Published online May 24, 2022. doi: 10.5306/wjco.v13.i5.366
Peer-review started: January 18, 2022
First decision: February 15, 2022
Revised: February 28, 2022
Accepted: May 7, 2022
Article in press: May 7, 2022
Published online: May 24, 2022
Laparoscopic pancreaticoenteric anastomosis is one of the technically challenging steps of minimally invasive pancreaticoduodenectomy (PD), especially during the learning curve. Despite multiple randomized controlled trials and meta-analyses, the type of pancreatico-enteric anastomosis as a risk factor for post-pancreatectomy complications is debatable. Also, the ideal technique of pancreatic reconstruction during the learning curve of laparoscopic PD has not been well studied.
To compare the short-term outcomes of modified binding pancreaticogastrostomy (PG) and Blumgart pancreaticojejunostomy (PJ) during learning curve of laparoscopic PD.
The first 25 patients with resectable pancreatic or periampullary tumors who underwent laparoscopic PD with modified binding PG or modified Blumgart PJ between January 2015 and May 2020 were retrospectively analyzed to compare perioperative outcomes during the same learning curve. A single layer of the full-thickness purse-string suture was placed around the posterior gastrotomy in the modified binding PG. In the modified Blumgart technique, only a single transpancreatic horizontal mattress suture was placed on either side of the pancreatic duct (total two sutures) to secure the pancreatic parenchyma to the jejunum. Also, on the ventral surface, the knot is tied on the jejunal wall without going through the pancreatic parenchyma. Post pancreatectomy complications are graded as per the International Study Group for Pancreatic Surgery criteria.
During the study period, modified binding PG was performed in 27 patients and modified Blumgart PJ in 29 patients. The demographic and clinical parameters of the first 25 patients included in both groups were comparable. Lower end cholangiocarcinoma and ampullary adenocarcinoma were the primary indications for laparoscopic PD in both groups (32/50, 64%). The median operative time for pancreatic reconstruction was significantly lower in the binding PG group (42 vs 58 min, P = 0.01). The clinically relevant (Grade B/C) postoperative pancreatic fistula (POPF) was significantly more in the modified PJ group (28% vs 4%, P = 0.04). In contrast, intraluminal postpancreatectomy hemorrhage (PPH) was more in the binding PG group (32% vs 4%, P = 0.02). There was no significant difference in the incidence of delayed gastric emptying between the two groups.
During the learning curve of laparoscopic PD, modified binding PG reduces POPF but is associated with increased intraluminal PPH compared to PJ using the modified Blumgart technique.
Core Tip: During the learning curve of laparoscopic pancreaticoduodenectomy, modified binding pancreaticogastrostomy reduces the operative time for pancreatic reconstruction. Also, modified binding pancreaticogastrostomy reduces clinically relevant postoperative pancreatic fistula compared to modified Blumgart pancreaticojejunostomy. However, modified binding pancreaticogastrostomy is associated with increased intraluminal postpancreatectomy hemorrhage. The present study results could guide surgeons to tailor the pancreatic reconstruction during the learning curve of laparoscopic pancreaticoduodenectomy.
- Citation: Choudhury SR, Kalayarasan R, Gnanasekaran S, Pottakkat B. Modified binding pancreaticogastrostomy vs modified Blumgart pancreaticojejunostomy after laparoscopic pancreaticoduodenectomy for pancreatic or periampullary tumors. World J Clin Oncol 2022; 13(5): 366-375
- URL: https://www.wjgnet.com/2218-4333/full/v13/i5/366.htm
- DOI: https://dx.doi.org/10.5306/wjco.v13.i5.366
Laparoscopic pancreaticoduodenectomy (PD) is considered one of the most complex minimal access surgical procedures, requiring proficiency in advanced laparoscopic surgery. With advancements in laparoscopic skills and technology, multiple studies have reported the feasibility, safety, and oncological equivalence of Laparoscopic PD compared to open PD[1-3]. Despite improved surgical techniques and perioperative management, PD remains a morbid procedure with a 30%-50% estimated morbidity rate[4]. As in open PD, pancreatico-enteric anastomosis remains the Achilles’ heel in laparoscopic PD, and postoperative pancreatic fistula (POPF) is the critical cause of morbidity in these patients. The type of pancreatico-enteric anastomosis as a risk factor for POPF is still debatable. Multiple retrospective studies, some randomized controlled trials (RCTs), and meta-analyses have reported that pancreaticogastrostomy (PG) is associated with less incidence of POPF compared to pancreaticojejunostomy (PJ)[5,6]. However, other RCTs and meta-analyses did not report any difference between the two anastomotic techniques concerning clinically relevant POPF rates[7,8].
In laparoscopic PD, in addition to conventional risk factors for POPF, laparoscopic instruments’ restricted range of motion poses an additional risk, especially during the learning curve. A review of various techniques of laparoscopic pancreatic reconstruction following laparoscopic PD reported that PJ was more commonly used than PG like open PD[9]. However, to date, no RCT has compared different techniques of pancreatic reconstruction in laparoscopic PD, precluding a definite conclusion. The ideal method of managing remnant pancreas following laparoscopic PD should be safe and easy to perform, especially during the learning curve. In open PD, binding PG using two layers of purse-string sutures has been described as a safe and technically simpler method of pancreatic reconstruction[10,11]. Of the many techniques of PJ, the Blumgart method of PJ is a popular one, and its safety has been established in multiple open PD series[12-14]. However, the outcomes of these techniques of pancreatic reconstruction during the learning curve of Laparoscopic PD have not been previously studied. We used the binding PG and Blumgart method of PJ that was modified to suit the laparoscopic pancreatic reconstruction[12,15]. The present study compares the short-term outcomes of modified binding PG and Blumgart technique of PJ for pancreatic reconstruction in laparoscopic PD during the learning curve.
Laparoscopic PD was started in the institute in January 2015. Until October 2017, modified binding PG was used for pancreatic reconstruction in laparoscopic PD. Subsequently, the modified Blumgart technique was mainly used for pancreatic reconstruction, except in patients whose pancreatic duct could not be identified after pancreatic transection, where invagination PJ or binding PG was used. Clinical data of the first 25 patients with resectable pancreatic and periampullary tumors who underwent laparoscopic PD with modified binding PG or modified Blumgart PJ between January 2015 and May 2020 were retrospectively analyzed to evaluate the outcomes during the same learning curve. Pancreatic cancer patients with suspected vascular involvement and those with contraindications for laparoscopic surgery were not considered for laparoscopic PD. Patients who underwent laparoscopic PD with different techniques of pancreatic reconstruction and those who underwent robotic PD were excluded from the analysis. Also, patients who underwent laparoscopic PD for chronic pancreatitis or other nonmalignant etiology were not included in the study. All surgeries were performed by a single surgeon (RK) with sufficient experience in advanced minimally invasive gastrointestinal surgery. The study was approved by the institute scientific advisory committee (PGRMC 19.04.2021-18) and the institute ethics committee (JIP/IEC/2021/0194).
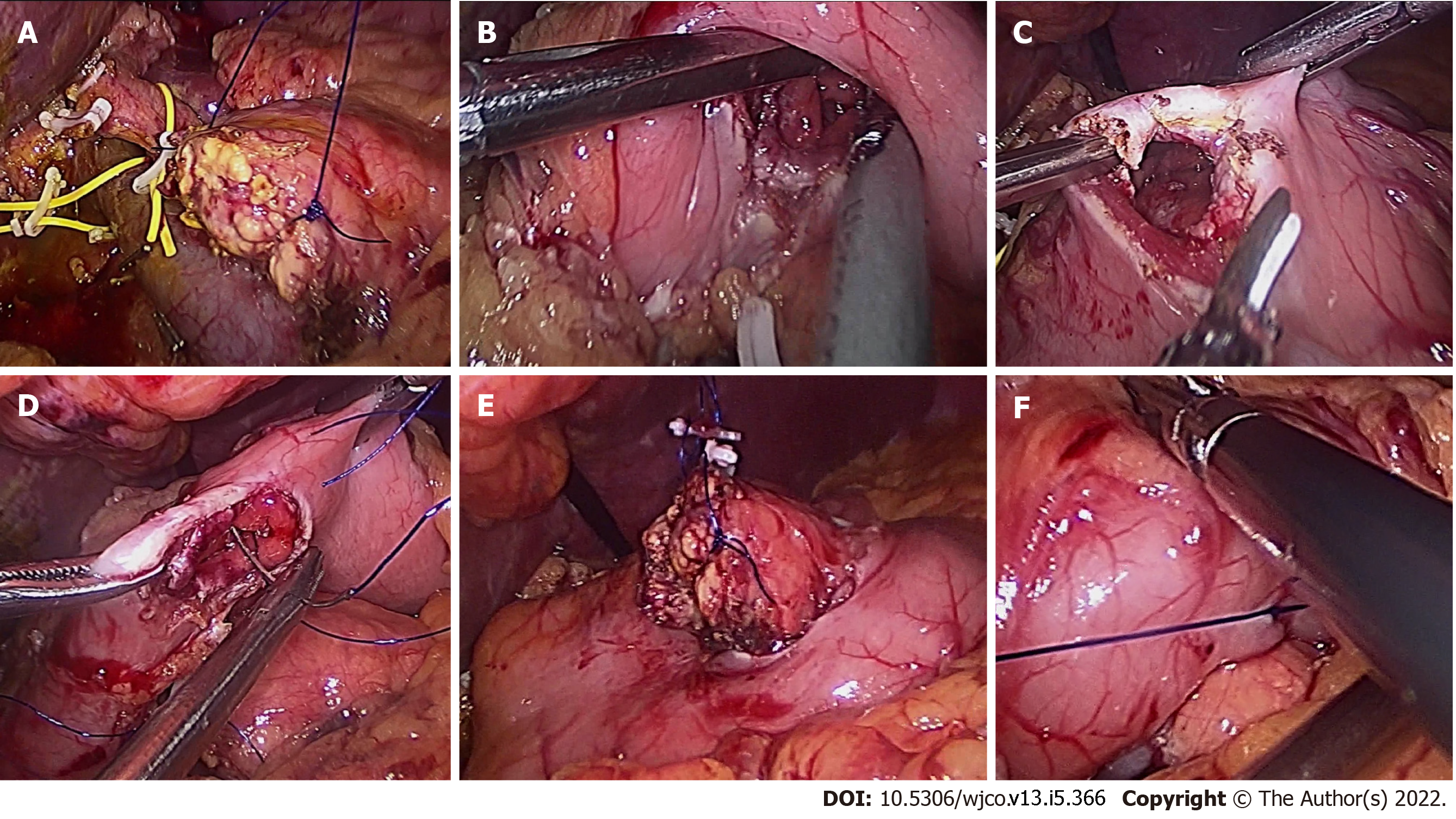
The procedure was performed using six laparoscopic ports: One infra umbilical 12 mm port, two 12 mm pararectal ports, one left subcostal 12 mm port, one right subcostal 5 mm port, and one 5 mm epigastric port with the patient in French position (supine with leg split). The infraumbilical port is used for laparoscopic camera except during uncinate dissection when the camera is moved to the right pararectal port. For ligation and division of gastrocolic trunk, division of stomach, lymph node dissection in hepatoduodenal ligament, and bile duct division, the two 12 mm ports on the left side are used as primary working ports with the surgeon standing on the left side of the patient. The primary surgeon moves to the patient’s right side for the remaining dissection. The two right-sided ports are used as a primary working port for the pancreatic reconstruction using modified binding PG. Two full-thickness stay sutures are taken at the corners of the pancreatic cut surface using 3-0 polypropylene to facilitate pancreatic mobilization and invagination into the stomach (Figure 1). The pancreas is carefully mobilized from the splenic vein and artery after sealing and dividing small vessels for approximately 3-4 cm. The left gastric vein that usually drains to the splenic portal vein junction should be identified during pancreatic mobilization to avoid inadvertent injury and troublesome bleeding. Anterior gastrotomy of length approximately 4-5 cm was made proximal to the stapled end of the stomach. A posterior gastrotomy was made at a site where the pancreas can be invaginated without undue tension for a length approximately equivalent to the width of the pancreatic cut surface. In contrast to the original technique of binding PG that used two layers (inner mucosal and outer seromuscular) of purse-string sutures, the modified binding PG technique utilizes only a single layer of a full-thickness purse-string suture[10,15]. The modified binding PG technique used in the current series was adapted from the publication by Hong et al[15] that reported the feasibility of binding PG using a single layer of the full thickness purse-string suture in 10 patients undergoing laparoscopic central pancreatectomy. The placement of the purse-string suture using 3-0 polypropylene should start from the superior edge of the posterior gastrotomy to ensure adequate visualization of knots after invagination of the pancreas. The pancreas was lifted using the stay sutures and invaginated into the stomach through posterior gastrotomy. The stay sutures are held with a laparoscopic grasper advanced through anterior gastrotomy. Once the invagination of at least 2 cm of the pancreas into the stomach was confirmed, the stay suture is tied to bind the gastric wall to the pancreatic stump. The position of the pancreas inside the stomach was rechecked after completion of the hepaticojejunostomy to ensure a tension-free anastomosis. An anterior gastrotomy was used for hand sewn gastrojejunostomy.
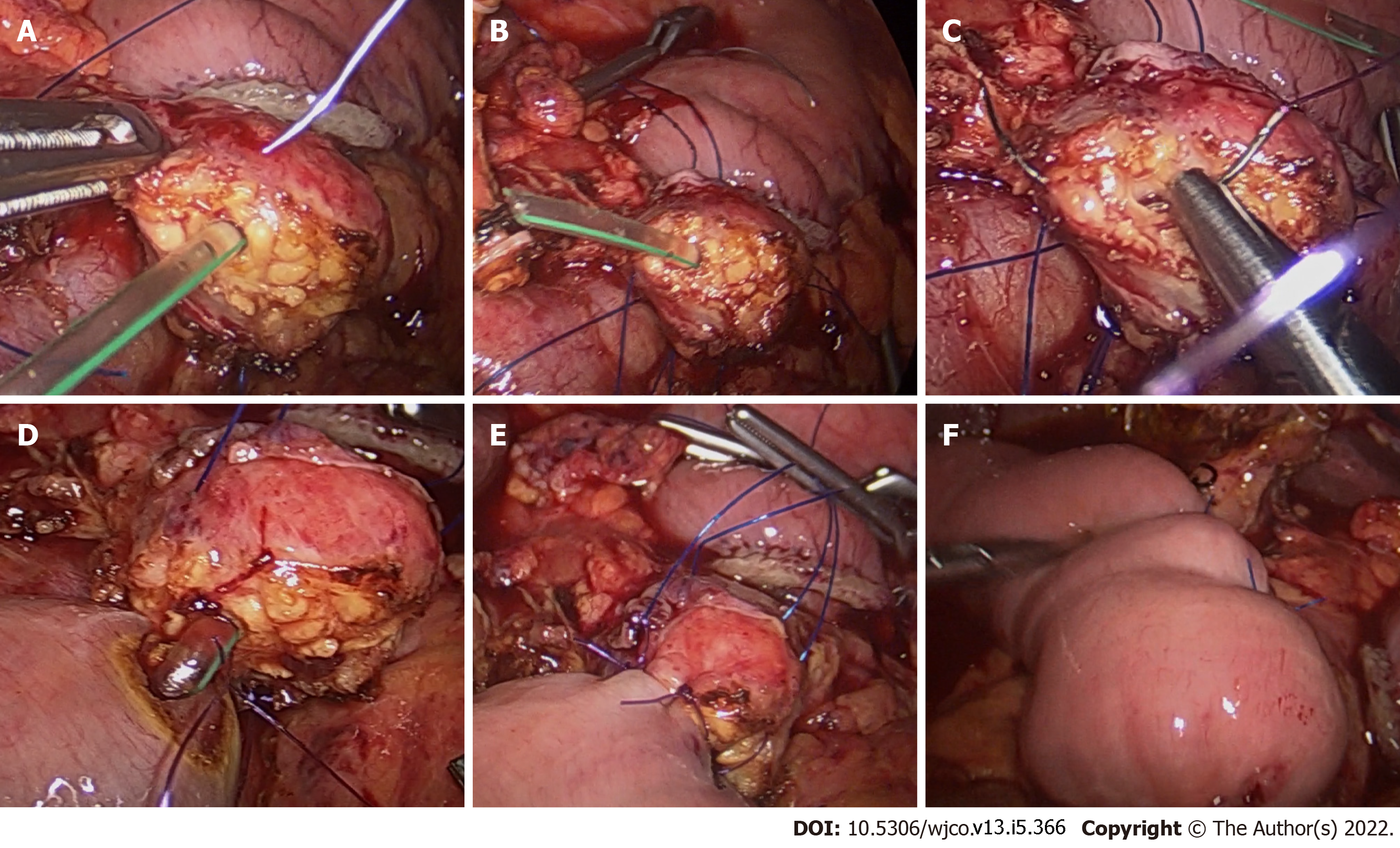
For PJ using the modified Blumgart technique, the surgeon stands between the patient’s legs and uses the infraumbilical and right subcostal ports as working ports. The laparoscopic camera was inserted through the right pararectal port. In the original Blumgart technique, two to three transpancreatic full-thickness U-shaped sutures were placed on either side of the pancreatic duct[16]. In the modified technique, a single transpancreatic horizontal mattress suture was placed on either side of the pancreatic duct (total two sutures) to secure the pancreatic parenchyma to the jejunum (Figure 2). The modified Blumgart PJ used in the present series was based on the previous studies in open PD that reported the advantages of using fewer transpancreatic sutures to minimize the risk of pancreatic juice leakage[12,14]. The 26 mm ½ circle round body needle of 3-0 polypropylene suture was straightened to facilitate the placement of transpancreatic suture. For duct to mucosa anastomosis, six interrupted 4-0 PDS sutures are placed at 4, 6, 8, 10, 12, and 2o’clock position. The needle moves in-out direction in the ductal end to ensure accurate placement of pancreatic duct sutures. In-out needle movement was facilitated by taking the initial bite in the pancreatic duct for 4, 6, and 8 o’clock sutures. For the remaining sutures, the initial bite was taken in the jejunal end. The pancreatic duct stent was placed after knotting the 6 and 8o’clock sutures. However, the stent was not fixed with sutures. After knotting the remaining duct to mucosa sutures, the transpancreatic suture needle was used to take a seromuscular bite on the antimesenteric edge of the jejunum. Ligation of these sutures wraps the ventral portion of the pancreatic cut edge with the jejunum. In contrast to the original Blumgart technique, no suture was taken on the anterior surface of the pancreas. A feeding jejunostomy was routinely performed in all patients undergoing laparoscopic PD.
The patients’ demographic and clinical data, including age, sex, body mass index, bilirubin level, preoperative biliary drainage, total operative time, time taken for pancreatic reconstruction, estimated blood loss, need for blood transfusions, fistula risk score, and tumor type, were reviewed and compared between the two groups[17]. Postoperative morbidity was graded as per Clavien-Dindo classification[18]. Delayed gastric emptying [DGE], postpancreatectomy hemorrhage (PPH), and postoperative pancreatic fistula [POPF] were graded as per the International Study Group for Pancreatic Surgery [ISGPS] definition[19-21]. Postoperative mortality is defined as any death, regardless of cause, occurring within 90 d after surgery in or out of the hospital.
Continuous variables were expressed as the median with range. Categorical variables were expressed as proportions. Continuous variables were analyzed using the Mann-Whitney U test. Categorical variables were analyzed using the chi-square test or Fisher’s exact test. A P value of less than 0.05 was considered statistically significant. All analyses were performed using IBM SPSS Statistics for Windows, Version 28.0. (Armonk, NY: IBM Corp).
During the study period, 78 patients underwent minimally invasive PD. Of these, 22 patients [Robotic PD (n = 18), nonmalignant etiology (n = 2), invagination PJ (n = 2)] who did not meet the inclusion criteria were excluded from the analysis. Overall, modified binding PG was performed in 27 patients and modified Blumgart PJ in 29 patients. To evaluate the short-term outcomes during the learning curve of laparoscopic PD, the first 25 consecutive patients who underwent modified binding PG and modified Blumgart PJ were included in the study.
The demographic and clinical parameters between the two groups were comparable (Table 1). Both groups had lower end cholangiocarcinoma and ampullary adenocarcinoma as the primary indications for laparoscopic PD (32/50, 64%). Hence, most patients had jaundice (43/50, 86%) at presentation. All 3 patients with intraductal papillary mucinous neoplasm had the main duct type of tumor. Of the 3 patients with neuroendocrine tumor, 1 patient had an ampullary tumor, and the other 2 had cancer in the head and uncinate process of the pancreas.
| Variable | Binding PG group, n = 25 | Modified Blumgart PJ group, n = 25 | P value |
| Age in yr, median (range) | 53.7 (37-75) | 58.2 (31-79) | 0.12 |
| Sex, Male:Female | 14:11 | 15:10 | > 0.99 |
| BMI in kg/m2, median (range) | 23.8 (17.6-41.6) | 24.6 (18.2-40.0) | 0.69 |
| Jaundice, n (%) | 22 (88) | 21 (84) | > 0.99 |
| Cholangitis, n (%) | 8 (32) | 5 (20) | 0.52 |
| Peak total bilirubin levels in mg/dL, median (range) | 12.8 (1.2-28.3) | 10.6 (1.1-31.2) | 0.59 |
| Preoperative biliary drainage, n (%) | 14 (56) | 12 (48) | 0.78 |
| CA 19-9 (U/mL), median (range) | 55 (1-5682) | 84 (2-3318) | 0.12 |
| Diagnosis, n (%) | |||
| Cholangiocarcinoma | 9 (36) | 7 (28) | 0.76 |
| Pancreatic adenocarcinoma | 3 (12) | 2 (8) | > 0.99 |
| Ampullary adenocarcinoma | 7 (28) | 9 (36) | 0.76 |
| Duodenal adenocarcinoma | 3 (12) | 4 (16) | > 0.99 |
| Intraductal papillary mucinous | 2 (8) | 1 (4) | > 0.99 |
| Neoplasm pancreas | |||
| Neuroendocrine tumor | 1 (4) | 2 (8) | > 0.99 |
There was no significant difference in the total operative time and estimated blood loss between the two groups (Table 2). However, the median time to perform modified binding PG was significantly less than modified Blumgart PJ. While most patients had intermediate or high fistula risk scores (38/50, 76%), the proportion was not significantly different between the two groups. However, the modified binding PG group had a significantly lesser number of patients with Grade B/C POPF. None of the patients required reoperation for POPF. Overall, 9 patients had PPH (Grade A-3, Grade B-5, Grade C-1). The proportion of patients with PPH was significantly more in the modified binding PG group. On the fifth postoperative day, 1 patient in the binding PG group was reoperated in an emergency due to severe upper gastrointestinal bleeding that manifested as hematemesis. To visualize the pancreatic stump, an anterior gastrotomy was made away from the gastrojejunostomy site. After evacuating the clots in the gastric lumen, an arterial bleeder in the inferior edge of the pancreatic stump was suture ligated. DGE was present in 13 patients (Grade A-7, Grade B-4, Grade C-2). However, there was no significant difference in the rate of DGE between the two groups. There was no postoperative mortality in both groups.
| Variable | Binding PG group, n = 25 | Modified Blumgart PJ group, n = 25 | P value |
| Total operative time in min, median (range) | 445 (390-710) | 405 (330-670) | 0.06 |
| Operative time for pancreatic reconstruction in min, median (range) | 42 (26-65) | 58 (44-81) | 0.01 |
| Estimated blood loss in mL, median (range) | 320 (210-740) | 310 (175-950) | 0.09 |
| Blood Transfusion, n (%) | 6 (24) | 7 (28) | > 0.99 |
| Gland texture, n (%) | |||
| Soft | 17 (68) | 19 (76) | 0.75 |
| Firm | 8 (32) | 6 (24) | |
| Pancreatic duct diameter in mm, median (range) | 3 (1-9) | 3 (2-10) | > 0.99 |
| Fistula risk score, n (%) | |||
| Low | 5 (20) | 7 (28) | 0.74 |
| Intermediate | 12 (48) | 13 (52) | > 0.99 |
| High | 8 (32) | 5 (20) | 0.52 |
| Postoperative morbidity, Clavien-Dindo classification IIIa or more, n (%) | 8 (32) | 9 (36) | > 0.99 |
| Pancreatic fistula as Grade B/C, n (%) | 1 (4) | 7 (28) | 0.04 |
| Delayed gastric emptying, n (%) | 7(28) | 6 (24) | > 0.99 |
| Post pancreatectomy hemorrhage, n (%) | 8 (32) | 1 (4) | 0.02 |
| Bile leak, n (%) | 0 | 1 (4) | > 0.99 |
| Postoperative hospital stay in days, median (range) | 9 (6-38) | 8 (5-56) | 0.72 |
The present study results suggest that during the learning curve of laparoscopic PD, modified binding PG reduces POPF but is associated with increased intraluminal PPH compared to PJ using the modified Blumgart technique. The feasibility, safety, and oncological outcomes of laparoscopic PD have been documented in multiple retrospective series and a few single-center prospective trials[1-3]. However, the multicenter randomized trial (LEOPARD-2) comparing laparoscopic with open PD was prematurely terminated because of higher complication-related mortality in the laparoscopic group[22]. As in open PD, pancreatico-enteric anastomosis is the critical cause of morbidity and mortality in patients undergoing laparoscopic PD, especially during the learning curve in low and medium volume centers[4,22]. While the learning curve for laparoscopic PD has not been well studied, a few single-center studies have suggested that operative time and complications stabilize after 30-42 procedures[23-25]. Hence, in the present study, the perioperative outcomes of the first 25 laparoscopic procedures are compared.
The type of pancreatico-enteric anastomosis as a risk factor for POPF is still controversial. While a few RCTs and meta-analyses have documented the benefits of PG in reducing POPF, others did not find any difference between the two anastomotic techniques[5-8]. The ideal pancreatic reconstruction technique during the learning curve of laparoscopic PD should be safe and easy to perform. The binding technique for pancreatoenteric anastomosis was described by Peng et al[26] based on the hypothesis that avoiding pancreatic sutures at the level of the anastomosis can minimize POPF. Initially, he described binding PJ with an excellent postoperative outcome[26]. However, binding PJ cannot be used when the pancreatic stump is too large to be invaginated into the jejunum. Hence, binding PG was developed in which the pancreatic stump was invaginated into the stomach and held in place by two purse-string sutures: an outer seromuscular and inner mucosal purse-string suture[10]. Despite encouraging outcomes with binding PG in open PD, its safety and feasibility have not been well studied in laparoscopic PD. Wakabayashi et al[27] reported the feasibility of double purse-string suture PG in robotic PD as a technical report. In the present study, only a single layer of the full-thickness purse-string suture was used that was adapted from the previous report on the feasibility of binding PG using a single layer of the full thickness purse-string suture in patients undergoing laparoscopic central pancreatectomy[28]. The efficacy of the Blumgart technique in reducing the POPF rate has been documented in multiple open PD series[29,30]. The transpancreatic, full-thickness, mattress U-sutures used in the Blumgart technique reduce the tangential tension and shear force at the pancreatic stump. However, more sutures on the pancreas increase the POPF risk[31]. Another potential risk with the original Blumgart technique is excessive compression on the pancreas while tying the transpancreatic sutures. Hence, only two transpancreatic U sutures were used in the present technique. Also, on the ventral surface, only a seromuscular bite was taken on the jejunum without taking any suture on the anterior surface of the pancreas to reduce shear force and excessive compression of the pancreatic parenchyma.
The perioperative outcomes of the modified binding PG and modified Blumgart technique of PJ have not been previously compared in the laparoscopic approach. As documented in the present study, modified binding PG can minimize the pancreatic reconstruction time as it requires only a single layer of the full-thickness purse-string suture. Also, only 1 patient developed clinically relevant POPF in the binding PG group despite the high fistula risk score of the included patients. In Binding PG, no sutures are taken to fix the pancreas with the stomach, which precludes the risk of suture cut through in the soft pancreas. Also, the portion of the pancreas through which stay sutures are taken is invaginated into the stomach. It ensures that a minor pancreatic leak from the needle entry site enters the gastric lumen rather than the peritoneal cavity. The clinically relevant POPF rate with the modified Blumgart technique was 28% in the present study. The grade B/C POPF rate with the Blumgart technique in open PD ranges from 2.5% to 20.5%[12-14,29,30]. Nagakawa et al[31] reported a Grade B/C POPF rate of 20% in their laparoscopic series using the modified Blumgart technique. The relatively high POPF rate in the present series could be due to the learning curve effect and inclusion of high fistula risk score patients.
In contrast to POPF, modified binding PG is associated with an increased incidence of intraluminal PPH. While most patients had Grade A or B PPH, surgical intervention was required in 1 patient. Also, seeing blood through the nasogastric gastric tube makes the patient anxious. Raw pancreatic stump lying freely in the gastric lumen without any compression effect of jejunum may be the reason for an increased incidence of intraluminal PPH. Hong et al[27] suggested that full-thickness suture closure of pancreatic stump can reduce the incidence of intraluminal PPH with binding PG. It is recommended to stent the pancreatic duct to avoid including it while taking the hemostatic sutures.
The choice of pancreatic reconstruction in both open and laparoscopic PD is determined by surgeon preference and familiarity with a particular technique. As binding PG is a technically more straightforward procedure, we used it in our initial patients who underwent PD. The increased incidence of intraluminal PPH was the primary reason for changing to modified Blumgart PJ. The present study results suggest that it may be preferable to start with a simpler technique of pancreatic reconstruction to reduce the POPF rate. Modified Binding PG with hemostatic pancreatic sutures on either side of the pancreatic duct may achieve the goal without increasing PPH. Alternatively, tailored pancreatic reconstruction with modified binding PG for patients with a high fistula risk score and modified Blumgart PJ for patients with low fistula risk score may be a reasonable approach during the learning curve of laparoscopic PD. While retrospective study design is the primary limitation of the current series, it is the first study to compare the perioperative outcomes of modified binding PG and modified Blumgart technique of PJ.
Modified Binding PG reduces the pancreatic reconstruction time and POPF rate during the learning curve of laparoscopic PD but is associated with increased intraluminal PPH compared to PJ using the modified Blumgart technique.
Complications related to pancreatico-enteric anastomosis are a significant cause of morbidity, especially during the learning curve in laparoscopic pancreaticoduodenectomy (PD). Despite multiple randomized controlled trials and meta-analyses, the type of pancreatico-enteric anastomosis [pancreaticojejunostomy (PJ) vs pancreaticogastrostomy(PG)] as a risk factor for post-pancreatectomy complications is debatable.
The ideal technique of pancreatic reconstruction during the learning curve of laparoscopic PD has not been well studied.
To compare the short-term outcomes of modified binding PG and Blumgart technique of PJ for pancreatic reconstruction in laparoscopic PD during the learning curve.
The first 25 patients with resectable pancreatic or periampullary tumors who underwent laparoscopic PD and pancreatic reconstruction with modified binding PG or Blumgart PJ between January 2015 and May 2020 were retrospectively analyzed. A single layer of the full-thickness purse-string suture was placed around the posterior gastrotomy in the modified binding PG. In the modified Blumgart technique, a total of two transpancreatic horizontal mattress sutures were placed on either side of the pancreatic duct to secure the pancreatic parenchyma to the jejunum. Also, on the ventral surface, the knot is tied to the jejunal wall without going through the pancreatic parenchyma. Post pancreatectomy complications are graded as per the International Study Group for Pancreatic Surgery criteria and compared to evaluate perioperative outcomes during the same learning curve.
The demographic and clinical parameters of the patients included in both groups were comparable. The median operative time for pancreatic reconstruction was significantly lower in the binding PG group (42 vs 58 min, P = 0.01). The clinically relevant (Grade B/C) postoperative pancreatic fistula (POPF) was significantly more in the modified PJ group (28% vs 4%, P = 0.04). In contrast, intraluminal postpancreatectomy hemorrhage (PPH) was more in the binding PG group (32% vs 4%, P = 0.02). There was no significant difference in the incidence of delayed gastric emptying between the two groups.
Modified binding PG reduces the pancreatic reconstruction time and POPF rate during the learning curve of laparoscopic PD but is associated with increased intraluminal PPH compared to PJ using the modified Blumgart technique.
Modified Binding PG combined with techniques to reduce PPH like hemostatic pancreatic sutures on either side of the pancreatic duct may reduce POPF without increasing PPH during the learning curve of laparoscopic PD. A tailored pancreatic reconstruction with modified binding PG for patients with a high fistula risk score and modified Blumgart PJ for patients with low fistula risk score may be a reasonable approach during the learning curve of laparoscopic PD.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: International Hepato-Pancreato Biliary Association, M02056.
Specialty type: Oncology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bencini L, Italy; Fernández-Placencia RM, Peru S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | Palanivelu C, Senthilnathan P, Sabnis SC, Babu NS, Srivatsan Gurumurthy S, Anand Vijai N, Nalankilli VP, Praveen Raj P, Parthasarathy R, Rajapandian S. Randomized clinical trial of laparoscopic vs open pancreatoduodenectomy for periampullary tumours. Br J Surg. 2017;104:1443-1450. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 241] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 2. | Wang M, Li D, Chen R, Huang X, Li J, Liu Y, Liu J, Cheng W, Chen X, Zhao W, Tan Z, Huang H, Zhu F, Qin T, Ma J, Yu G, Zhou B, Zheng S, Tang Y, Han W, Meng L, Ke J, Feng F, Chen B, Yin X, Chen W, Ma H, Xu J, Lin R, Dong Y, Yu Y, Zhang H, Qin R; Minimally Invasive Treatment Group in the Pancreatic Disease Branch of China's International Exchange and Promotion Association for Medicine and Healthcare (MITG-P-CPAM). Laparoscopic vs open pancreatoduodenectomy for pancreatic or periampullary tumours: a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol. 2021;6:438-447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 96] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 3. | Sun R, Yu J, Zhang Y, Liang Z, Han X. Perioperative and oncological outcomes following minimally invasive vs open pancreaticoduodenectomy for pancreatic duct adenocarcinoma. Surg Endosc. 2021;35:2273-2285. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | Tzeng CW, Katz MH, Fleming JB, Lee JE, Pisters PW, Holmes HM, Varadhachary GR, Wolff RA, Abbruzzese JL, Vauthey JN, Aloia TA. Morbidity and mortality after pancreaticoduodenectomy in patients with borderline resectable type C clinical classification. J Gastrointest Surg. 2014;18:146-155; discussion 155. [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Menahem B, Guittet L, Mulliri A, Alves A, Lubrano J. Pancreaticogastrostomy is superior to pancreaticojejunostomy for prevention of pancreatic fistula after pancreaticoduodenectomy: an updated meta-analysis of randomized controlled trials. Ann Surg. 2015;261:882-887. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 104] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 6. | Qin H, Luo L, Zhu Z, Huang J. Pancreaticogastrostomy has advantages over pancreaticojejunostomy on pancreatic fistula after pancreaticoduodenectomy. A meta-analysis of randomized controlled trials. Int J Surg. 2016;36:18-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Li Y, Hua R. The optimal choice for pancreatic anastomosis after pancreaticoduodenectomy: a network meta-analysis. Minerva Surg. 2021;In press. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Ratnayake CBB, Wells CI, Kamarajah SK, Loveday B, Sen G, French JJ, White S, Pandanaboyana S. Critical appraisal of the techniques of pancreatic anastomosis following pancreaticoduodenectomy: A network meta-analysis. Int J Surg. 2020;73:72-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Kang CM, Lee SH, Chung MJ, Hwang HK, Lee WJ. Laparoscopic pancreatic reconstruction technique following laparoscopic pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2015;22:202-210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Peng SY, Wang JW, Hong DF, Liu YB, Wang YF. Binding pancreaticoenteric anastomosis: from binding pancreaticojejunostomy to binding pancreaticogastrostomy. Updates Surg. 2011;63:69-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Routh D, Pathak N, Naidu CS, Singh AK, Rao PP, Ranjan P. A study on outcome of binding pancreaticogastrostomy following pancreaticoduodenectomy: A prospective observational study. Int J Surg. 2018;50:104-109. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Fujii T, Sugimoto H, Yamada S, Kanda M, Suenaga M, Takami H, Hattori M, Inokawa Y, Nomoto S, Fujiwara M, Kodera Y. Modified Blumgart anastomosis for pancreaticojejunostomy: technical improvement in matched historical control study. J Gastrointest Surg. 2014;18:1108-1115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 120] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 13. | Mishra PK, Saluja SS, Gupta M, Rajalingam R, Pattnaik P. Blumgart's technique of pancreaticojejunostomy: an appraisal. Dig Surg. 2011;28:281-287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Hirono S, Kawai M, Okada KI, Miyazawa M, Kitahata Y, Hayami S, Ueno M, Yamaue H. Modified Blumgart Mattress Suture Versus Conventional Interrupted Suture in Pancreaticojejunostomy During Pancreaticoduodenectomy: Randomized Controlled Trial. Ann Surg. 2019;269:243-251. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 15. | Hong D, Xin Y, Cai X, Peng S. Application of binding pancreatogastrostomy in laparoscopic central pancreatectomy. World J Surg Oncol. 2012;10:223. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Brennan M. Pancreaticojejunostomy. In: Blumgart LH, Fong Y, editors. Surgery of the liver and biliary tract, 3rd edition. Philadelphia: Saunders, 2000: 1073-1089. [DOI] [Cited in This Article: ] |
| 17. | Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 2013;216:1-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 653] [Cited by in F6Publishing: 796] [Article Influence: 66.3] [Reference Citation Analysis (0)] |
| 18. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [DOI] [Cited in This Article: ] [Cited by in Crossref: 18532] [Cited by in F6Publishing: 21934] [Article Influence: 1096.7] [Reference Citation Analysis (0)] |
| 19. | Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M; International Study Group on Pancreatic Surgery (ISGPS). The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161:584-591. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2435] [Cited by in F6Publishing: 2375] [Article Influence: 339.3] [Reference Citation Analysis (1)] |
| 20. | Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761-768. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1771] [Cited by in F6Publishing: 2043] [Article Influence: 120.2] [Reference Citation Analysis (0)] |
| 21. | Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20-25. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1411] [Cited by in F6Publishing: 1660] [Article Influence: 97.6] [Reference Citation Analysis (0)] |
| 22. | van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, Gerhards MF, de Hingh IH, Karsten TM, Lips DJ, Luyer MD, Busch OR, Festen S, Besselink MG; Dutch Pancreatic Cancer Group. Laparoscopic vs open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol. 2019;4:199-207. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 242] [Cited by in F6Publishing: 334] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 23. | Kim H, Choi HZ, Kang BM, Lee JW. Learning Curve in Laparoscopic Pancreaticoduodenectomy: Using Risk-Adjusted Cumulative Summation Methods. J Laparoendosc Adv Surg Tech A. 2021;In press. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Lu C, Jin W, Mou YP, Zhou J, Xu X, Xia T, Zhang R, Zhou Y, Yan J, Huang C, Zhang B, Wang J. Analysis of learning curve for laparoscopic pancreaticoduodenectomy. J Vis Surg. 2016;2:145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 25. | Wang M, Meng L, Cai Y, Li Y, Wang X, Zhang Z, Peng B. Learning Curve for Laparoscopic Pancreaticoduodenectomy: a CUSUM Analysis. J Gastrointest Surg. 2016;20:924-935. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 97] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 26. | Peng SY, Wang JW, Li JT, Mou YP, Liu YB, Cai XJ. Binding pancreaticojejunostomy--a safe and reliable anastomosis procedure. HPB (Oxford). 2004;6:154-160. [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Wakabayashi T, Felli E, Pessaux P. Robotic Double Purse-String Telescoped Pancreaticogastrostomy: How I Do It. World J Surg. 2019;43:604-607. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Hong D, Liu Y, Peng S, Sun X, Wang Z, Cheng J, Shen G, Zhang Y, Huang D. Binding pancreaticogastrostomy in laparoscopic central pancreatectomy: a novel technique in laparoscopic pancreatic surgery. Surg Endosc. 2016;30:715-720. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Li Z, Wei A, Xia N, Zheng L, Yang D, Ye J, Xiong J, Hu W. Blumgart anastomosis reduces the incidence of pancreatic fistula after pancreaticoduodenectomy: a systematic review and meta-analysis. Sci Rep. 2020;10:17896. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Cao F, Tong X, Li A, Li J, Li F. Meta-analysis of modified Blumgart anastomosis and interrupted transpancreatic suture in pancreaticojejunostomy after pancreaticoduodenectomy. Asian J Surg. 2020;43:1056-1061. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Nagakawa Y, Takishita C, Hijikata Y, Osakabe H, Nishino H, Akashi M, Nakajima T, Shirota T, Sahara Y, Hosokawa Y, Ishizaki T, Katsumata K, Tsuchida A. Blumgart method using LAPRA-TY clips facilitates pancreaticojejunostomy in laparoscopic pancreaticoduodenectomy. Medicine (Baltimore). 2020;99:e19474. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |