular bone marrow due to increased erythropoisesis and granulopoiesis with pleomorphic megakaryocytes (C-E) similar as in typical polycythemia vera case 9 (F) with a hypercellular bone marrow picture due to increased erythropoiesis and granulopoiesis and slight increase of reticuline fibers grade 1 (G).
Figure 17 Bone marrow histology in normocellular essential thrombocythemia carrying the MPLW515L mutation showing giant megakaryocytes with hyperlobulated stag-horn like nuclei charateristic for essential thrombocythemia the MPLW515L/K mutation.
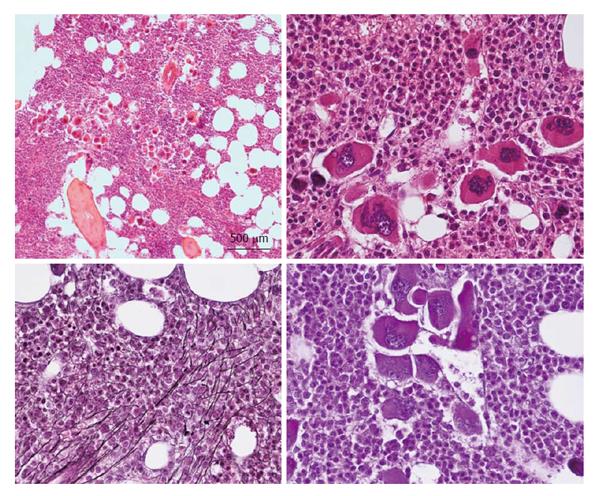
Figure 18 Clinical case of JAK2/MPL negative and calcireticulin positie essential thrombocythemia who present with aspirin responsive platelet thrombophilia, normal values for hemoglobin.
Hematocrit and erythrocytes, platelet count of 1832 × 109/L and slight splenomegaly (16 cm lenght diameter on echogram). Bone marrow histology is hypercellular with relative decrease of erythropoisis, dense cluster of immature megakaryocytes with hypolobulated nuclei consistent, and no increase of reticulin fibrosis consistent with a typical primary megakaryocytic granulocytic myeloproliferation (Table 10) bone marrow.
Figure 19 Clinical case of calcireticulin positive myelofibrosis: Hemoglobin 11.
2 g/dL, hematocrit 0.33, leukocytes 9.2 × 109/L, platelets 347 × 109/L, lactodehydrogenase 1393 U/L, and the presence of tear drop erythrocytes, poikolocytosis and polychromasie in a peripheral bloodsmear, and hypercellular bone marrow with relative decrease of erythropoisis, dense cluster of immature megakaryocytes with hypolobulated nuclei consistent, and reticulin fibrosis grade 2 consistent with bone marrow histology features similar to World Health Organization-defined primary myelofibrosis, but distinct from JAK2V617F mutated essential thrombocythemia and polycythemia vera, and distinct from MPL515 mutated essential thrombocythemia (Figures 17).
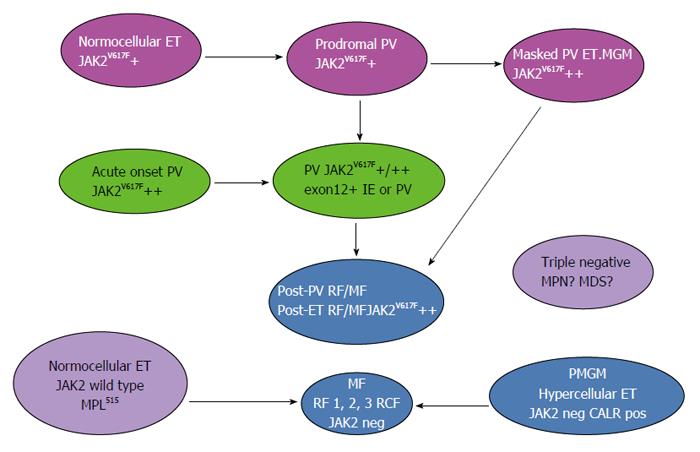
Figure 20 World Health Organization-clinical molecular and pathological myeloproliferative neoplasms classification and transitional states.
ET: Essential thrombocythemia; PV: Polycythemia vera; MGM: Megakaryocytic granulocytic myeloproliferation; IE: Idiopathic erythrocythemia; RF: Reticulin fibrosis; MF: Myelofibrosis; RCF: Reticulin collagen fibrosis; CALR: Calreticulin; PMGM: Primary megakaryocytic granulocytic myeloproliferation.
-
Citation: Michiels JJ, Valster F, Wielenga J, Schelfout K, Raeve HD. European
vs 2015-World Health Organization clinical molecular and pathological classification of myeloproliferative neoplasms. World J Hematol 2015; 4(3): 16-53 - URL: https://www.wjgnet.com/2218-6204/full/v4/i3/16.htm
- DOI: https://dx.doi.org/10.5315/wjh.v4.i3.16